Abstract
Objectives
This analysis sought to determine factors (including adiposity-related factors) most associated with HF-type symptoms (fatigue, shortness of breath, and edema) in adults with chronic kidney disease (CKD).
Background
Symptom burden impairs quality of life in CKD, especially symptoms that overlap with HF. These symptoms are common regardless of clinical HF diagnosis, and may be affected by subtle cardiac dysfunction, kidney dysfunction, and other factors. We used machine learning to investigate cross-sectional relationships of clinical variables with symptom scores in a CKD cohort.
Methods
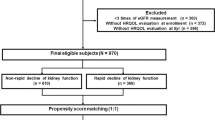
Participants in the Chronic Renal Insufficiency Cohort (CRIC) with a baseline modified Kansas City Cardiomyopathy Questionnaire (KCCQ) score were included, regardless of prior HF diagnosis. The primary outcome was Overall Summary Score as a continuous measure. Predictors were 99 clinical variables representing demographic, cardiac, kidney and other health dimensions. A correlation filter was applied. Random forest regression models were fitted. Variable importance scores and adjusted predicted outcomes are presented.
Results
The cohort included 3426 individuals, 10.3% with prior HF diagnosis. BMI was the most important factor, with BMI 24.3 kg/m2 associated with the least symptoms. Symptoms worsened with higher or lower BMIs, with a potentially clinically relevant 5 point score decline at 35.7 kg/m2 and a 1-point decline at the threshold for low BMI, 18.5 kg/m2. The most important cardiac and kidney factors were heart rate and eGFR, the 4th and 5th most important variables, respectively. Results were similar for secondary analyses.
Conclusions
In a CKD cohort, BMI was the most important feature for explaining HF-type symptoms regardless of clinical HF diagnosis, identifying an important focus for symptom directed investigations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data used for this study are available from the National Institute of Diabetes and Digestive and Kidney Diseases Central Repository: https://repository.niddk.nih.gov/studies/cric/.
References
Brown SA, Tyrer FC, Clarke AL, Lloyd-Davies LH, Stein AG, Tarrant C, et al. Symptom burden in patients with chronic kidney disease not requiring renal replacement therapy. Clinical Kidney J.2017;10:788–96.
Abdel-Kader K, Unruh ML, Weisbord SD. Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin J American Soc Nephrol: CJASN. 2009;4:1057–64.
Almutary H, Bonner A, Douglas C. Symptom burden in chronic kidney disease: A review of recent literature. J Ren Care. 2013;39:140–50.
House AA, Wanner C, Sarnak MJ, Piña IL, McIntyre CW, Komenda P, et al. Heart failure in chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;95:1304–17.
Park M, Hsu CY, Li Y, Mishra RK, Keane M, Rosas SE, et al. Associations between kidney function and subclinical cardiac abnormalities in CKD. J Am Soc Nephrol. 2012;23:1725–34.
Bansal N, Roy J, Chen H-Y, Deo R, Dobre M, Fischer MJ, et al. Evolution of echocardiographic measures of cardiac disease from CKD to ESRD and risk of all-cause mortality: Findings from the CRIC study. American J Kidney Dis. 2018;72:390–9.
Di Lullo L, Gorini A, Russo D, Santoboni A, Ronco C. Left ventricular hypertrophy in chronic kidney disease patients: from pathophysiology to treatment. Cardiorenal Med. 2015;5:254–66.
Zambroski CH, Moser DK, Bhat G, Ziegler C. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. Eur J Cardiovasc Nursing. 2005;4:198–206.
Spertus JA, Jones PG, Sandhu AT, Arnold SV. Interpreting the Kansas City Cardiomyopathy Questionnaire in Clinical Trials and Clinical Care: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;76:2379–90.
Shlipak MG, Lash JP, Yang W, Teal V, Keane M, Cappola T, et al. Symptoms characteristic of heart failure among CKD patients without diagnosed heart failure. J Cardiac Failure. 2011;17:17–23.
Mishra RK, Yang W, Roy J, Anderson AH, Bansal N, et al. Kansas City Cardiomyopathy Questionnaire Score Is Associated With Incident Heart Failure Hospitalization in Patients With Chronic Kidney Disease Without Previously Diagnosed Heart Failure: Chronic Renal Insufficiency Cohort Study. Circ Heart Fail. 2015;8:702–8.
Munger E, Choi H, Dey AK, Elnabawi YA, Groenendyk JW, Rodante J, et al. Application of machine learning to determine top predictors of noncalcified coronary burden in psoriasis: An observational cohort study. J Am Acad Dermatol. 2020;83:1647–53.
Munger E, Hickey JW, Dey AK, Jafri MS, Kinser JM, Mehta NN. Application of machine learning in understanding atherosclerosis: Emerging insights. APL Bioeng. 2021;5:011505
Chen X, Wang CC, Yin J, You ZH. Novel Human miRNA-Disease Association Inference Based on Random Forest. (2162-2531 (Print)).
Lash JP, Go AS, Appel LJ, He J, Ojo A, Rahman M, et al. Chronic Renal Insufficiency Cohort (CRIC) Study: Baseline Characteristics and Associations with Kidney Function. Clinical J American Soc Nephrol. 2009;4:1302
Feldman HI, Appel LJ, Chertow GM, Cifelli D, Cizman B, Daugirdas J, et al. The Chronic Renal Insufficiency Cohort (CRIC) Study: Design and Methods. J Am Soc Nephrol. 2003;14:S148–53.
Heidenreich PA, Spertus JA, Jones PG, Weintraub WS, Rumsfeld JS, Rathore SS, et al. Health status identifies heart failure outpatients at risk for hospitalization or death. J American College Cardiol. 2006;47:752–6.
Joseph SM, Novak E, Arnold SV, Jones PG, Khattak H, Platts AE, et al. Comparable performance of the Kansas City Cardiomyopathy Questionnaire in patients with heart failure with preserved and reduced ejection fraction. Circ: Heart Fail. 2013;6:1139–46.
Spertus JA, Jones PG. Development and validation of a short version of the Kansas City Cardiomyopathy Questionnaire. Circ: Cardiovasc Quality Outcomes. 2015;8:469–76.
Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35:1245–55.
U.S. Food and Drug Administration. Qualified Clinical Outcome Assessments (COA) Silver Spring, Maryland: Department of Health and Human Services; 2020 [updated 4/14/2020. Available from: https://www.fda.gov/drugs/clinical-outcome-assessment-coa-qualification-program/qualified-clinical-outcome-assessments-coa.
Kuhn M, Johnson K. Feature engineering and selection: A practical approach for predictive models: CRC Press; 2019.
Hastie T, Tibshirani R, Friedman J. The Elements of Statistical Learning. 2nd Edition, Corrected 12th Printing ed. New York, NY: Springer; 2017.
Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clin Psychological Sci. 2017;5:457–69.
Ambale-Venkatesh B, Yang X, Wu CO, Liu K, Hundley WG, McClelland R, et al. Cardiovascular Event Prediction by Machine Learning: The Multi-Ethnic Study of Atherosclerosis. Circ Res. 2017;121:1092–101.
Huynh-Thu VA, Saeys Y, Wehenkel L, Geurts P. Statistical interpretation of machine learning-based feature importance scores for biomarker discovery. Bioinformatics.2012;28:1766–74.
Biau G, Scornet E. A random forest guided tour. TEST. 2016;25:197–227.
Kuhn M, Johnson K. Applied Predictive Modeling. Corrected 5th Printing ed. New York, NY: Springer; 2016.
Liaw A, Wiener M. Classification and regression by randomForest. R news. 2002;2:18–22.
Gregg LP, Bossola M, Ostrosky-Frid M, Hedayati SS. Fatigue in CKD: Epidemiology, Pathophysiology, and Treatment. Clin J Am Soc Nephrol. 2021;16:1445–55.
Rumsfeld JS, Havranek E, Masoudi FA, Peterson ED, Jones P, Tooley JF, et al. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol. 2003;42:1811–7.
Resnick HE, Carter EA, Aloia M, Phillips B. Cross-sectional relationship of reported fatigue to obesity, diet, and physical activity: results from the third national health and nutrition examination survey. J Clin Sleep Med. 2006;2:163–9.
Lim W, Hong S, Nelesen R, Dimsdale JE. The association of obesity, cytokine levels, and depressive symptoms with diverse measures of fatigue in healthy subjects. Arch Internal Med. 2005;165:910–5.
Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metabol Care. 2011;14:402
Preiss K, Brennan L, Clarke D. A systematic review of variables associated with the relationship between obesity and depression. Obes Rev. 2013;14:906–18.
Mehta R. Impacts of obesity and stress on neuromuscular fatigue development and associated heart rate variability. Int J Obes. 2015;39:208–13.
Buras ED, Converso-Baran K, Davis CS, Akama T, Hikage F, Michele DE, et al. Fibro-adipogenic remodeling of the diaphragm in obesity-associated respiratory dysfunction. Diabetes.2019;68:45–56.
Brock JM, Billeter A, Müller-Stich BP, Herth F. Obesity and the Lung: What We Know Today. Respiration.2020;99:856–66.
Davies HO, Popplewell M, Singhal R, Smith N, Bradbury AW. Obesity and lower limb venous disease–The epidemic of phlebesity. Phlebology.2017;32:227–33.
Savetsky IL, Torrisi JS, Cuzzone DA, Ghanta S, Albano NJ, Gardenier JC, et al. Obesity increases inflammation and impairs lymphatic function in a mouse model of lymphedema. American J Physiol-Heart Circulatory Physiol. 2014;307:H165–72.
Kolotkin RL, Andersen JR. A systematic review of reviews: Exploring the relationship between obesity, weight loss and health‐related quality of life. Clin Obes. 2017;7:273–89.
Schweitzer ML, Stengel B, Legrand K, Briancon S, Jacquelinet C, Combe C, et al. Obesity phenotype and patient-reported outcomes in moderate and severe chronic kidney disease: A cross-sectional study from the CKD-REIN cohort study. Qual Life Res. 2019;28:1873–83.
Perlman RL, Finkelstein FO, Liu L, Roys E, Kiser M, Eisele G, et al. Quality of life in chronic kidney disease (CKD): A cross-sectional analysis in the Renal Research Institute-CKD study. Am J Kidney Dis. 2005;45:658–66.
Drüeke TB, Locatelli F, Clyne N, Eckardt K-U, Macdougall IC, Tsakiris D, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. New England J Med. 2006;355:2071–84.
Munafo MR, Tilling K, Taylor AE, Evans DM, Davey, Smith G. Collider scope: When selection bias can substantially influence observed associations. Int J Epidemiol. 2018;47:226–35.
Acknowledgements
Dr. Navaneethan is supported by research funding from the Department of Veterans Affairs Health Services Research & Development (1I01HX002917–01A1) and a grant from the National Institutes of Health (NIDDK-R01DK101500). Dr. Gregg is supported in part by the Center for Innovations in Quality, Effectiveness and Safety (CIN 13–413), Michael E. DeBakey VA Medical Center, Houston, TX.
Funding
Funding for this project was obtained through the CRIC Study Opportunity Pool Program. Funding for the CRIC Study was obtained under a cooperative agreement from National Institute of Diabetes and Digestive and Kidney Diseases (U01DK060990, U01DK060984, U01DK061022, U01DK061021, U01DK061028, U01DK060980, U01DK060963, U01DK060902 and U24DK060990). In addition, this work was supported in part by: the Perelman School of Medicine at the University of Pennsylvania Clinical and Translational Science Award NIH/NCATS UL1TR000003, Johns Hopkins University UL1 TR-000424, University of Maryland GCRC M01 RR-16500, Clinical and Translational Science Collaborative of Cleveland, UL1TR000439 from the National Center for Advancing Translational Sciences (NCATS) component of the National Institutes of Health and NIH roadmap for Medical Research, Michigan Institute for Clinical and Health Research (MICHR) UL1TR000433, University of Illinois at Chicago CTSA UL1RR029879, Tulane COBRE for Clinical and Translational Research in Cardiometabolic Diseases P20 GM109036, Kaiser Permanente NIH/NCRR UCSF-CTSI UL1 RR-024131, Department of Internal Medicine, University of New Mexico School of Medicine Albuquerque, NM R01DK119199.
Author information
Authors and Affiliations
Consortia
Contributions
CPW and SDN contributed to the research idea, study design, and data acquisition. CPW, JSB, LPG, NB, VN, HIF, MGS, and SDN contributed to the data analysis/interpretation. CPW performed the statistical analysis. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work.
Corresponding author
Ethics declarations
Competing interests
Dr. Walther reports consulting fees from GlaxoSmithKline. Dr. Navaneethan reports personal fees from Bayer, personal fees from Boehringer-Ingelheim, personal fees from REATA, personal fees from Tricida, and grants from Keryx, outside the submitted work. Dr. Nambi has a provisional patent along with Roche and Baylor College of Medicine for use of biomarkers in prediction of heart failure risk and was the site PI for studies sponsored by Merck and Amgen. Dr. Shlipak has reported consulting fees from Cricket Health and Intercept Pharmaceuticals.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or Veterans Administration.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Walther, C.P., Benoit, J.S., Gregg, L.P. et al. Heart failure-type symptom scores in chronic kidney disease: The importance of body mass index. Int J Obes 46, 1910–1917 (2022). https://doi.org/10.1038/s41366-022-01208-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01208-x