Abstract
Background/objectives
Patients affected by obesity and Coronavirus disease 2019, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), appear to have a higher risk for intensive care (ICU) admission. A state of low-grade chronic inflammation in obesity has been suggested as one of the underlying mechanisms. We investigated whether obesity is associated with differences in new inflammatory biomarkers mid-regional proadrenomedullin (MR-proADM), C-terminal proendothelin-1 (CT-proET-1), and clinical outcomes in critically ill patients with SARS-CoV-2 pneumonia.
Subjects/methods
A total of 105 critically ill patients with SARS-CoV-2 pneumonia were divided in patients with obesity (body mass index (BMI) ≥ 30 kg/m2, n = 42) and patients without obesity (BMI < 30 kg/m2, n = 63) and studied in a retrospective observational cohort study. MR-proADM, CT-proET-1 concentrations, and conventional markers of white blood count (WBC), C-reactive protein (CRP), and procalcitonin (PCT) were collected during the first 7 days.
Results
BMI was 33.5 (32–36.1) and 26.2 (24.7–27.8) kg/m2 in the group with and without obesity. There were no significant differences in concentrations MR-proADM, CT-proET-1, WBC, CRP, and PCT at baseline and the next 6 days between patients with and without obesity. Only MR-proADM changed significantly over time (p = 0.039). Also, BMI did not correlate with inflammatory biomarkers (MR-proADM rho = 0.150, p = 0.125, CT-proET-1 rho = 0.179, p = 0.067, WBC rho = −0.044, p = 0.654, CRP rho = 0.057, p = 0.564, PCT rho = 0.022, p = 0.842). Finally, no significant differences in time on a ventilator, ICU length of stay, and 28-day mortality between patients with or without obesity were observed.
Conclusions
In critically ill patients with confirmed SARS-CoV-2 pneumonia, obesity was not associated with differences in MR-proADM, and CT-proET-1, or impaired outcome.
Trial registration
Netherlands Trial Register, NL8460.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19), the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1, 2], has turned out to be an enormous challenge to intensive care units (ICU) worldwide [3,4,5]. A substantial part of the patients deteriorated quickly and needed to be admitted to the ICU with signs and symptoms consistent with acute respiratory failure and/or acute respiratory distress syndrome (ARDS). Age, male sex, hypertension, type 2 diabetes, and coronary artery disease were reported as risk factors for ICU admission in COVID-19 patients [1,2,3,4,5]. Also, the prevalence of obesity was high among COVID-19 patients admitted to the ICU [5, 6]. Moreover, the need for invasive mechanical ventilation was higher in COVID-19 patients with obesity admitted to the ICU [7, 8].
The potential pathophysiological mechanisms between SARS-CoV-2 infection and obesity are not yet fully understood. SARS-CoV-2 virus infection of the host, using the angiotensin-converting enzyme 2 (ACE2) receptor, is one of the proposed mechanisms in COVID-19 [9]. The ACE2 receptors are highly expressed by adipocytes of patients affected by obesity and type 2 diabetes [10]. The adipose tissue may serve as a reservoir for the virus and excrete the virus over a long period, resulting in a continuous augmented inflammatory response [10].
Cytokines were measured to observe the inflammatory response in a prospective observational cohort study with 67 COVID-19 ICU patients [11]. There were no differences in cytokine response between ICU patients with and without obesity. But, as cytokines have a short half-life and can therefore only be measured during a short period, there may be a role for more stable biomarkers as a measure of inflammation. There were no differences in conventional inflammatory biomarkers white blood count (WBC), C-reactive protein (CRP), and procalcitonin (PCT) in this observational study [11]. As virus-induced endothelial dysfunction and damage, endotheliitis, has been proposed as one of the potential mechanisms of COVID-19 [12, 13], there may be a role for endothelium-related inflammatory biomarkers mid-regional proadrenomedullin (MR-proADM) and C-terminal proendothelin-1 (CT-proET-1). MR-proADM and CT-proET-1 are the precursor fragments of the prohormones of adrenomedullin (ADM) and endothelin-1 (ET-1) [14, 15]. The precursor fragments are more stable and therefore measuring the fragments is more feasible for clinical purposes. ADM is a peptide generated by endothelial and vascular smooth muscle cells, with anti-inflammatory effects on vascular endothelial cells, protecting the microcirculation against endothelial permeability in sepsis [16, 17]. ADM is also an adipokine, a pro-inflammatory cytokine released by adipose tissue [18]. ET-1 is a strong vasoconstrictor peptide and pro-inflammatory cytokine that is released from activated endothelial cells [19]. Patients with obesity showed increased vascular expression of ET-1 and vasoconstriction activity [20, 21].
The primary aim of the present study was to investigate whether obesity was associated with differences in endothelium and obesity-related inflammatory biomarkers MR-proADM and CT-proET-1 in critically ill patients with SARS-CoV-2 pneumonia. The secondary aim was the association between obesity and clinical outcome (time on a ventilator, ICU length of stay (LOS), and 28-day mortality).
Materials/subjects and methods
Study design and selection criteria
This single-center observational cohort study is a secondary analysis of a prospective observational biomarker study [22], in which patients were enrolled with confirmed SARS-CoV-2 pneumonia, and admitted to the ICU of the Elisabeth Tweesteden Hospital (Tilburg Netherlands) from March 11 until May 27, 2020. All clinical data, microbiological and laboratory results, including MR-proADM and CT-proET-1, were prospectively collected during this period. The study protocol was approved by the METC Brabant (Medisch Ethische Toetsingscommissie Brabant) (Tilburg, Netherlands) (NW 2020–86). Informed consent was received from all participating patients. Inclusion criteria were adults ≥18 years of age, admitted to the ICU with pneumonia and SARS-CoV-2 infection confirmed by real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay of nasopharyngeal or bronchial swabs. Patients who did not meet the inclusion criteria or without informed consent were excluded. Both severe and critical type diseases defined by the World Health Organization (WHO) interim guidance were included. Severe disease; severe pneumonia was designated when the patients had clinical signs of pneumonia (fever, cough, dyspnea, fast breathing) plus one of the following symptoms or physiological signs: respiratory rate >30 breaths/min, severe respiratory distress, or SpO2 < 90% on room air. Chest imaging (radiograph, CT scan, or lung ultrasound) may assist in diagnosis and identifying or excluding pulmonary complications [23]. Critical disease: ARDS was designated when the symptoms of pneumonia lasted less than 1 week or when there were new or worsening symptoms, chest imaging showed bilateral ground-glass lobar opacities, lobar or lung collapse, or nodules, and respiratory failure could not be solely explained by cardiac failure or fluid overload. In addition, signs of oxygenation impairment (PaO2/FiO2 ≤ 300 mmHg with positive end expiratory pressure ≥5 cmH2O or continuous positive airway pressure ≥5 cmH2O) needed to be present [23]. The included patients were divided into two categories: (1) patients with obesity (body mass index (BMI) ≥30 kg/m2) and (2) without obesity (BMI < 30 kg/m2) according to the classification by the WHO [24]. All patients received selective decontamination of the digestive tract, as described in previous publications [25]. Prophylactic antibiotics were given during the first 4 days to all patients as part of this decontamination strategy. STROBE (Strengthening the Reporting of Observational Studies in Epidemiology Statement) guidelines for reporting observational studies were followed [26].
Procedures
For clinical purposes, serial values of conventional biomarkers WBC, CRP, and PCT were collected on a daily basis in patients enrolled in the study. Additional blood samples were collected into EDTA tubes on a daily basis for 7 days, or until discharge or death. Plasma was separated by centrifugation and stored in aliquots at −80 °C. MR-proADM and CT-pro-ET-1 concentrations were measured using an automated immunofluorescent sandwich assay on a B.R.A.H.M.S. Kryptor Compact Plus analyzer (Thermo Fisher Scientific, Hennigsdorf, Germany) at the central diagnostic laboratory in Maastricht, the Netherlands. The Kryptor measures the signal that is emitted from an immunocomplex by time-resolved amplified cryptate emission. MR-proADM and CT-proET-1 assays have a limit of detection of 0.05 nmol/L and 2.94 pmol/L. The functional sensitivity (lowest value with an interassay coefficient of variation (CV) <20% as described by the manufacturer) of 0.25 nmol/L (MR-proADM) and 9.78 pmol/L (CT-proET-1), respectively. Imprecision of the assays was verified according to the Clinical & Laboratory Standards Institute Evaluation Protocol 17-A (CLSI EP17-A), using a low and high sample, measured for 5 days in triplicate. Intra and Inter CV values were all ≤10% for MR-proADM and CT-proET-1.
Statistical analysis
All non-normally distributed data (Kolmogorov–Smirnov test p < 0.05) will be expressed as median (with interquartile range, IQR) or as a number of patients (percentage) where appropriate. Patient characteristics and outcomes will be compared using a Mann–Whitney U test for continuous variables and chi-square test for categorical variables. To analyze the time course of biomarker profiles a linear mixed model for repeated measures with time and obesity as independent factors was used. Testing for interaction was performed. Individual BMI values were correlated with biomarker concentrations. The time on a ventilator, LOS intensive care, and cumulative survival will be analyzed by applying the Kaplan–Meier curves and differences will be compared with the log-rank test. Patients who died in the hospital or those who were still in the ICU and/or receiving mechanical ventilation on day 28 were censored on day 29 for the analysis of time on mechanical ventilation and ICU LOS. Patients who were discharged alive from the hospital or were still in the ICU or hospital on day 28 were censored on day 29 for the mortality analysis. We assessed the proportional hazards assumption in time on the ventilator, LOS ICU, and 28-day survival analysis using Schoenfeld residuals. The proportional hazards assumption was not violated (all p values >0.30). All tests are two-sided and a p value <0.05 was considered statistically significant. All data are analyzed using a statistical software package (SPSS Inc., version 24, Chicago, IL, USA).
Results
Characteristics of the patients
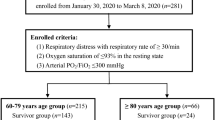
We selected a cohort of 133 critically ill patients with suspected SARS-CoV-2 pneumonia during the study period. In 105 patients, SARS-CoV-2 was confirmed by RT-PCR, informed consent was achieved and MR-proADM, CT-proET-1, WBC, CRP, and PCT concentrations were measured on day 1 and subsequent days. The patient flow diagram shows the flow of patients with and without obesity along with the endpoint of 28-day survival (Supplementary Fig. 1). Fifty-five (52.4%) patients were transferred to another ICU to distribute COVID-19 patients equally over the country. Median ICU time before transfer to another ICU was 3 days (IQR 2–5).
Demographics and clinical characteristics of the 105 selected patients are shown in Table 1. Twenty-three (22%) patients had severe disease and 82 (78%) had a critical disease, i.e., ARDS, 12 (11%) had mild ARDS, 51 (49%) moderate ARDS, and 19 (18%) severe ARDS according to the Berlin definition [27]. There was a low number of bacterial and fungal coinfections. Gram-positive bacterial microorganisms were found in nine patients (Enterococcus spp n = 5, Streptococcus pneumonia n = 3, Staphylococcus aureus n = 1). Gram-negative bacterial microorganisms were found in six patients (Pseudomonas aeruginosa n = 2, Legionella spp. n = 1, Enterobacter spp. n = 1, Bacteroides fragilis n = 1, Stenotrophomonas maltophilia n = 1). Aspergillus fumigatus was found in deep respiratory tract secretions in seven patients.
Patients were divided in two categories: patients with obesity, n = 42, of which 26.6% with class I obesity (BMI 30–34.99), 8.6% with class II (BMI 35–39.99), and 4.8% with class III obesity (BMI ≥ 40) [24] and patients without obesity, n = 63, 19% with normal weight (BMI 18.50–24.99), and 41% overweight (BMI 25–29.99) [24] (Supplementary Fig. 2). Both groups were comparable except for age and BMI.
Association biomarkers and obesity
There were no significant differences in plasma concentrations inflammatory biomarkers at ICU admission between patients with and without obesity (p < 0.05 for all biomarkers) (Table 1). Despite lower values of WBC and CRP in patients with obesity at all the timepoints, there were no significant differences in concentrations MR-proADM, CT-proET-1, WBC, CRP, and PCT at baseline and the next 6 days between patients with and without obesity (Fig. 1a–e). Only MR-proADM changed significantly over time (p = 0.039). Furthermore, BMI did not correlate with concentrations MR-proADM, CT-proET-1, WBC, CRP, and PCT, at ICU admission (rho = 0.150 (p = 0.125), rho = 0.179 (p = 0.067), rho = −0.044 (p = 0.654), rho = 0.057 (p = 0.564), rho = 0.022 (p = 0.842), respectively) (Supplementary Fig. 3a–e).
a Temporal changes in WBC. Median values with IQR. WBC was non-significant different between patients with obesity and without obesity (p = 0.375) and non-significant over time (p = 0.302). b Temporal changes in CRP. Median values with IQR. CRP was non-significant different between patients with obesity and without obesity (p = 0.401) and non-significant over time (p = 0.461). c Temporal changes in PCT. Median values with IQR. PCT was non-significant different between patients with obesity and without obesity (p = 0.945) and non-significant over time (p = 0.504). d Temporal changes in MR-proADM. Median values with IQR. MR-proADM was non-significant different between patients with obesity and without obesity (p = 0.121) and significant over time (p = 0.039). e Temporal changes in CT-proET-1. Median values with IQR. CT-proET-1 was non-significant different between patients with obesity and without obesity (p = 0.074) and non-significant over time (p = 0.273).
Clinical outcomes
On day 28 of ICU admission, 9 (23%) of the patients with obesity were still mechanically ventilated and 13 (31%) were still in the ICU, while 11 (19%) of the patients without obesity were still mechanically ventilated and 20 (32%) were still in the ICU (p = 0.594, p = 0.932, respectively). Time on the ventilator was 14 days (IQR 9–27) in patients with obesity and 18 days (IQR 9–26) in patients without obesity (log-rank p = 0.992). ICU LOS was 14 days (IQR 10–33) in patients with obesity and 20 days (10–32) in patients without obesity (log-rank p = 0.671). There was no significant difference in 28-day mortality between both groups, 31% versus 27%, log-rank p = 0.570. The Kaplan–Meier curves for time on mechanical ventilation, ICU LOS, and 28-day mortality are presented in Supplementary Fig. 4a–c.
Discussion
The primary aim of the study was to investigate whether obesity was associated with differences in endothelium and obesity-related inflammatory biomarkers MR-proADM and CT-proET-1 in a well-described cohort of critically ill patients with SARS-CoV-2 pneumonia. Secondary outcomes were the association between obesity and time on a ventilator, ICU LOS, and 28-day mortality. We reported two main findings. First, obesity was not related to different responses in MR-proADM and CT-proET-1. Secondly, we found no relationship between obesity and clinical outcome. What our study adds pertaining to the role of obesity in critically ill patients with SARS-CoV-2 pneumonia are data of inflammatory biomarkers MR-proADM and CT-proET-1 during the first 7 days of ICU admission.
Worldwide changes in lifestyle, consumer markets, and urbanization are important causes of a high prevalence of obesity, especially in western countries [28]. Patients affected by obesity have an increased risk of developing type 2 diabetes mellitus, hypertension, and dyslipidemia [28, 29]. It is no surprise that obesity has a high impact on health care providers [28]. Obesity was found to be an independent risk factor for ICU admission and mortality during the H1N1 pandemic 10 years ago [30]. Two single-center studies showed a high prevalence of patients affected by obesity and severe obesity in patients with SARS-CoV-2 in need of invasive mechanical ventilation [7, 8]. Mortality doubled among different classes of obesity in patients hospitalized with SARS-CoV-2 infection in a multicenter prospective cohort study with 5795 hospitalized patients [31]. The present study is a secondary analysis of a prospective observational biomarker study, in which 105 critically ill patients with confirmed SARS-CoV-2 pneumonia were enrolled [22]. Baseline MR-proADM ≥ 1.57 nmol/L and CT-proET-1 ≥ 111 pmol/L were significant predictors of 28-day mortality for all 105 patients in multivariable Cox regression models adjusted for age and SOFA score (HR 6.80, 95% CI 3.12–14.84, p < 0.001 and HR 3.72, 95% CI 1.71–8.08, p = 0.01). The value of MR-proADM as a prognostic marker in adult patients hospitalized with SARS-CoV-2 infection was studied in several other observational studies [32,33,34,35,36,37]. Increased levels of MR-proADM were independently associated with mortality [32,33,34,35,36,37]. However, none of these studies investigated whether obesity was associated with differences in MR-proADM. Obesity was associated with lower 6-year mortality and higher MR-proADM levels in non-COVID-19 community-acquired pneumonia patients in a secondary analysis of the ProHosp Trial [38]. The baseline median MR-proADM level was 1.21 nmol/L (IQR 0.81–1.88), but no details of the number of patients admitted to the ICU were reported. MR-proADM levels were measured in a cohort of 153 critically ill patients with presumed bacterial pneumonia [39]. Median baseline MR-proADM levels were significantly higher compared with the SARS-CoV-2 cohort, 1.32 nmol/L (IQR 0.91–2.45) vs 1.16 nmol/L (0.86–1.71), p = 0.015. However, median APACHE IV scores of the bacterial pneumonia cohort were also significantly higher compared with the SARS-CoV-2 cohort, 73 (IQR 53–86) vs 47 (40–59), p < 0.001. Increased levels of CT-pro-ET-1 were independently associated with mortality in critically ill patients with SARS-CoV-2 pneumonia in one observational cohort study [22], but without differences in BMI classes. Epidemiologic studies in non-COVID-19 critically ill patients have shown beneficial effects of higher BMI on mortality in hospitalized patients with specific disease conditions. It has been observed in chronic diseases such as heart failure, coronary artery disease, sepsis, ARDS, or critical illness in general [40,41,42]. A phenomenon called the “obesity paradox” [40,41,42,43]. The existence of the obesity paradox has been challenged [40, 43]. The J-shaped relationship between BMI and outcome may result from increased mortality at the extremes on both sides (underweight and severe obesity). Moderate obesity may reflect relatively good health. The paradoxical association may be mediated by confounding variables. Patients with obesity might be admitted to the ICU at a lower level of severity or because of different admission criteria, due to difficulties in providing adequate care in the ward setting or to avoid possible complications [40]. High-risk patients with obesity and comorbidities may have already died before hospital admission, a phenomenon called “selective survivor” effect [44]. On the other hand, the obesity paradox is increasingly adopted [40, 41]. Several mechanisms have been proposed. Patients with obesity have higher metabolic reserves [40, 41]. An activated renin-angiotensin system in obesity may have protective hemodynamic effects in critically ill patients due to decreased need for fluid or vasopressor support [41]. Obesity may constitute to a status of low-grade chronic inflammation, which protects against the detrimental effects of an aggressive second hit during critical illness [40,41,42]. Conflicting data on the obesity paradox in critically ill patients are reported in different studies. The relationship between obesity and in-hospital mortality was analyzed in 222 critically ill COVID-19 patients with respiratory failure in a French observational cohort study [45]. Patients with moderate obesity (defined as BMI 30–39.9 kg/m2) had a lower risk of death than patients with normal weight, overweight or severe obesity, suggesting a possible obesity paradox. We could not detect significant differences in 28-day mortality between patients with and without obesity in our smaller study, as previously reported [46]. Our findings are in line with a much larger Dutch multicenter observational cohort study with 2635 COVID-19 patients admitted to the ICU [47].
Regarding the pathophysiology, the relation between SARS-CoV-2 and obesity might be explained by a state of low-grade chronic inflammation, associated with obesity [40, 48, 49]. Adipose tissue is considered to be more than a long-term energy storage organ [49]. Pro-inflammatory adipokines, released by adipocytes, are thought to play a crucial role in the pathogenesis of obesity and related adverse outcome [40, 48, 49]. Studies have shown increased plasma levels of leptin, tumor necrosis factor-alpha (TNF-α), interleukin-1 and 6 (IL-1, IL-6), reactive oxygen species, and ADM, leading to a dysregulated chronic immune response, which disrupt vascular homeostasis and contribute to endothelial dysfunction and damage in patients affected by obesity [18, 48,49,50,51]. Evidence of diffuse endothelial inflammation was also found in post-mortem analysis of COVID-19 patients [13]. ADM is a peptide hormone, produced by endothelial, vascular smooth muscle cells, and adipose tissue due to pro-inflammatory cytokines, bacterial toxins, hypoxia, or volume overload. ADM binds to receptors in especially cardiovascular and pulmonary tissues and has anti-inflammatory effects on vascular endothelial cells, stabilizing the endothelial barrier function and protecting the microcirculation against permeability in sepsis [16, 17]. Besides its action on the endothelium ADM has important effects on the vascular system, ADM reduces vasoconstriction through inhibition of the renin-angiotensin-aldosterone system [16, 52]. ET-1 is released from activated endothelial cells. It is a strong vasoconstrictor peptide and pro-inflammatory cytokine [19]. Patients with obesity showed increased vascular expression of ET-1 and vasoconstriction activity [20, 21]. ET-1 release is stimulated by bacterial toxins and inflammatory cytokines such as TNF-α or IL-6 [53]. MR-proADM and CT-proET-1 are the more stable precursor fragments of the prohormones that correlate with the release of the active peptides [14, 15]. In addition, there are studies showing a positive association between obesity and MR-proADM [50, 51, 54]. BMI correlated significantly to plasma MR-proADM (r = 0.714, p < 0.001) in a cohort of 357 subjects in a study reported by Vila et al. [50]. We could not detect any correlation between BMI and MR-proADM and there were no significant differences in MR-proADM between patients with and without obesity at baseline and the next days. Lower MR-proADM values, median 0.39 nmol/L (IQR 0.33–0.45) and median 0.41 nmol/L (IQR 0.23–0.64), were reported in reference populations of healthy individuals [55, 56]. We measured higher baseline median values in our cohort of critically ill patients with SARS-CoV-2 pneumonia. A state of hyper-inflammation in all SARS-CoV-2 patients, as illustrated by high baseline CRP values could be a possible explanation for higher baseline MR-proADM values. Moreover, we found no differences in MR-proADM levels between SARS-CoV-2 patients with and without obesity, but 68% of the patients in the non-obese group had overweight and only 32% had normal weight. A negative association between CT-proET-1 and obesity was observed in human participants in an observational cohort study of 8592 participants [54] and lower levels of endothelin-1 were found in mice with obesity in an animal model [57]. We could not detect any significant differences in CT-proET-1, at baseline and the next 6 days, in patients with and without obesity. Again, due to hyper-inflammation in critically ill patients with SARS-CoV-2 pneumonia. It appears that the pathophysiological influences of obesity and COVID-19 comprise multifactorial mechanisms, which are still not fully understood.
Some limitations of our study need to be addressed. First, this was a small retrospective observational single-center study in which results are hypothesis generating, but no direct cause-and-effect relationship can be deduced. Second, all clinical, microbiological, and laboratory data were prospectively collected between March 11 and May 27, 2020, which was the first period of the COVID-19 pandemic in the Netherlands. The treatment of COVID-19 has changed during the last year. Treatment with Chloroquine and Lopinavir/Ritonavir is obsolete and none of these patients were treated with dexamethasone during the first 10 days of hospitalization or IL-6 receptor antagonists. We must rely on older data of clinical practice leading to potential observational bias. Third, by only investigating ICU patients we may have introduced selection and collider bias between SARS-CoV-2 infection and adiposity [58]. Fourth, plasma samples could not be collected for 7 days in all patients due to early ICU discharge, transfer to another ICU, or early death. Incomplete longitudinal biomarker data might result in withdrawal bias. Fifth, the group of patients with obesity consisted largely of patients with class I obesity, and only a low number of patients had a BMI above 40 kg/m2. Again, selection bias needs to be taken into account. Both observation, selection, collider, and withdrawal bias may have led to potential underestimation of the association between obesity and the biomarkers MR-proADM and CT-proET-1.
Conclusions
Obesity was not associated with differences in new endothelium and obesity-related MR-proADM, CT-proET-1, and conventional inflammatory biomarkers in critically ill patients with confirmed SARS-CoV-2 pneumonia. We found no relation between obesity, time on the ventilator, ICU LOS, and 28-day mortality.
Data availability
Data collected for the study, including deidentified participant data and related documents, including the protocol, and informed consent form, will be made available to researchers after the publication of the manuscript upon reasonable request via application to the corresponding author.
References
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62.
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–81.
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323:1574–81.
Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. COVID-19 in critically ill patients in the Seattle region – case series. N Engl J Med. 2020;382:2012–22.
Gupta S, Hayek SS, Wang W, Chan L, Mathews KS, Melamed M, et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020;180:1436–47.
Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, et al. High prevalence of obesity in severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. 2020;28:1195–9.
Caussy C, Wallet F, Laville M, Disse E. Obesity is associated with severe forms of COVID-19. Obesity. 2020;28:1175.
Ni W, Yang X, Yang D, Bao J, Li R, Xiao Y, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;24:422.
Kruglikov IL, Scherer PE. The role of adipocytes and adipocyte-like cells in the severity of COVI-19 infections. Obesity. 2020;28:1187–90.
Kooistra EJ, de Nooijer AH, Claassen WJ, Grondman I, Janssen NAF, Netea MG, et al. A higher BMI is not associated with a different immune response and disease course in critically ill COVID-19 patients. Int J Obes. 2021;45:687–94.
Wilson DC, Schefold JC, Baldirà J, Spinetti T, Saeed K, Elke G. Andrenomedullin in COVID-19 induced endotheliitis. Crit Care. 2020;24:411.
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Andermatt R, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–8.
Struck J, Tao C, Morgenthaler NG, Bergman A. Identification of an adrenomedullin precursor fragment in plasma of sepsis patients. Peptides. 2004;25:1369–72.
Papassotiriou J, Morgenthaler NG, Struck J, Alanso C, Bergmann A. Immunoluminometric assay for measurement of the C-terminal Endothelin-1 precursor fragment in human plasma. Clin Chem. 2006;52:1144–51.
Temmesfeld-Wollbrück B, Hocke AC, Suttorp N, Hippenstiel S. Adrenomedullin and endothelial barrier function. Thromb Haemost. 2007;98:944–51.
Temmesfeld-Wollbrück B, Brell B, Dávid I, Dorenberg M, Adolphs J, Schmeck B, et al. Adrenomedullin reduces vascular hyperpermeability and improves survival in rat septic shock. Intensive Care Med. 2007;33:703–10.
Li Y, Jiang C, Wang X, Zhang Y, Shibahara S, Takahashi K, et al. Andrenomedullin is a novel adipokine: adrenomedullin in adipocytes and adipose tissues. Peptides. 2007;28:1129–43.
Teder P, Noble P. A cytokine reborn? Endothelin-1 in pulmonary inflammation and fibrosis. Am J Cell and Mol Biol. 2000;23:7–10.
Weil BR, Westby CM, Van Guilder GP, Greiner JJ, Stauffer BL, DeSouza CA. Enhanced endothelin-1 system activity with overweight and obesity. Am J Physiol Heart Circ Physiol. 2011;301:H689–H695.
Engin A. Endothelial dysfunction in obesity. Adv Exp Med Biol. 2017;960:345–79.
Van Oers JAH, Kluiters Y, Bons JAP, de Jongh M, Pouwels S, Ramnarain D, et al. Endothelium-associated biomarkers mid-regional proadrenomedullin and C-terminal proendothelin-1 have good ability to predict 28-day mortality in critically ill patients with SARS-C0V-2 pneumonia: a prospective cohort study. J Crit Care. 2021;66:173–89.
WHO. Clinical management of COVID-19. May 27. 2020. https://www.who.int/publications/i/item/clinical-management-of-covid-19. Accessed 11 Jan 2021.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253.
De Smet AM, Kluytmans JA, Cooper BS, Mascini EM, Benus RF, van der Werf TS, et al. Decontamination of the digestive tract and oropharynx in ICU patients. N Engl J Med. 2009;360:20–31.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296.
ARDS Definition Task Force Ranieri VM, Rubensfeld GD, Thompson BT, Ferguson ND, Caldwell E. et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–33.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Appachi S, Kelly KR, Schauer PR, Kirwan JP, Hazen S, Gupta M, et al. Reduced cardiovascular risk following bariatric surgeries is related to a partial recovery from adiposopathy. Obes Surg. 2011;21:1928–36.
Fezeu L, Julia C, Henegar A, Bitu J, Hu FB, Grobbee DE, et al. Obesity is associated with higher risk of intensive care unit admission and death in influenza A (H1N1) patients: a systematic review and meta-analysis. Obes Rev. 2011;12:653–9.
Czernichow S, Beeker N, Rives-Lange C, Guerot E, Diehl JL, Katsahian S, et al. Obesity doubles mortality in patients hospitalized for SARS-CoV-2 in Paris hospitals, France: a cohort study on 5795 patients. Obesity. 2020;28:2282–9.
Garcia de Guadiana-Romualdo L, Calvo Nieves MD, Rodríguez Mulero MD, Calcerrada Alises I, Hernández Olivo M, Trapiello Fernández W, et al. MR-proADM as marker of endotheliitis predicts COVID-19 severity. Eur J Clin Invest. 2021;51:e13511.
Sozio E, Tascini C, Fabris M, D’Aurizio F, De Carlo C, Graziano E, et al. MR-proADM as prognostic factor of outcome in COVID-19 patients. Sci Rep. 2021;11:5121.
Montrucchio G, Sales G, Rumbolo F, Palmesino F, Fanelli V, Urbino C, et al. Effectiveness of mid-regional pro-adrenomedullin (MR-proADM) as prognostic marker in COVID-19 critically ill patients: an observational prospective study. PLoS One. 2021;16:e0246771.
Spoto S, Agro FE, Sambuco F, Travaglino F, Valeriani E, Fogolari M, et al. High value of mid-regional proadrenomedullin in COVID-19: a marker of widespread endothelial damage, disease severity and mortality. J Med Virol. 2020;93:2820–7.
Gregoriano C, Koch D, Kutz A, Haubitz S, Conen A, Bernasconi L, et al. The vasoactive peptide MR-pro-adrenomedullin in COVID-19 patients: an observational study. Clin Chem Lab Med. 2021;59:995–1004.
Benedetti L, Spinelli D, Callegari T, Bonometti R, Molinaro E, Novara E, et al. High levels of mid-regional proadrenomedullin in ARDS COVID-19 patients: the experience of a single, Italian center. Eur Rev Med Pharmacol Sci. 2021;25:1743–51.
Braun N, Hoess C, Kutz A, Christ-Crain M, Thomann R, Henzen C, et al. Obesity paradox in patients with community-acquired pneumonia: is inflammation the missing link? Nutrition. 2017;33:304–10.
Van Oers J, Krabbe J, Kemna E, Kluiters Y, Vos P, De Lange D, et al. Mid-regional proadrenomedullin and mid-regional proatrial natriuretic peptide clearance predicts poor outcome better than single baseline measurements in critically ill patients with pneumonia: a retrospective cohort study. Cureus. 2021;13:e15285.
Schetz M, de jong A, Deane AM, Druml W, Hemelaar P, Pelosi P, et al. Obesity in the critically ill: a narrative review. Intensive Care Med. 2019;45:757–69.
Pepper DJ, Sun J, Welsh J, Cui X, Suffredini AF, Eichacker PQ. Increased body mass index and adjusted mortality in ICU patients with sepsis or septic shock: a systematic review and meta-analysis. Crit Care. 2016;20:181.
Ball L, Serpa Neto A, Pelosi P. Obesity and survival in critically ill patients with acute respiratory distress syndrome: a paradox within the paradox. Crit Care. 2017;21:114.
Aldes PA, Savage PD. The obesity paradox: perception vs knowledge. Mayo Clin Proc. 2010;85:112–4.
Zamboni M, Mazzali G, Zoico E, Harris TB, Meigs JB, Di Francesco V, et al. Health consequences of obesity in the elderly: a review of four unresolved questions. Int J Obes. 2005;29:1011–29.
Dana R, Bannay A, Bourst P, Ziegler C, Losser MR, Gibot S, et al. Obesity and mortality in critically ill COVID-19 patients with respiratory failure. Int J Obes. 2021;45:2028–37.
Pouwels S, Ramnarain D, Aupers E, Rutjes-Weurding L, van Oers J. Obesity may not be associated with 28-day mortality, duration of invasive mechanical ventilation and length of intensive care unit and hospital stay in critically ill patients with severe acute respiratory syndrome coronavirus-2: A retrospective cohort study. Medicina. 2021;57:674.
Kooistra EJ, Brinkman S, van der Voort PHJ, de Keizer NF, Dongelmans DA, Kox M, et al. Body mass index and mortality in coronavirus disease 2019 and other diseases: a cohort study in 35,506 ICU patients. Crit Care Med. 2022;50:e1–e10.
Kotsis V, Stabouli S, Papakatsika S, Rizos Z, Parati G. Mechanisms of obesity-induced hypertension. Hypertens Rev. 2010;33:386–93.
Ouchi N, Parker JL, Lugus JL, Walsh K. Adipokines in inflammation and metabolic disease. Nat Rev Immunol. 2011;11:85–97.
Vila G, Riedl M, Maier C, Struck J, Morgenthaler NG, Handisurya A, et al. Plasma MR-proADM correlates to BMI and decreases in relation to leptin after gastric bypass surgery. Obesity. 2009;17:1184–8.
Del RyS, Cabiati M, Bianchi V, Caponi L, Di Cecco P, Marchi B, et al. Mid-regional-pro-adrenomedullin plasma levels are increased in obsess adolescents. Eur J Nutr. 2016;55:1255–60.
Voors AA, Kremer D, Geven C, Ter Maaten JM, Struck J, Bergmann A, et al. Adrenomedullin in heart failure: pathophysiology and therapeutic application. Eur J Heart Fail. 2019;21:163–71.
Buendgens L, Yagmur E, Bruensing J, Herbers U, Baeck C, Trautwein C, et al. C-terminal proendothelin-1 (CT-proET-1) is associated with organ failure and predicts mortality in critically ill patients. J Intensive Care. 2017;5:25.
Suthahar N, Meems LMG, Groothof D, Bakker SJL, Gansevoort RT, van Veldhuisen DJ, et al. Relationship between body mass index, cardiovascular biomarkers and incident heart failure. Eur J Heart Fail. 2021;23:396–402.
Krintus M, Kozinski M, Braga F, Kubica J, Sypniewska G, Pantegghini M. Plasma midregional proadrenomedullin (MR-proADM) concentrations and their biological determinants in a reference population. Clin Chem Lab Med. 2018;56:1161–8.
Smith JG, Newton-Cheh C, Hedblad B, Struck J, Morgenthaler NG, Bergmann A, et al. Distribution and correlates of midregional proadrenomedullin in the general population. Clin Chem. 2009;55:1593–5.
Baretella O, Chung SK, Xu A, Van Houtte PM. Pardoxical lack of increase in endothelin-1 levels in obese mice – possible role of endothelin-B receptors. Acta Pharmacol Sin. 2017;38:1699–1700.
Griffith GJ, Morris TT, Tudball MJ, Herbert A, Mancano G, Pike L, et al. Collider bias undermines our understanding of COVID-19 disease risk and severity. Nat Commun. 2020;11:5749.
Funding
Thermo Scientific provided free MR-proADM and CT-proET-1 laboratory kits for this study. Thermo Scientific had no involvement in data collection, data analysis, data interpretation, trial design or patient recruitment, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
JAHvO, SP, and DR designed the study and collected all data. YK and JAPB collected and analyzed the extra MR-proADM and CT-proET-1 laboratory samples. JAHvO, SP, DR, and H-JdG contributed to the data analysis and data interpretation. All authors contributed to the writing and reviewing of the manuscript. JAHvO, SP, and DR verify that they had access to and take responsibility for all the data in the manuscript. All authors read and approved the final manuscript and had final responsibility for the decision to submit the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the METC Brabant (Tilburg, the Netherlands) (METC number NW 2020–86).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
van Oers, J.A.H., Pouwels, S., Ramnarain, D. et al. Mid-regional proadrenomedullin, C-terminal proendothelin-1 values, and disease course are not different in critically ill SARS-CoV-2 pneumonia patients with obesity. Int J Obes 46, 1801–1807 (2022). https://doi.org/10.1038/s41366-022-01184-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01184-2