Abstract
Background/Objectives
Obesity is the main risk factor for obstructive sleep apnoea, commonly occurring in females who are overweight after menopause. We aimed to study the effect of a palaeolithic diet on sleep apnoea in females with overweight after menopause from the population.
Methods
Seventy healthy, non-smoking females with a mean age of 60 years and a mean BMI of 33 kg/m2 were randomised to a palaeolithic diet or to a control low-fat diet according to Nordic Nutritional Recommendations, for 2 years. The apnoea-hypopnoea index was measured and daytime sleepiness was estimated during the intervention.
Results
The mean apnoea-hypopnoea index at baseline was 11.6 (95% CI 8.6–14.5). The mean weight loss was 7.2 kg (95% CI 5.3–9.2 kg) in the palaeolithic diet group and 3.9 kg in the control group (95% CI 1.9–5.9 kg); p < 0.021 for the group difference. The reduction in weight corresponded to a reduction in the apnoea-hypopnoea index in the palaeolithic diet group (r = 0.38, p = 0.034) but not in the control group (r = 0.08, p = 0.69). The apnoea-hypopnoea index was reduced in the palaeolithic diet group when the weight was reduced by more than 8 kg. Daytime sleepiness according to the Epworth Sleepiness Scale score and the Karolinska Sleepiness Scale score was unaffected by dietary group allocation.
Conclusions
A substantial decrease in body weight of 8 kg was needed to achieve a reduction in sleep apnoea in this small trial of women who are overweight after menopause. The palaeolithic diet was more effective for weight reduction than a control low-fat diet and the reduction in sleep apnoea was related to the degree of weight decrement within this diet group.
Trial registration
Clinicaltrials.gov: NCT00692536.
Similar content being viewed by others
Introduction
Obstructive sleep apnoea is now estimated to affect almost a billion people worldwide [1] and up to 80% of women with obesity develop sleep apnoea [2]. Women after menopause run a particular risk of developing sleep apnoea. This may relate to fat mass redistribution, sex-hormone changes and age per se [3, 4]. Action to reduce weight in the population is needed to counteract poor health outcomes from obstructive sleep apnoea [5,6,7,8,9,10,11,12,13].
Obesity is an important risk factor for sleep apnoea and these patients are often recommended to reduce the severity of sleep apnoea by weight reduction. There are, however, mixed results regarding the resolution of sleep apnoea by dietary interventions or bariatric surgery [14,15,16,17,18,19,20,21]. The reason for this is unclear, but it may be due to the degree of weight reduction.
We and others have shown that a palaeolithic diet reduces body weight and improves metabolic factors [22,23,24]. The diet mimics our ancestors’ cuisine, with low carbohydrates and a high intake of monounsaturated fats and omega-3 fatty acids. To the best of our knowledge, no study has investigated the effect of a palaeolithic diet on sleep apnoea in people who are overweight from the population. This study aimed to investigate the effect of a palaeolithic diet on sleep apnoea in women who were overweight after menopause, compared with a low-fat control diet.
Methods
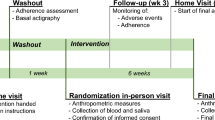
This is a secondary analysis from a randomised controlled trial comparing a palaeolithic diet with a low-fat control diet according to the Nordic Nutritional Recommendations, conducted in Umeå, Sweden [24]. The eligible group comprised 210 females who responded to advertisements in two local newspapers. Seventy females fulfilled the inclusion criteria of being postmenopausal, non-smoking, body mass index >27 kg/m2, healthy and free from medication, except for three women with well-controlled hypertension treated with an angiotensin-converting enzyme inhibitor. Investigations were recorded at baseline, after 6 months and after 2 years and included sleep apnoea recordings, subjective sleepiness scales, weight and height (Fig. 1). All the participants were invited to a follow-up, intention-to-treat analysis, regardless of whether they had continued the allocated diet. The participants were recruited from 4 September 2007 to 29 February 2008. Follow-up investigations were made from 4 October 2009 to 22 June 2010.
Ethical approval
The Regional Ethical Review Board at Umeå University approved the study protocols (no. 07-034 M), in accordance with the Helsinki Declaration, and all the patients gave their written informed consent.
Randomisation and masking
The included females were put in order according to their body mass index and randomised in blocks of four with an equal probability of being randomised to the palaeolithic diet (n = 35) or to the low-fat control diet (n = 35). The randomisation sequence was created by a statistician, using statistical software (IBM SPSS v. 19, Chicago, IL). All study personnel except the dieticians were blinded to dietary allocation.
Outcome measurements
The primary outcome of the trial was a change in fat mass over a period of 2 years [24]. Secondary outcomes included the apnoea-hypopnoea index and daytime sleepiness.
Procedures
Dietary intervention
The palaeolithic diet was based on lean meat, fish, eggs, vegetables, fruits, berries and nuts. Additional fat sources were avocado, rapeseed oil and olive oil. Dairy products, cereals, added salt, refined fats and sugar were excluded. The diet aimed at 30% of energy intake from protein, 40% of energy intake from fat, with a recommended high intake of mono- and polyunsaturated fatty acids, and 30% of energy intake from carbohydrates [24]. The control diet according to the official Nordic Nutritional Recommendations was based on low-fat and high-fibre products, aiming at a daily intake of 15% energy intake from protein, 25–30% energy intake from fat and 55–60% energy intake from carbohydrates [25].
One dietician per dietary group held 12 group sessions. Four cooking classes and four follow-up sessions were held during the first 6 months, followed by group meetings at 6, 12, 18 and 24 months. Participants were recommended to eat the advised food at three main meals and two snacks a day. Food intake was ad libitum for both diets, meaning that women could eat as much as they liked, without restriction. Recipes, written instructions and suggestions of food for breakfast, lunch and dinner were given during the 12 group sessions. The group sessions consisted of information on how to prepare and cook meals and dishes in the intervention diet. The sessions also included information about dietary effects on health, body weight and how to maintain behavioural changes. The group session on behavioural change was devoted to a discussion of different aspects of motivation, including group discussions of benefits and difficulties changing diet. Adherence to the diet intervention was monitored using self-reported 4-day food records at study start, monthly during the first 6 months and at 9, 12, 18 and 24 months. Participants were instructed to estimate the amount of food eaten from coloured food-portion photographs and household measuring utensils. Adherence to the different diets was assessed using the Dietist XP nutritional analysis package (version 3.0, Kost och Näringsdata AB, Bromma, Sweden), which converted the food intake to estimates of energy intake and nutrients. Adherence to protein intake was measured by nitrogen excretion in urine at baseline and after 6 and 24 months [24]. Body weight was measured at baseline and after 6, 12, 18 and 24 months.
Sleep apnoea recordings
The apnoea-hypopnoea index was measured with overnight sleep apnoea recordings (Embletta X10, Natus Medical Inc., CA, USA). It included continuous recordings of airflow using a nasal flow pressure sensor, thoracic and abdominal respiratory effort (XactTrace respiratory effort belts), finger pulse oximetry (Nonin Oximeter XPOD) and a body position sensor.
An obstructive apnoea was defined as a drop in airflow of at least 90% of the pre-event baseline for at least 10 s with continuing abdominal and thoracic movements, according to the American Academy of Sleep Medicine [26]. An obstructive hypopnoea was defined as a 50% reduction in airflow for at least 10 s compared with baseline, accompanied by abdominal and thoracic movements in combination with an oxygen desaturation of 3% or more. A central apnoea was scored as absent inspiratory effort throughout the entire period of airflow absence lasting 10 s or more [26]. All recordings were scored manually by one of the authors (CS) and the duration of sleep was estimated from the recordings.
Daytime sleepiness scales
Subjective sleepiness over a longer period was measured using the Epworth Sleepiness Scale, with a summary of answers rated from 0 to 3 to eight questions on sleepiness during the daytime, leading to a summary score of 0–24 [27]. The Karolinska Sleepiness Scale that assesses immediate sleepiness on a scale from 1 to 9 was measured at awakening in the morning, at 3 pm and at 10 pm [28].
Statistical methods
The sample size needed was estimated at 30 females in each arm to detect a significant difference in fat mass (p < 0.05) with a power of 80% [24]. In a post-hoc analysis, it was estimated that 65 patients in each group would be needed to detect a mean (SD) apnoea-hypopnoea index difference of 5 [10] units with a power of 80% and a significance level of 5%.
Baseline characteristics were presented as means and 95% confidence intervals. The differences between baseline and outcome were analysed with Student’s t test when comparing the diet groups. Model evaluations were carried out with residual analysis. The Mann–Whitney U-test was used when analysing differences in the apnoea-hypopnoea index due to outlier problems. All the tests were two sided. Pearson’s correlation coefficient was used to measure the linear correlation between the change in weight and body mass index and the change in apnoea-hypopnoea index. All the analyses were performed on an intention-to-treat basis. They included patients with low adherence to the diet intervention and all the patients were analysed with respect to randomisation. Patients who dropped out were also invited to a follow-up. A complete case analysis was performed, and missing data were assumed to be missing at random. A significance level of 0.05 was used. SPSS Statistics for Windows, Version 26.0, Armonk, NY: IBM Corp was used for statistical analysis.
Results
The mean apnoea-hypopnoea index at baseline was 11.6 (95% CI 8.6–14.5, range 0.3–73.8) among the 70 included females and 70% had an apnoea-hypopnoea index of 5 or more. No woman had central sleep apnoea. Two women with previously diagnosed sleep apnoea were treated with continuous positive airway pressure (CPAP), one in each dietary group, and they were investigated after three nights without treatment. The baseline characteristics did not differ between the diet groups (Table 1). Four females in the palaeolithic group and nine females in the control group quit further participation during the study period. Thirty-two females randomised to the palaeolithic diet and 30 females in the control group were investigated at follow-up after 2 years. The intention-to-treat analysis included five females who had stopped following the dietary recommendations during the study period, four in the palaeolithic group and one in the control group (Fig. 1).
In the palaeolithic diet group, body weight decreased by a mean of 7.2 (95% CI 5.3–9.2) kg, p < 0.001, from baseline to follow-up after 2 years, and the corresponding weight reduction was 3.9 kg (95% CI 1.9–5.9 kg) in the control group The between-group difference in weight was 3.4 (95% CI 0.5–6.2) kg, (p = 0.021). There was no between-group difference in the apnoea-hypopnoea index at 2 years (Table 2). The effect on outcome remained in a sub-analysis of women with sleep apnoea (apnoea-hypopnoea index > 5) at baseline (Table 3).
The reduction in weight corresponded to a reduction in the apnoea-hypopnoea index in the palaeolithic group (r = 0.38, p = 0.034) but not in the control group (r = 0.08, p = 0.69) (Fig. 2). The correlation between the change in body mass index and the change in the apnoea-hypopnoea index was also significant in the palaeolithic group (r = 0.137, p = 0.03) but not in the control group (r = 0.005, p = 0.70) (Fig. 3). A reduction in the apnoea-hypopnoea index after 2 years was observed in females in the palaeolithic group and in the control low-fat group, who lost more than 8 kg, p = 0.026 (Fig. 4). About 40% of the women in the palaeolithic group and 20% in the control group had lost more than 8 kg at follow-up.
A reduction in weight corresponded to a reduction in the apnoea-hypopnoea index in the palaeolithic diet group (r = 0.38, p = 0.034) but not in the control low-fat diet group (r = 0.08, p = 0.69). A decrease in the apnoea-hypopnoea index was mainly present in individuals with a weight reduction of more than 8 kg in the palaeolithic diet group.
Daytime sleepiness using the Epworth Sleepiness Scale score and the Karolinska Sleepiness Scale score on awakening, at 3 pm and at 10 pm did not change significantly from baseline to follow-up after 2 years in the palaeolithic diet group, without any difference in any score between the two randomised groups (Table 2).
Discussion
Here, we show that the reduction in weight in the palaeolithic diet group correlated with a reduction in the apnoea-hypopnoea index. This was linked to high adherence to the palaeolithic diet for 2 years, with a substantial weight reduction in women who were overweight after menopause, compared with a low-fat diet. A reduction in sleep apnoea occurred in women with a pronounced weight loss >8 kg, regardless of the diet group. This supports the finding that, the more weight that is lost, the greater the reduction in the apnoea-hypopnea index, found in previous trials [14,15,16, 18].
Despite significant weight reductions, there was no significant change in the mean apnoea-hypopnea index in either diet group after 2 years. The fact that the women were 2 years older at follow-up could explain the lack of effect on the apnoea-hypopnoea index. It is known that sleep apnoea worsens with age, especially in women in the menopausal transition [2, 29]. This further underlines the importance of weight reduction in women in relation to menopause.
The weight reduction was more pronounced in the palaeolithic group and 40% of them had a weight reduction of over 8 kg vs. 20% in the control group. We found a significant, albeit weak, dose-response relationship between weight loss and improvements in the apnoea-hypopnoea index in the palaeolithic diet group. One potential mechanism may be that palaeolithic diets, compared with low-fat diets, in previous randomised controlled trials have shown greater improvements in components of the metabolic syndrome, notably waist circumference and triglyceride levels [23] and earlier studies have found close relationships between the metabolic syndrome and the apnoea-hypopnoea index [30]. A palaeolithic diet can therefore be recommended to women who are overweight after menopause, with the understanding that it will only affect the severity of sleep apnoea if weight is reduced by more than 8 kg.
The mean apnoea-hypopnoea index at baseline was 11.6 and 70% of the present women previously had unrecognised obstructive sleep apnoea. This prevalence is well in line with earlier population-based studies [2, 31] and thus constitutes a group of women running a major risk of sleep apnoea-related metabolic disorders, cardiovascular events and mortality [5,6,7,8,9,10,11,12,13, 32].
A systematic review from 2013 concluded that lifestyle and dietary interventions improved obstructive sleep apnoea parameters but not sufficiently to normalise them [33]. A recent study also found that interventions combining physical activity and eating behaviour reduced the severity of sleep apnoea but was not curative and the problem of how to increase the effectiveness of lifestyle modifications remains [34]. The American Thoracic Society recommends “that clinicians regularly assess weight and incorporate weight management strategies that are tailored to individual patient preferences into the routine treatment of adult patients with obstructive sleep apnoea who are overweight or obese” [35]. This statement is based on a review of weight reduction trials among patients with overweight and sleep apnoea. Effects on apnoea frequency have been observed in studies using a very low-calorie diet [14, 15], energy restriction [36, 37], bariatric surgery [21] and pharmacological treatment [38, 39]. The study with the greatest weight reduction reported the largest reduction in the apnoea-hypopnoea index [14]. In contrast, a study reporting a mean weight loss of 1.7 kg with the Mediterranean diet had no effect on sleep apnoea [17]. This is in line with our key finding, i.e. a substantial weight loss is needed to achieve a pronounced reduction in the apnoea-hypopnoea index. However, in a recent trial, Georgoulis et al. reported that the Mediterranean diet and Mediterranean lifestyle interventions, in addition to CPAP treatment, reduce the severity of obstructive sleep apnoea, regardless of CPAP and weight loss, including cardiometabolic benefits [19, 20]. This diet has some similarities with the palaeolithic diet and future studies of diets of these types in patients with sleep apnoea are warranted.
The Sleep AHEAD study presented data that support our results [16]. This study included patients with obesity and type 2 diabetes, with or without sleep apnoea at study start. Half the patients were given a very low-calorie diet during the first 4 months, plus moderate to intense exercise for 3 h a week, with the individual goal of losing at least 7% of their initial body weight. The study subjects lost a mean of 10 kg and their apnoea-hypopnoea index was reduced by 10 units per hour of sleep after 12 months vs. controls. The initial apnoea-hypopnoea index and weight reduction were the strongest predictors of a reduction in sleep apnoea. Future lifestyle interventions in females after menopause, running an increased risk of obstructive sleep apnoea because of overweight, in combination with an increased cardiometabolic risk, should focus on profound weight reduction, as there may be an individual threshold effect for effects on sleep apnoea, in line with what has recently been suggested for the remission of type 2 diabetes [40].
Excessive daytime sleepiness is suggested as the most important symptom of sleep apnoea. One review found 15 articles reporting large improvements in daytime sleepiness after bariatric surgery and 27 studies that reported a moderate improvement after non-surgical weight reduction, with a non-linear association between weight loss and change in daytime sleepiness [8]. However, only a fraction of the women and men from the population with sleep apnoea report daytime sleepiness [41] and there has been a lack of any clear relationship between daytime sleepiness and sleep apnoea among women in the population [42]. It is thus possible that daytime sleepiness in women with overweigh after menopause is primarily due to factors other than sleep apnoea. This may explain why no effect was found between weight reduction and daytime sleepiness in the present trial.
One limitation is the small sample size and the large variability in the apnoea-hypopnea index, as women both with and without sleep apnoea at baseline were included. Another limitation is the use of simplified sleep apnoea recordings instead of polysomnography including an EEG for sleep scoring. We did not control for abstinence from alcohol and caffeine before the sleep apnoea recordings, which could have affected the results. The high adherence to the palaeolithic diet, with a low drop-out rate from the study over a period of 2 years, is a strength in the present study. Further studies with large sample sizes are needed before a palaeolithic diet can be recommended to people with obstructive sleep apnoea.
Conclusions
A substantial decrease in body weight of 8 kg was needed to achieve a reduction in sleep apnoea in women who are overweight after menopause. The palaeolithic diet was more effective for weight reduction than a control low-fat diet and the reduction in sleep apnoea was related to the degree of weight decrement within this diet group. The study sample size was limited and further studies are warranted.
Data availability
All data that support the findings are available on request to the corresponding authors within reason. Material and correspondence requests should be made to the corresponding author.
References
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7:687–98.
Franklin KA, Sahlin C, Stenlund H, Lindberg E. Sleep apnoea is a common occurrence in females. Eur Respir J. 2013;41:610–5.
Zolfaghari S, Yao C, Thompson C, Gosselin N, Desautels A, Dang-Vu TT, et al. Effects of menopause on sleep quality and sleep disorders: Canadian Longitudinal Study on Aging. Menopause. 2020;27:295–304.
Perger E, Mattaliano P, Lombardi C. Menopause and Sleep Apnea. Maturitas. 2019;124:35–8.
Perger E, Pengo MF, Lombardi C. Hypertension and atrial fibrillation in obstructive sleep apnea: is it a menopause issue? Maturitas. 2019;124:32–4.
Linz D, McEvoy RD, Cowie MR, Somers VK, Nattel S, Levy P, et al. Associations of obstructive sleep apnea with atrial fibrillation and continuous positive airway pressure treatment: a review. JAMA Cardiol. 2018;3:532–40.
Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, et al. Sleep Apnea: Types, Mechanisms, and Clinical Cardiovascular Consequences. J Am Coll Cardiol. 2017;69:841–58.
Ng WL, Stevenson CE, Wong E, Tanamas S, Boelsen-Robinson T, Shaw JE, et al. Does intentional weight loss improve daytime sleepiness? A systematic review and meta-analysis. Obes Rev. 2017;18:460–75.
Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O’Connor GT, Resnick HE, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182:269–77.
Valham F, Mooe T, Rabben T, Stenlund H, Wiklund U, Franklin KA. Increased risk of stroke in patients with coronary artery disease and sleep apnea: a 10-year follow-up. Circulation. 2008;118:955–60.
Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53.
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41.
Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84.
Johansson K, Neovius M, Lagerros YT, Harlid R, Rossner S, Granath F, et al. Effect of a very low energy diet on moderate and severe obstructive sleep apnoea in obese men: a randomised controlled trial. BMJ. 2009;339:b4609.
Tuomilehto HP, Seppa JM, Partinen MM, Peltonen M, Gylling H, Tuomilehto JO, et al. Lifestyle intervention with weight reduction: first-line treatment in mild obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179:320–7.
Foster GD, Borradaile KE, Sanders MH, Millman R, Zammit G, Newman AB, et al. A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the Sleep AHEAD study. Arch Intern Med. 2009;169:1619–26.
Papandreou C, Schiza SE, Bouloukaki I, Hatzis CM, Kafatos AG, Siafakas NM, et al. Effect of Mediterranean diet versus prudent diet combined with physical activity on OSAS: a randomised trial. Eur Respir J. 2012;39:1398–404.
Dixon JB, Schachter LM, O’Brien PE, Jones K, Grima M, Lambert G, et al. Surgical vs conventional therapy for weight loss treatment of obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;308:1142–9.
Georgoulis M, Yiannakouris N, Kechribari I, Lamprou K, Perraki E, Vagiakis E, et al. Cardiometabolic Benefits of a Weight-Loss Mediterranean Diet/Lifestyle Intervention in Patients with Obstructive Sleep Apnea: The “MIMOSA” Randomized Clinical Trial. Nutrients. 2020;12:1570.
Georgoulis M, Yiannakouris N, Kechribari I, Lamprou K, Perraki E, Vagiakis E, et al. The effectiveness of a weight-loss Mediterranean diet/lifestyle intervention in the management of obstructive sleep apnea: results of the “MIMOSA” randomized clinical trial. Clin Nutr. 2021;40:850–9.
Furlan SF, Drager LF, Santos RN, Damiani LP, Bersch-Ferreira AC, Miranda TA, et al. Three-year effects of bariatric surgery on obstructive sleep apnea in patients with obesity grade 1 and 2: a sub-analysis of the GATEWAY trial. Int J Obes (Lond). 2021;45:914–7.
Fraczek B, Pieta A, Burda A, Mazur-Kurach P, Tyrala F. Paleolithic Diet-Effect on the Health Status and Performance of Athletes? Nutrients. 2021;13:1019.
Manheimer EW, van Zuuren EJ, Fedorowicz Z, Pijl H. Paleolithic nutrition for metabolic syndrome: systematic review and meta-analysis. Am J Clin Nutr. 2015;102:922–32.
Mellberg C, Sandberg S, Ryberg M, Eriksson M, Brage S, Larsson C, et al. Long-term effects of a Palaeolithic-type diet in obese postmenopausal women: a 2-year randomized trial. Eur J Clin Nutr. 2014;68:350–7.
Becker W. New Nordic nutrition recommendations 2004. Physical activity as important as good nourishing food. Lakartidningen. 2005;102:2757–8. 2760-2.
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597–619.
Johns MW. Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep. 1994;17:703–10.
Akerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosci. 1990;52:29–37.
Young T, Finn L, Austin D, Peterson A. Menopausal status and sleep-disordered breathing in the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2003;167:1181–5.
Theorell-Haglow J, Berne C, Janson C, Lindberg E. The role of obstructive sleep apnea in metabolic syndrome: a population-based study in women. Sleep Med. 2011;12:329–34.
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3:310–8.
Muraki I, Wada H, Tanigawa T. Sleep apnea and type 2 diabetes. J Diabetes Investig. 2018;9:991–7.
Araghi MH, Chen YF, Jagielski A, Choudhury S, Banerjee D, Hussain S, et al. Effectiveness of lifestyle interventions on obstructive sleep apnea (OSA): systematic review and meta-analysis. Sleep. 2013;36:1562A–1562E.
Igelstrom H, Asenlof P, Emtner M, Lindberg E. Improvement in obstructive sleep apnea after a tailored behavioural sleep medicine intervention targeting healthy eating and physical activity: a randomised controlled trial. Sleep Breath. 2018;22:653–61.
Hudgel DW, Patel SR, Ahasic AM, Bartlett SJ, Bessesen DH, Coaker MA, et al. The Role of Weight Management in the Treatment of Adult Obstructive Sleep Apnea. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2018;198:e70–e87.
Fernandes JF, Araujo Lda S, Kaiser SE, Sanjuliani AF, Klein MR. The effects of moderate energy restriction on apnoea severity and CVD risk factors in obese patients with obstructive sleep apnoea. Br J Nutr. 2015;114:2022–31.
Ng SSS, Chan RSM, Woo J, Chan TO, Cheung BHK, Sea MMM, et al. A Randomized Controlled Study to Examine the Effect of a Lifestyle Modification Program in OSA. Chest. 2015;148:1193–203.
Blackman A, Foster GD, Zammit G, Rosenberg R, Aronne L, Wadden T, et al. Effect of liraglutide 3.0 mg in individuals with obesity and moderate or severe obstructive sleep apnea: the SCALE Sleep Apnea randomized clinical trial. Int J Obes (Lond). 2016;40:1310–9.
Winslow DH, Bowden CH, DiDonato KP, McCullough PA. A randomized, double-blind, placebo-controlled study of an oral, extended-release formulation of phentermine/topiramate for the treatment of obstructive sleep apnea in obese adults. Sleep. 2012;35:1529–39.
Taylor R. Type 2 diabetes and remission: practical management guided by pathophysiology. J Intern Med. 2021;289:754–70.
Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis. 2015;7:1311–22.
Svensson M, Franklin KA, Theorell-Haglow J, Lindberg E. Daytime sleepiness relates to snoring independent of the apnea-hypopnea index in women from the general population. Chest. 2008;134:919–24.
Acknowledgements
Inger Arnesjö, Katarina Iselid and Monica Holmgren assisted with the health screening of the study participants and provided technical assistance and Susanne Sandberg informed the participants about the diets and analysed their food records. AnnChatrin Edlund assisted with the sleep apnoea recordings.
Funding
Financial support was received from the Swedish Heart and Lung Foundation, Swedish Research Council, Swedish Research Council for Working Life and Social Research, the County Council of Västerbotten and Umeå University. Open access funding provided by Umea University.
Author information
Authors and Affiliations
Contributions
TO, CL, BL, KAF, CM and MR designed the study, while CS, CM and MR collected data and KAF, EL, JS, CS, TO and MR played an important role in interpreting the results. KAF, EL, To and MR drafted the paper and JS, CL, BL, CM and CV revised the paper. All the authors agreed to be accountable for every aspect of the work of ensuring that questions related to the accuracy or integrity of any part of the work have been appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Franklin, K.A., Lindberg, E., Svensson, J. et al. Effects of a palaeolithic diet on obstructive sleep apnoea occurring in females who are overweight after menopause—a randomised controlled trial. Int J Obes 46, 1833–1839 (2022). https://doi.org/10.1038/s41366-022-01182-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01182-4
This article is cited by
-
Influence of nutrition and food on sleep—is there evidence?
Sleep and Breathing (2023)