Abstract
Background/objectives
Chronotype, i.e., the individual attitude to carry out the daily activities at a certain time of the day, has been reported to play a role in metabolic diseases. Thus, the aim of our study was to investigate the association of non-alcoholic fatty liver disease (NAFLD) with chronotype categories in individuals with obesity.
Subjects/methods
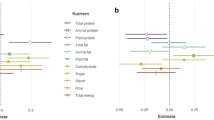
In this cross-sectional study, participants underwent to anthropometric, biochemical, and the Visceral Adiposity Index (VAI) assessment. Chronotype categories were assessed by the Horne–Ostberg Morningness–Eveningness Questionnaire (MEQ). The following indirect indices of NAFLD were calculated: Liver Fat Equation (LFE), Hepatic Steatosis Index (HSI) and Index of Non-alcoholic steatohepatitis (ION).
Results
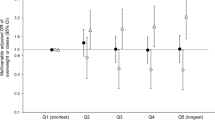
The study population consisted of 87 participants (40.3 ± 12.3 years; BMI 45.6 ± 6.3 kg/m2; 64F/23M). According to the chronotype score, 31.0% were morning (MC), 36.8% were intermediate (IC), and 32.2% evening chronotype (EC). Individuals with IC were significantly younger than those with MC and EC (p = 0.002 and p = 0.047, respectively). EC presented significantly higher BMI (p < 0.001), waist circumference (p = 0.007), and hip circumference (p = 0.001) than MC. Moreover, EC had higher BMI (p < 0.001) and waist circumference (p = 0.011) than IC. All participants presented NAFLD (HSI ≥ 36 and LFE ≥ 5). Nevertheless, only individuals with EC were above the threshold of non-alcoholic steatohepatitis evaluated as ION index (ION ≥ 50). Individuals with EC presented significantly higher VAI (p = 0.036), LFE (p = 0.034), HSI (p < 0.001) and ION (p = 0.014) than MC, also after the adjustment for age, gender, and BMI.
Conclusion
EC is associated with more severe NAFLD independently of age, gender, and BMI than MC and IC in individuals with obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stenvers DJ, Scheer FAJL, Schrauwen P, la Fleur SE, Kalsbeek A. Circadian clocks and insulin resistance. Nat Rev Endocrinol. 2019;15:75–89. https://doi.org/10.1038/s41574-018-0122-1.
Muscogiuri G, Barrea L, Aprano S, Framondi L, Di Matteo R, Laudisio D, et al. Chronotype and adherence to the Mediterranean diet in obesity: results from the opera prevention project. Nutrients. 2020;12:1354. https://doi.org/10.3390/nu12051354.
Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110.
Han H, Dou J, Hou Q, Wang H. Role of circadian rhythm and impact of circadian rhythm disturbance on the metabolism and disease. J Cardiovasc Pharmacol. 2021; https://doi.org/10.1097/FJC.0000000000001178.
Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA 2009;106:4453–8. https://doi.org/10.1073/pnas.0808180106.
Wong PM, Hasler BP, Kamarck TW, Muldoon MF, Manuck SB. Social jetlag, chronotype, and cardiometabolic risk. J Clin Endocrinol Metab. 2015;100:4612–20. https://doi.org/10.1210/jc.2015-2923.
Barrea L, Vetrani C, Altieri B, Verde L, Savastano S, Colao A, et al. The importance of being a ‘lark’ in post-menopausal women with obesity: a ploy to prevent type 2 diabetes mellitus? Nutrients. 2021;13:3762. https://doi.org/10.3390/nu13113762.
Lotti S, Pagliai G, Colombini B, Sofi F, Dinu M. Chronotype differences in energy intake, cardiometabolic risk parameters, cancer and depression: a systematic review with meta-analysis of observational studies. Adv Nutr. 2021:nmab115. https://doi.org/10.1093/advances/nmab115.
Makarem N, Paul J, Giardina EGV, Liao M, Aggarwal B. Evening chronotype is associated with poor cardiovascular health and adverse health behaviors in a diverse population of women. Chronobiol. Int. 2020;37:673–85. https://doi.org/10.1080/07420528.2020.1732403.
Divella R, Mazzocca A, Daniele A, Sabbà C, Paradiso A. Obesity, nonalcoholic fatty liver disease and adipocytokines network in promotion of cancer. Int J Biol Sci. 2019;15:610–6. https://doi.org/10.7150/ijbs.29599.
Chitturi S, Abeygunasekera S, Farrell GC, Holmes-Walker J, Hui JM, Fung C, et al. NASH and insulin resistance: Insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology. 2002;35:373–9. https://doi.org/10.1053/jhep.2002.30692.
Wong VW, Hui AY, Tsang SW, Chan JL, Tse AM, Chan KF, et al. Metabolic and adipokine profile of Chinese patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2006;4:1154–61. https://doi.org/10.1016/j.cgh.2006.06.011.
Della Pepa G, Vetrani C, Lombardi G, Bozzetto L, Annuzzi G, Rivellese AA. Isocaloric dietary changes and non-alcoholic fatty liver disease in high cardiometabolic risk individuals. Nutrients. 2017;9:1065. https://doi.org/10.3390/nu9101065.
Turek FW, Joshu C, Kohsaka A, Lin E, Ivanova G, McDearmon E, et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science. 2005;308:1043–5. https://doi.org/10.1126/science.1108750.
Shimba S, Ogawa T, Hitosugi S, Ichihashi Y, Nakadaira Y, Kobayashi M, et al. Deficient of a clock gene, brain and muscle Arnt-like protein-1 (BMAL1), induces dyslipidemia and ectopic fat formation. PLoS One. 2011;6:e25231. https://doi.org/10.1371/journal.pone.0025231.
Kohsaka A, Laposky AD, Ramsey KM, Estrada C, Joshu C, Kobayashi Y, et al. High-fat diet disrupts behavioral and molecular circadian rhythms in mice. Cell Metab. 2007;6:414–21. https://doi.org/10.1016/j.cmet.2007.09.006.
Adamovich Y, Rousso-Noori L, Zwighaft Z, Neufeld-Cohen A, Golik M, Kraut-Cohen J, et al. Circadian clocks and feeding time regulate the oscillations and levels of hepatic triglycerides. Cell Metab. 2014;19:319–30. https://doi.org/10.1016/j.cmet.2013.12.016.
Yu JH, Yun CH, Ahn JH, Suh S, Cho HJ, Lee SK, et al. Evening chronotype is associated with metabolic disorders and body composition in middle-aged adults. J Clin Endocrinol Metab. 2015;100:1494–502. https://doi.org/10.1210/jc.2014-3754.
Muscogiuri G, Barrea L, Aprano S, Framondi L, Di Matteo R, Altieri B, et al. Chronotype and cardio metabolic health in obesity: does nutrition matter? Int J Food Sci Nutr. 2021;72:892–900. https://doi.org/10.1080/09637486.2021.1885017.
Lohman TM, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics; 1988.
Barrea L, Muscogiuri G, Pugliese G, Laudisio D, de Alteriis G, Graziadio C, et al. Phase angle as an easy diagnostic tool of meta-inflammation for the nutritionist. Nutrients. 2021;13:1446. https://doi.org/10.3390/nu13051446.
Madden AM, Smith S. Body composition and morphological assessment of nutritional status in adults: a review of anthropometric variables. J Hum Nutr Diet. 2016;29:7–25. https://doi.org/10.1111/jhn.12278.
Barrea L, Muscogiuri G, Pugliese G, Graziadio C, Maisto M, Pivari F, et al. Association of the chronotype score with circulating trimethylamine N-oxide (TMAO) concentrations. Nutrients. 2021;13:1671. https://doi.org/10.3390/nu13051671.
Della Pepa G, Russo M, Vitale M, Carli F, Vetrani C, Masulli M, et al. Pioglitazone even at low dosage improves NAFLD in type 2 diabetes: clinical and pathophysiological insights from a subgroup of the TOSCA.IT randomised trial. Diabetes Res Clin Pract. 2021;178:108984. https://doi.org/10.1016/j.diabres.2021.108984.
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, et al. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33:920–2. https://doi.org/10.2337/dc09-1825.
Kotronen A, Peltonen M, Hakkarainen A, Sevastianova K, Bergholm R, Johansson LM, et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology. 2009;137:865–72. https://doi.org/10.1053/j.gastro.2009.06.005.
Lee JH, Kim D, Kim HJ, Lee CH, Yang JI, Kim W, et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis. 2010;42:503–8. https://doi.org/10.1016/j.dld.2009.08.002.
Otgonsuren M, Estep MJ, Hossain N, Younossi E, Frost S, Henry L, et al. Single non-invasive model to diagnose non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH). J. Gastroenterol Hepatol. 2014;29:2006–13. https://doi.org/10.1111/jgh.12665.
Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. https://doi.org/10.3389/fpsyg.2013.00863.
Ruiz-Lozano T, Vidal J, de Hollanda A, Canteras M, Garaulet M, Izquierdo-Pulido M. Evening chronotype associates with obesity in severely obese subjects: interaction with CLOCK 3111T/C. Int J Obes. 2016;40:1550–7. https://doi.org/10.1038/ijo.2016.116.
Torres-Castillo N, Martinez-Lopez E, Vizmanos-Lamotte B, Garaulet M. Healthy obese subjects differ in chronotype, sleep habits, and adipose tissue fatty acid composition from their non-healthy counterparts. Nutrients. 2020;13:119. https://doi.org/10.3390/nu13010119.
Arora T, Taheri S. Associations among late chronotype, body mass index and dietary behaviors in young adolescents. Int J Obes. 2015;39:39–44. https://doi.org/10.1038/ijo.2014.157.
Muñoz JSG, Cañavate R, Hernández CM, Cara-Salmerón V, Morante JJH. The association among chronotype, timing of food intake and food preferences depends on body mass status. Eur J Clin Nutr. 2017;71:736–42. https://doi.org/10.1038/ejcn.2016.182.
Lucassen EA, Zhao X, Rother KI, Mattingly MS, Courville AB, de Jonge L, et al. Evening chronotype is associated with changes in eating behavior, more sleep apnea, and increased stress hormones in short sleeping obese individuals. PLoS One. 2013;8:e56519. https://doi.org/10.1371/journal.pone.0056519.
Xiao Q, Garaulet M, Scheer FAJL. Meal timing and obesity: interactions with macronutrient intake and chronotype. Int J Obes. 2019;43:1701–11. https://doi.org/10.1038/s41366-018-0284-x.
Maukonen M, Kanerva N, Partonen T, Männistö S. Chronotype and energy intake timing in relation to changes in anthropometrics: a 7-year follow-up study in adults. Chronobiol Int. 2019;36:27–41. https://doi.org/10.1080/07420528.2018.1515772.
McMahon DM, Burch JB, Youngstedt SD, Wirth MD, Hardin JW, Hurley TG, et al. Relationships between chronotype, social jetlag, sleep, obesity and blood pressure in healthy young adults. Chronobiol Int. 2019;36:493–509. https://doi.org/10.1080/07420528.2018.1563094.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22:939–43. https://doi.org/10.1016/j.cub.2012.03.038.
Parsons MJ, Moffitt TE, Gregory AM, Goldman-Mellor S, Nolan PM, Poulton R, et al. Social jetlag, obesity and metabolic disorder: investigation in a cohort study. Int J Obes. 2015;39:842–8. https://doi.org/10.1038/ijo.2014.201.
Muscogiuri G, Barrea L, Annunziata G, Di Somma C, Laudisio D, Colao A, et al. Obesity and sleep disturbance: the chicken or the egg? Crit Rev Food Sci Nutr. 2019;59:2158–65. https://doi.org/10.1080/10408398.2018.1506979.
Muscogiuri G, Tuccinardi D, Nicastro V, Barrea L, Colao A, Savastano S. Sleep disturbances: one of the culprits of obesity-related cardiovascular risk? Int J Obes Suppl. 2020;10:62–72. https://doi.org/10.1038/s41367-020-0019-z.
Pugliese G, Barrea L, Laudisio D, Salzano C, Aprano S, Colao A, et al. Sleep apnea, obesity, and disturbed glucose homeostasis: epidemiologic evidence, biologic insights, and therapeutic strategies. Curr Obes Rep. 2020;9:30–38. https://doi.org/10.1007/s13679-020-00369-y.
Dockray S, Steptoe A. Chronotype and diurnal cortisol profile in working women: differences between work and leisure days. Psychoneuroendocrinology. 2011;36:649–55. https://doi.org/10.1016/j.psyneuen.2010.09.008.
Kudielka BM, Federenko IS, Hellhammer DH, Wüst S. Morningness and eveningness: the free cortisol rise after awakening in “early birds” and “night owls”. Biol Psychol. 2006;72:141–6. https://doi.org/10.1016/j.biopsycho.2005.08.003.
Baudrand R, Vaidya A. Cortisol dysregulation in obesity-related metabolic disorders. Curr Opin Endocrinol Diabetes Obes. 2015;22:143–9. https://doi.org/10.1097/MED.0000000000000152.
Abraham SB, Rubino D, Sinaii N, Ramsey S, Nieman LK. Cortisol, obesity, and the metabolic syndrome: a cross-sectional study of obese subjects and review of the literature. Obesity. 2013;21:E105–E117. https://doi.org/10.1002/oby.20083.
Castera L, Friedrich-Rust M, Loomba R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156:1264–.e4. https://doi.org/10.1053/j.gastro.2018.12.036.
Hassani Zadeh S, Mansoori A, Hosseinzadeh M. Relationship between dietary patterns and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2021;36:1470–8. https://doi.org/10.1111/jgh.15363.
Mir HM, Stepanova M, Afendy H, Cable R, Younossi ZM. Association of sleep disorders with nonalcoholic fatty liver disease (NAFLD): a population-based study. J Clin Exp Hepatol. 2013;3:181–5. https://doi.org/10.1016/j.jceh.2013.06.004.
Woods CP, Hazlehurst JM, Tomlinson JW. Glucocorticoids and non-alcoholic fatty liver disease. J Steroid Biochem Mol Biol. 2015;154:94–103. https://doi.org/10.1016/j.jsbmb.2015.07.020.
Targher G, Bertolini L, Rodella S, Zoppini G, Zenari L, Falezza G. Associations between liver histology and cortisol secretion in subjects with nonalcoholic fatty liver disease. Clin Endocrinol. 2006;64:337–41. https://doi.org/10.1111/j.1365-2265.2006.02466.x.
Holt HB, Wild SH, Postle AD, Zhang J, Koster G, Umpleby M, et al. Cortisol clearance and associations with insulin sensitivity, body fat and fatty liver in middle-aged men. Diabetologia. 2007;50:1024–32. https://doi.org/10.1007/s00125-007-0629-9.
Mukherji A, Bailey SM, Staels B, Baumert TF. The circadian clock and liver function in health and disease. J Hepatol. 2019;71:200–11. https://doi.org/10.1016/j.jhep.2019.03.020.
Ferrante A, Gellerman D, Ay A, Woods KP, Filipowicz AM, Jain K, et al. Diurnal preference predicts phase differences in expression of human peripheral circadian clock genes. J Circadian Rhythms. 2015;13:4. https://doi.org/10.5334/jcr.ae.
Acknowledgements
The authors thank the study participants.
Author information
Authors and Affiliations
Contributions
CV, LB, and GM were responsible for conceptualization; CV and LB conducted the statistical analysis and wrote the manuscript; LV, GS, AD, and GdA contributed to the methodology, including data collection and data management. SS, AC, and GM provided a critical review of the paper. All authors contributed to the critical review and agreed on the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Vetrani, C., Barrea, L., Verde, L. et al. Evening chronotype is associated with severe NAFLD in obesity. Int J Obes 46, 1638–1643 (2022). https://doi.org/10.1038/s41366-022-01159-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01159-3
This article is cited by
-
Is chronotype linked with adherence to the Mediterranean diet among adolescents? The EHDLA study
Pediatric Research (2023)
-
Chronotype and Sleep Quality in Obesity: How Do They Change After Menopause?
Current Obesity Reports (2022)