Abstract
Background
Bariatric and Metabolic Surgery (BMS) is a popular weight loss intervention worldwide, yet few scientific studies have examined variations in preoperative practices globally. This study aimed to capture global variations in preoperative practices concerning patients planned for BMS.
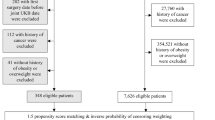
Methods
A 41-item questionnaire-based survey was designed and the survey link was freely distributed on social and scientific media platforms, email groups and circulated through personal connections of authors. The survey included eight parts: basic information; criteria for BMS; preoperative nutritional screening; preoperative weight loss; preoperative diets for liver size reduction; preoperative glycemic control; other laboratory investigations and preparations; decision making, education, and consents. Descriptive statistics were used to analyse data and graphs were used for representation where applicable.
Results
Six hundred thirty-four bariatric healthcare professionals from 76 countries/regions completed the survey. Of these, n = 310 (48.9%) were from public hospitals, n = 466 (73.5%) were surgeons, and the rest were multidisciplinary professionals. More than half of respondents reported using local society/association guidelines in their practice (n = 310, 61.6%). The great majority of respondents routinely recommend nutritional screening preoperatively (n = 385, 77.5%), mandatory preoperative diets for liver size reduction (n = 220, 53.1%), routine screening for T2DM (n = 371, 90.7%), and mandate a glycemic control target before BMS in patients with T2DM (n = 203, 55.6%). However, less than half (n = 183, 43.9%) recommend mandatory preoperative weight loss to all patients. Most respondents (n = 296, 77.1%) recommend psychological intervention before surgery for patients diagnosed with psychological conditions. Variations were also identified in laboratory investigations and optimisation; and in the aspects of decision making, education and consent.
Conclusions
This survey identified significant global variations in preoperative practices concerning patients seeking primary BMS. Our findings could facilitate future research for the determination of best practice in these areas of variations, and consensus-building to guide clinical practice while we wait for that evidence to emerge.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Angrisani L, Santonicola A, Iovino P, Ramos A, Shikora S, Kow L. Bariatric surgery survey 2018: similarities and disparities among the 5 IFSO chapters. Obes Surg. 2021;31:1937–48.
Arterburn DE, Telem DA, Kushner RF, Courcoulas AP. Benefits and risks of bariatric surgery in adults: a review. Jama. 2020;324:879–87.
Cummings DE, Rubino F. Metabolic surgery for the treatment of type 2 diabetes in obese individuals. Diabetologia. 2018;61:257–64.
Hazlehurst JM, Logue J, Parretti HM, Abbott S, Brown A, Pournaras DJ, et al. Developing integrated clinical pathways for the management of clinically severe adult obesity: a critique of NHS England policy. Curr Obes Rep. 2020;9:530–43.
Mahawar KK, Small PK. Medical weight management before bariatric surgery: is it an evidence-based intervention or a rationing tool? Clin Obes. 2016;6:359–60.
Kelley K, Clark B, Brown V, Sitzia J. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15:261–6.
NIH conference. Gastrointestinal surgery for severe obesity. Consensus development conference panel. Ann Intern Med. 1991;115:956–61.
Yermilov I, McGory ML, Shekelle PW, Ko CY, Maggard MA. Appropriateness criteria for bariatric surgery: beyond the NIH guidelines. Obesity. 2009;17:1521–7.
Bhasker AG, Prasad A, Raj PP, Wadhawan R, Khaitan M, Agarwal AJ, et al. OSSI (obesity and metabolic surgery society of India) guidelines for patient and procedure selection for bariatric and metabolic surgery. Obes Surg. 2020;30:2362–8.
Yang W, Wang C. Chinese Obesity and Metabolic Surgery Collaborative. Metabolic Surgery Needs Stronger Endorsement in Asian T2DM Patients with Low BMI. Obes Surg. 2022;32:212–13.
Kasama K, Mui W, Lee WJ, Lakdawala M, Naitoh T, Seki Y, et al. IFSO-APC consensus statements 2011. Obes Surg. 2012;22:677–84.
Livingston EH. Pitfalls in using BMI as a selection criterion for bariatric surgery. Curr Opin Endocrinol Diabetes Obes. 2012;19:347–51.
Oskrochi Y, Majeed A, Easton G. Biting off more than we can chew: is BMI the correct standard for bariatric surgery eligibility? Br J Gen Pract. 2015;65:482–3.
Guan B, Yang J, Chen Y, Yang W, Wang C. Nutritional deficiencies in Chinese patients undergoing gastric bypass and sleeve gastrectomy: prevalence and predictors. Obes Surg. 2018;28:2727–36.
Wang C, Guan B, Yang W, Yang J, Cao G, Lee S. Prevalence of electrolyte and nutritional deficiencies in Chinese bariatric surgery candidates. Surg Obes Relat Dis. 2016;12:629–34.
Zhang W, Fan M, Wang C, Mahawar K, Parmar C, Chen W, et al. Global Bariatric Research Collaborative. Hair Loss After Metabolic and Bariatric Surgery: a Systematic Review and Meta-analysis. Obes Surg. 2021;31:2649–59.
Zhang W, Fan M, Wang C, Mahawar K, Parmar C, Chen W, et al. Global Bariatric Research Collaborative. Importance of Maintaining Zinc and Copper Supplement Dosage Ratio After Metabolic and Bariatric Surgery. Obes Surg. 2021;31:3339–40.
Elhag W, El Ansari W. Nutritional Deficiencies Among Adolescents Before and After Sleeve Gastrectomy: First Study with 9-Year Followup. Obes Surg. 2022;32:284–94.
Bretault M, Zaharia R, Vigan M, Vychnevskaia K, Raffin-Sanson ML, Crenn P, et al. Complications requiring intensive nutritional care after bariatric surgery result in more long-term weight loss but has no impact on nutritional deficiencies and depression-anxiety scores. Obes Surg. 2021;31:4767–75.
Gasmi A, Bjørklund G, Mujawdiya PK, Semenova Y, Peana M, Dosa A, et al. Micronutrients deficiences in patients after bariatric surgery. Eur J Nutr. 2022;61:55–67.
Mahawar KK, Bhasker AG, Bindal V, Graham Y, Dudeja U, Lakdawala M, et al. Zinc deficiency after gastric bypass for morbid obesity: a systematic review. Obes Surg. 2017;27:522–9.
Kumar P, Hamza N, Madhok B, De Alwis N, Sharma M, Miras AD, et al. Copper deficiency after gastric bypass for morbid obesity: a systematic review. Obes Surg. 2016;26:1335–42.
O’Kane M, Parretti HM, Pinkney J, Welbourn R, Hughes CA, Mok J, et al. British obesity and metabolic surgery society guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery-2020 update. Obes Rev. 2020;21:e13087.
Mechanick JI, Apovian C, Brethauer S, Timothy Garvey W, Joffe AM, Kim J, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic and Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Obesity. 2020;28:O1–o58.
Sun Y, Liu B, Smith JK, Correia MLG, Jones DL, Zhu Z, et al. Association of preoperative body weight and weight loss with risk of death after bariatric surgery. JAMA Netw Open. 2020;3:e204803.
Eng V, Garcia L, Khoury H, Morton J, Azagury D. Preoperative weight loss: is waiting longer before bariatric surgery more effective? Surg Obes Relat Dis. 2019;15:951–7.
Schiavo L, Scalera G, Sergio R, De Sena G, Pilone V, Barbarisi A. Clinical impact of Mediterranean-enriched-protein diet on liver size, visceral fat, fat mass, and fat-free mass in patients undergoing sleeve gastrectomy. Surg Obes Relat Dis. 2015;11:1164–70.
Holderbaum M, Casagrande DS, Sussenbach S, Buss C. Effects of very low calorie diets on liver size and weight loss in the preoperative period of bariatric surgery: a systematic review. Surg Obes Relat Dis. 2018;14:237–44.
Samuel N, Mustafa A, Hawkins H, Wei N, Boyle M, De Alwis N, et al. Influence of Pre-operative HbA1c on Bariatric Surgery Outcomes-the Sunderland (UK) Experience. ObesSurg. 2022;32:42–47.
de Raaff CAL, Gorter-Stam MAW, de Vries N, Sinha AC, Jaap Bonjer H, Chung F, et al. Perioperative management of obstructive sleep apnea in bariatric surgery: a consensus guideline. Surg Obes Relat Dis. 2017;13:1095–109.
de Raaff CAL, de Vries N, van Wagensveld BA. Obstructive sleep apnea and bariatric surgical guidelines: summary and update. Curr Opin Anaesthesiol. 2018;31:104–9.
O’Reilly E, Doherty L, O’Boyle C. How relevant is pre-operative obstructive sleep apnoea in the asymptomatic bariatric surgery patient? Obes Surg. 2020;30:969–74.
Wolvers PJD, Ayubi O, Bruin SC, Hutten BA, Brandjes DPM, Meesters EW, et al. Smoking behaviour and beliefs about smoking cessation after bariatric surgery. Obes Surg. 2021;31:239–49.
David LA, Sijercic I, Cassin SE. Preoperative and post-operative psychosocial interventions for bariatric surgery patients: A systematic review. Obes Rev. 2020;21:e12926.
Graham Y, Callejas-Diaz L, Parkin L, Mahawar K, Small PK, Hayes C. Exploring the patient-reported impact of the pharmacist on pre-bariatric surgical assessment. Obes Surg. 2019;29:891–902.
Lee YC, Wu WL. Shared decision making and choice for bariatric surgery. Int J Environ Res Public Health. 2019;16:4966.
Hamadi R, Marlow CF, Nassereddine S, Taher A, Finianos A. Bariatric venous thromboembolism prophylaxis: an update on the literature. Expert Rev Hematol. 2019;12:763–71.
Ruiz-Tovar J, Llavero C. Thromboembolic prophylaxis for morbidly obese patients undergoing bariatric surgery. Adv Exp Med Biol. 2017;906:9–13.
Imberti D, Baldini E, Pierfranceschi MG, Nicolini A, Cartelli C, De Paoli M, et al. Prophylaxis of venous thromboembolism with low molecular weight heparin in bariatric surgery: a prospective, randomised pilot study evaluating two doses of parnaparin (BAFLUX Study). Obes Surg. 2014;24:284–91.
Author information
Authors and Affiliations
Contributions
WY and KM conceived and designed the idea, wrote, and drafted the manuscript. WY, YG, and KM led the data analysis, interpretation, and manuscript preparation with input from all authors. All authors contributed to the survey design, survey distribution, data collection, editing, and revising the manuscript, and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
MOK has been paid honoraria by Novo Nordisk for services provided/consultancy and Johnson and Johnson for educational activities. AT reports grants from Novo Nordisk, personal fees from Novo Nordisk, non-financial support from Novo Nordisk, personal fees from Eli Lilly, non-financial support from Eli Lilly, personal fees from Janssen, personal fees from AZ, non-financial support from AZ, non-financial support from Impeto medical, non-financial support from Resmed, non-financial support from Aptiva, personal fees from BI, non-financial support from BI, personal fees from BMS, non-financial support from BMS, personal fees from NAPP, non-financial support from NAPP, personal fees from MSD, non-financial support from MSD, personal fees from Nestle, personal fees from Gilead, grants from Sanofi, and personal fees from Sanofi outside the submitted work. AAT is currently an employee of Novo Nordisk. This work was performed before AAT became a Novo Nordisk employee and Novo Nordisk had no role in this project. KM has been paid honoraria by Ethicon, Medtronic, Gore, Olympus, and various NHS trusts for educational activities and mentoring colleagues through One Anastomosis Gastric Bypass. The other authors declare that they have no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yang, W., Abbott, S., Borg, CM. et al. Global variations in preoperative practices concerning patients seeking primary bariatric and metabolic surgery (PACT Study): A survey of 634 bariatric healthcare professionals. Int J Obes 46, 1341–1350 (2022). https://doi.org/10.1038/s41366-022-01119-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01119-x
This article is cited by
-
Preoperative Follow-up in Bariatric Surgery: Why They Give Up? Rate, Causes, and Economic Impact of Dropout
Obesity Surgery (2023)
-
Young-IFSO Bariatric/Metabolic Surgery Training and Education Survey
Obesity Surgery (2023)