Abstract
Background/Objectives
Hypothalamic obesity (HO) frequently occurs following suprasellar tumors from a combination of decreased energy expenditure and increased energy intake. Glucagon-like peptide-1 receptor agonist (GLP1RA) therapy is associated with increased satiety and energy expenditure. We hypothesized GLP1RA therapy in patients with HO would cause both lower energy intake and increased energy expenditure.
Subjects/Methods
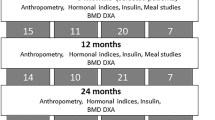
Forty-two patients aged 10-26 years (median 16 years) with HO with suprasellar tumors were randomized to GLP1RA (exenatide extended release once-weekly, ExQW, n = 23) or placebo (n = 19). Thirty seven (81%) patients completed the 36-week double-blind placebo-controlled trial. Total energy expenditure (TEE) was measured with doubly labeled water, physical activity was assessed with actigraphy, and intake was estimated with ad libitum buffet meal. Results are presented as adjusted mean between-group difference.
Results
As compared with treatment with placebo, treatment with ExQW was associated with decreased energy intake during a buffet meal (−1800 kJ (−430 kcal), 95% CI −3 184 to −418 kJ, p = 0.02). There were no significant differences in physical activity between groups. ExQW (vs. placebo) treatment was associated with a decrease in TEE (−695 kJ/day (−166 kcal/day), 95% CI −1 130 to −264 kJ/day, p < 0.01, adjusted for baseline TEE). The treatment effect was still significant after further adjustment for change in body composition (−372 kJ/day (−89 kcal/day), 95% CI −699 to −42 kJ/day, p = 0.04) or change in leptin (−695 kJ/day (−166 kcal/day), 95% CI −1 130 to −264 kJ/day, p < 0.01). This decrease in TEE occurred despite an increase in lean mass and fat mass (1.7 vs. 1.3 kg lean mass, p = 0.88 and 1.5 vs. 4.6 kg fat mass, p = 0.04, ExQW vs. placebo).
Conclusions
Treatment with a GLP1RA was associated with a decrease in food intake but also a decrease in TEE that was disproportionate to change in body composition.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Harz KJ, Muller HL, Waldeck E, Pudel V, Roth C. Obesity in patients with craniopharyngioma: assessment of food intake and movement counts indicating physical activity. J Clin Endocrinol Metab. 2003;88:5227–31.
Hoffmann A, Postma FP, Sterkenburg AS, Gebhardt U, Muller HL. Eating behavior, weight problems and eating disorders in 101 long-term survivors of childhood-onset craniopharyngioma. J Pediatr Endocrinol Metab. 2015;28:35–43.
Muller HL. Increased daytime sleepiness in patients with childhood craniopharyngioma and hypothalamic tumor involvement: review of the literature and perspectives. Int J Endocrinol. 2010;2010:519607.
Muller HL, Handwerker G, Wollny B, Faldum A, Sorensen N. Melatonin secretion and increased daytime sleepiness in childhood craniopharyngioma patients. J Clin Endocrinol Metab. 2002;87:3993–6.
Zegers D, Van Hul W, Van Gaal LF, Beckers S. Monogenic and complex forms of obesity: insights from genetics reveal the leptin-melanocortin signaling pathway as a common player. Crit Rev Eukaryot Gene Expr. 2012;22:325–43.
Muller HL, Gebhardt U, Etavard-Gorris N, Korenke E, Warmuth-Metz M, Kolb R, et al. Prognosis and sequela in patients with childhood craniopharyngioma - results of HIT-ENDO and update on KRANIOPHARYNGEOM 2000. Klin Padiatr. 2004;216:343–8.
Lomenick JP, Buchowski MS, Shoemaker AH. A 52-week pilot study of the effects of exenatide on body weight in patients with hypothalamic obesity. Obesity. 2016;24:1222–5.
Daubenbuchel AM, Ozyurt J, Boekhoff S, Warmuth-Metz M, Eveslage M, Muller HL. Eating behaviour and oxytocin in patients with childhood-onset craniopharyngioma and different grades of hypothalamic involvement. Pediatr Obes. 2019;14:e12527.
Westerterp KR. Doubly labelled water assessment of energy expenditure: principle, practice, and promise. Eur J Appl Physiol. 2017;117:1277–85.
Roth CL, Perez FA, Whitlock KB, Elfers C, Yanovski JA, Shoemaker AH. A phase 3 randomized clinical trial using a once-weekly glucagon-like peptide-1 receptor agonist in adolescents and young adults with hypothalamic obesity. Diabetes Obes Metab. 2020;23:363–73.
Schoeller DA, Schoeller DA. Validation of habitual energy intake. Public Health Nutr. 2002;5:883–8.
Black AE, Prentice AM, Coward WA. Use of food quotients to predict respiratory quotients for the doubly-labelled water method of measuring energy expenditure. Hum Nutr Clin Nutr. 1986;40:381–91.
Racette SB, Schoeller DA, Luke AH, Shay K, Hnilicka J, Kushner RF. Relative dilution spaces of 2H- and 18O-labeled water in humans. Am J Physiol. 1994;267:E585–90.
Tracy DJ, Xu Z, Choi L, Acra S, Chen KY, Buchowski MS. Separating bedtime rest from activity using waist or wrist-worn accelerometers in youth. PLoS One. 2014;9:e92512.
Vanl CM, Okely AD, Batterham MJ, Hinkley T, Ekelund U, Brage S, et al. Wrist accelerometer cut points for classifying sedentary behavior in children. Med Sci Sports Exerc. 2017;49:813–22.
Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43:357–64.
Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the children’s eating behaviour questionnaire. J Child Psychol Psychiatry. 2001;42:963–70.
Dykens EM, Maxwell MA, Pantino E, Kossler R, Roof E. Assessment of hyperphagia in Prader-Willi syndrome. Obesity. 2007;15:1816–26.
Abuzzahab MJ, Roth CL, Shoemaker AH. Hypothalamic obesity: prologue and promise. Horm Res Paediat. 2019;91:128–36.
Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87:1409–39.
Lockie SH, Heppner KM, Chaudhary N, Chabenne JR, Morgan DA, Veyrat-Durebex C, et al. Direct control of brown adipose tissue thermogenesis by central nervous system glucagon-like peptide-1 receptor signaling. Diabetes. 2012;61:2753–62.
Beiroa D, Imbernon M, Gallego R, Senra A, Herranz D, Villarroya F, et al. GLP-1 agonism stimulates brown adipose tissue thermogenesis and browning through hypothalamic AMPK. Diabetes. 2014;63:3346–58.
Perez FA, Elfers C, Yanovski JA, Shoemaker AH, Abuzzahab MJ, Roth CL. MRI measures of hypothalamic injury are associated with glucagon-like peptide-1 receptor agonist treatment response in people with hypothalamic obesity. Diabetes Obes Metab. 2021;23:1532–41.
Hill RJ, Davies PS. The validity of self-reported energy intake as determined using the doubly labelled water technique. Br J Nutr. 2001;85:415–30.
Fjalldal S, Holmer H, Rylander L, Elfving M, Ekman B, Osterberg K, et al. Hypothalamic involvement predicts cognitive performance and psychosocial health in long-term survivors of childhood craniopharyngioma. J Clin Endocrinol Metab. 2013;98:3253–62.
Wei Q, Li L, Chen JA, Wang SH, Sun ZL. Exendin-4 improves thermogenic capacity by regulating fat metabolism on brown adipose tissue in mice with diet-induced obesity. Ann Clin Lab Sci. 2015;45:158–65.
Heppner KM, Marks S, Holland J, Ottaway N, Smiley D, Dimarchi R, et al. Contribution of brown adipose tissue activity to the control of energy balance by GLP-1 receptor signalling in mice. Diabetologia. 2015;58:2124–32.
Tomas E, Stanojevic V, McManus K, Khatri A, Everill P, Bachovchin WW, et al. GLP-1(32-36)amide pentapeptide increases basal energy expenditure and inhibits weight gain in obese mice. Diabetes. 2015;64:2409–19.
Rosenbaum M, Leibel RL. Adaptive thermogenesis in humans. Int J Obes. 2010;34:S47–55.
Rosenbaum M, Leibel RL. Models of energy homeostasis in response to maintenance of reduced body weight. Obesity. 2016;24:1620–9.
Rosenbaum M, Goldsmith R, Bloomfield D, Magnano A, Weimer L, Heymsfield S, et al. Low-dose leptin reverses skeletal muscle, autonomic, and neuroendocrine adaptations to maintenance of reduced weight. J Clin Invest. 2005;115:3579–86.
DeLany JP, Kelley DE, Hames KC, Jakicic JM, Goodpaster BH. Effect of physical activity on weight loss, energy expenditure, and energy intake during diet induced weight loss. Obesity. 2014;22:363–70.
Unick JL, Gaussoin SA, Hill JO, Jakicic JM, Bond DS, Hellgren M, et al. Objectively assessed physical activity and weight loss maintenance among individuals enrolled in a lifestyle intervention. Obesity. 2017;25:1903–9.
Author information
Authors and Affiliations
Contributions
CLR, MJA, and AHS performed the study as investigators. HSJ supervised the nutrient analysis. MB analyzed actigraphy and DLW data. AHS and JCS completed the statistical analysis and created figures and tables. CE reviewed the analysis and provided data management. AHS wrote the first manuscript draft. All authors participated in manuscript editing and final approval.
Corresponding author
Ethics declarations
Competing interests
Astra Zeneca supported the study by providing the active drug and matching placebo. This study was supported by R01DK104936 (CLR, MJA and AHS) from the National Institute of Diabetes and Digestive and Kidney Diseases and CTSA award No. UL1 TR002243 from the National Center for Advancing Translational Sciences. AHS has consulted for Rhythm Pharmaceuticals, Radius Inc., and Saniona A/S on studies of obesity. JAY reports receiving grant support from the Intramural Research Program of NICHD, NIH, as well as grants from Hikma Pharmaceuticals, Soleno Therapeutics, and Rhythm Pharmaceuticals, for studies of obesity.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shoemaker, A.H., Silver, H.J., Buchowski, M. et al. Energy balance in hypothalamic obesity in response to treatment with a once-weekly GLP-1 receptor agonist. Int J Obes 46, 623–629 (2022). https://doi.org/10.1038/s41366-021-01043-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-01043-6
This article is cited by
-
Hypothalamic syndrome
Nature Reviews Disease Primers (2022)