Abstract
Background/Objective
Prevalence of pre-pregnancy obesity and excessive gestational weight gain (GWG) are higher among women of color with low SES. Dysregulation of the Hypothalamic-Pituitary-Adrenal (HPA) axis and its end-product, cortisol, during pregnancy is hypothesized to be associated with excessive GWG. However, past studies have produced inconsistent findings and often did not include health disparities populations. This study examined the association between pre-pregnancy body mass index (BMI), third trimester diurnal cortisol, and GWG in low-income, predominantly Hispanic women.
Subjects/Methods
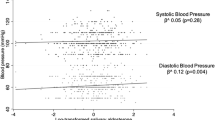
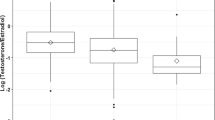
The MADRES study is an ongoing prospective cohort study of primarily Hispanic, low-income pregnant women and their children in Los Angeles, California. Data from 176 participants were included in this study. Total cortisol secretion (area under the curve, AUC) was quantified using four salivary cortisol samples (awakening, 30 min after awakening, afternoon, and bedtime) that were collected at home on one day during the third trimester of pregnancy. Moderation of the association between total cortisol and GWG by pre-pregnancy BMI was tested using multiple linear regression with a multiplicative interaction term.
Results
There was no association between total cortisol secretion and GWG overall (p = 0.82), but the association between total cortisol and GWG was stronger for women with class 1 pre-pregnancy obesity compared to women with normal pre-pregnancy BMI (interaction term p = 0.04).
Conclusions
Results suggest that obesity status before pregnancy may be exacerbating the physiological impact of cortisol on GWG.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Weight Gain During Pregnancy. Committee Opinion No. 548. 2013.
Deputy N, Sharma A, Kim S, Hinkle S. Prevalence and characteristics associated with gestational weight gain adequacy. Obs Gynecol. 2016;1.
Ali Z, Nilas L, Ulrik CS. Excessive gestational weight gain in first trimester is a risk factor for exacerbation of asthma during pregnancy: a prospective study of 1283 pregnancies. J Allergy Clin Immunol. 2018. https://doi.org/10.1016/j.jaci.2017.03.040.
Jensen DM, Ovesen P, Beck-Nielsen H, Mølsted-Pedersen L, Sørensen B, Vinter C, et al. Gestational weight gain and pregnancy outcomes in 481 obese glucose-tolerant women. Diabetes Care. 2005. https://doi.org/10.2337/diacare.28.9.2118.
Van Lieshout RJ, Taylor VH, Boyle MH. Pre-pregnancy and pregnancy obesity and neurodevelopmental outcomes in offspring: a systematic review. Obes Rev. 2011;12:548–59.
Kubo A, Ferrara A, Brown SD, Ehrlich SF, Tsai AL, Quesenberry CP, et al. Perceived psychosocial stress and gestational weight gain among women with gestational diabetes. PLoS ONE. 2017;12:1–11.
Kominiarek MA, Grobman W, Adam E, Buss C, Culhane J, Entringer S, et al. Stress during pregnancy and gestational weight gain. J Perinatol. 2018;38:462–7.
Cheney BDA. Examining the relationship between exercise, cortisol awakening response, diurnal cortisol, and mood a dissertation submitted to the faculty of the College of Arts and Sciences in Candidacy for the Degree of Doctor of Clinical Psychology Chicago, Illi. 2017.
Incollingo Rodriguez AC, Epel ES, White ML, Standen EC, Seckl JR, Tomiyama AJ. Hypothalamic-pituitary-adrenal axis dysregulation and cortisol activity in obesity: a systematic review. Psychoneuroendocrinology. 2015;62:301–18.
Papadimitriou A, Priftis KN. Regulation of the hypothalamic-pituitary-adrenal axis. Neuroimmunomodulation. 2009;16:265–71.
Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–31.
Rotenberg S, Mcgrath JJ, Roy-gagnon M. Stability of the diurnal cortisol profile in children and adolescents. Psychoneuroendocrinology. 2012;37:1981–9.
Kirschbaum C, Hellhammer DH. Noise and stress - salivary cortisol as a non-invasive measure of Allostatic Load. Noise Health. 1999;2.
Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–31.
Kuras YI, Rohleder N, Fiksdal A, Thoma MV, Chen X, Gianferante D, et al. Blunted diurnal cortisol activity in healthy adults with childhood adversity. Front Hum Neurosci. 2017;11:1–8.
Pasquali R, Vicennati V. The abdominal obesity phenotype and insulin resistance are associated with abnormalities of the hypothalamic-pituitaryadrenal axis in humans. Horm Metab Res. 2000;32:521–5.
Björntorp P, Rosmond R. Obesity and cortisol. In: Nutrition. 2000. https://doi.org/10.1016/S0899-9007(00)00422-6.
Allolio B, Hoffmann J, Linton EA, Winkelmann W, Kusche M, Schulte HM. Diurnal salivary cortisol patterns during pregnancy and after delivery: relationship to plasma corticotropin-releasing-hormone. Clin Endocrinol. 1990: 279–89.
Jung C, Ho JT, Torpy DJ, Rogers A, Doogue M, Lewis JG, et al. A longitudinal study of plasma and urinary cortisol in pregnancy and postpartum. J Clin Endocrinol Metab. 2011;96:1533–40.
Mustonen P, Karlsson L, Scheinin NM, Kortesluoma S, Coimbra B, Rodrigues AJ, et al. Hair cortisol concentration (HCC) as a measure for prenatal psychological distress — a systematic review. Psychoneuroendocrinology. 2018;92:21–8.
Liggins GC. The role of cortisol in preparing the fetus for birth. Reprod Fertil Dev. 1994. https://doi.org/10.1071/RD9940141.
Li XQ, Zhu P, Myatt L, Sun K. Roles of glucocorticoids in human parturition: a controversial fact? Placenta. 2014;35:291–6.
Wright RJ, Fisher K, Chiu YHM, Wright RO, Fein R, Cohen S, et al. Disrupted prenatal maternal cortisol, maternal obesity, and childhood wheeze: insights into prenatal programming. Am J Respir Crit Care Med. 2013;187:1186–93.
Aubuchon-Endsley NL, Bublitz MH, Stroud LR. Pre-pregnancy obesity and maternal circadian cortisol regulation: moderation by gestational weight gain. Biol Psychol. 2014;102:38–43.
Mina TH, Denison FC, Forbes S, Stirrat LI, Norman JE, Reynolds RM. Associations of mood symptoms with ante-and postnatal weight change in obese pregnancy are not mediated by cortisol. 2015. https://doi.org/10.1017/S0033291715001087.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017-8. NCHS Data Brief 2020.
Walker LO, Hoke MM, Brown A. Risk factors for excessive or inadequate gestational weight gain among Hispanic women in a U.S.-Mexico border state. JOGNN. J Obstet Gynecol Neonatal Nurs. 2009;38:418–29.
Brawarsky P, Stotland NE, Jackson RA, Fuentes-Afflick E, Escobar GJ, Rubashkin N, et al. Pre-pregnancy and pregnancy-related factors and the risk of excessive or inadequate gestational weight gain. Int J Gynecol Obstet. 2005;91:125–31.
Bastain TM, Chavez T, Habre R, Girguis MS, Grubbs B, Toledo-Corral C, et al. Study design, protocol and profile of the maternal and developmental risks from environmental and social stressors (MADRES) pregnancy cohort: a prospective cohort study in predominantly low-income Hispanic Women in Urban Los Angeles. BMC Pregnancy Childbirth. 2019. https://doi.org/10.1186/s12884-019-2330-7.
O’Connor SG, Habre R, Bastain TM, Toledo-Corral CM, Gilliland FD, Eckel SP, et al. Within-subject effects of environmental and social stressors on pre- and post-partum obesity-related biobehavioral responses in low-income Hispanic women: protocol of an intensive longitudinal study. BMC Public Health. 2019;19:253.
Kudielka BM, Gierens A, Hellhammer DH, Wüst S, Schlotz W. Salivary cortisol in ambulatory assessment-some dos, some don’ts, and some open questions. Psychosom Med. 2012;74:418–31.
Stalder T, Kirschbaum C, Kudielka BM, Adam EK, Pruessner JC, Wüst S, et al. Assessment of the cortisol awakening response: Expert consensus guidelines. Psychoneuroendocrinology. 2016;63:414–32.
National Institute of Health. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults.
Koren G, Boskovic R, Hard M, Maltepe C, Navioz Y, Einarson A. Motherisk - PUQE (pregnancy-unique quantification of emesis and nausea) scoring system for nausea and vomiting of pregnancy. In: American Journal of Obstetrics and Gynecology. 2002. https://doi.org/10.1067/mob.2002.123054.
SAS. SAS/STAT® 9.2 User’s Guide. 2008.
Montgomery DC, Peck EA, Vining GG. Introduction to linear regression analysis. John Wiley & Sons, 2021.
Peterson AK, Toledo-Corral CM, Chavez TA, Naya CH, Johnson M, Eckel SP, et al. Prenatal maternal cortisol levels and infant birth weight in a predominately low-income hispanic cohort. Int J Environ Res Public Health. 2020;17:1–13.
Peckett AJ, Wright DC, Riddell MC. The effects of glucocorticoids on adipose tissue lipid metabolism. Metabolism. 2011;60:1500–10.
Kominiarek MA, Peaceman AM. Gestational weight gain. Am J Obstet Gynecol. 2017;217:642–51.
Stirrat LI, O’Reilly JR, Barr SM, Andrew R, Riley SC, Howie AF, et al. Decreased maternal hypothalamic-pituitary-adrenal axis activity in very severely obese pregnancy: Associations with birthweight and gestation at delivery. Psychoneuroendocrinology. 2016. https://doi.org/10.1016/j.psyneuen.2015.09.019.
Wright RJ, Fisher K, Chiu Y-HM, Wright RO, Fein R, Cohen S, et al. Disrupted prenatal maternal cortisol, maternal obesity, and childhood wheeze insights into prenatal programming. Am J Respir Crit Care Med. 2013;187:1186–93.
Vicennati V, Garelli S, Rinaldi E, Di Dalmazi G, Pagotto U, Pasquali R. Cross-talk between adipose tissue and the HPA axis in obesity and overt hypercortisolemic states. Horm Mol Biol Clin Investig. 2014;17:63–77.
Vicennati V. Response of the hypothalamic-pituitary-adrenocortical axis to high-protein/fat and high-carbohydrate meals in women with different obesity phenotypes. J Clin Endocrinol Metab. 2002. https://doi.org/10.1210/jc.87.8.3984.
Pasquali R, Anconetani B, Chattat R, Biscotti M, Spinucci G, Casimirri F, et al. Hypothalamic-pituitary-adrenal axis activity and its relationship to the autonomic nervous system in women with visceral and subcutaneous obesity: effects of the corticotropin-releasing factor/arginine-vasopressin test and of stress. Metabolism. 1996. https://doi.org/10.1016/S0026-0495(96)90290-5.
Moisiadis VG, Matthews SG. Glucocorticoids and fetal programming part 1: outcomes. Nat Rev Endocrinol. 2014;10:391–402.
McDonald SD, Han Z, Mulla S, Beyene J. Overweight and obesity in mothers and risk of preterm birth and low birth weight infants: systematic review and meta-analyses. BMJ. 2010;341:187.
Gaudet L, Ferraro ZM, Wen SW, Walker M. Maternal obesity and occurrence of fetal macrosomia: a systematic review and meta-analysis. Biomed Res Int. 2014; 2014. https://doi.org/10.1155/2014/640291.
Cedergren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol. 2004. https://doi.org/10.1097/01.AOG.0000107291.46159.00.
Marchi J, Berg M, Dencker A, Olander EK, Begley C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev. 2015. https://doi.org/10.1111/obr.12288.
Cheng C-Y, Pickler RH, Zijlmans MAC, Korpela K, Riksen-Walraven JMA, de Vos WM, et al. NIH Public Access. Psychoneuroendocrinology. 2010;34:60–7.
Cheng C-Y, Pickler RH. Maternal psychological well-being and salivary cortisol in late pregnancy and early post-partum. Stress Heal. 2010;26:215–24.
De Weerth C, Buitelaar JK, Beijers R. Infant cortisol and behavioral habituation to weekly maternal separations: links with maternal prenatal cortisol and psychosocial stress. Psychoneuroendocrinology. 2013;38:2863–74.
Gilles M, Otto H, Wolf IAC, Scharnholz B, Peus V, Schredl M, et al. Maternal hypothalamus-pituitary-adrenal (HPA) system activity and stress during pregnancy: effects on gestational age and infant’s anthropometric measures at birth. Psychoneuroendocrinology. 2018;94:152–61.
Monk C, Feng T, Lee S, Krupska I, Champagne FA, Tycko B. Distress during pregnancy: epigenetic regulation of placenta glucocorticoid-related genes and fetal neurobehavior. Am J Psychiatry. 2016;173:705–13.
De Weerth C, Buitelaar JK. Physiological stress reactivity in human pregnancy - a review. Neurosci Biobehav Rev. 2005;29:295–312.
Adam EK, Kumari M. Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology. 2009. https://doi.org/10.1016/j.psyneuen.2009.06.011.
Saxbe DE. A field (researcher’s) guide to cortisol: tracking HPA axis functioning in everyday life. Health Psychol Rev. 2008;2:163–90.
Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39:263–72.
Acknowledgements
We want to thank the MADRES study families, nurses, midwives, doctors, and staff at each of our study sites and our MADRES study team without whom this study would not have been possible.
Funding
This work was supported by the Maternal and Developmental Risks from Environmental and Social Stressors (MADRES) Center (grant #s P50MD015705, P50ES026086, 83615801–0) funded by the National Institute of Environmental Health Sciences, the National Institute for Minority Health and Health Disparities and the Environmental Protection Agency; the Southern California Environmental Health Sciences Center (grant # P30ES007048) funded by the National Institute of Environmental Health Sciences; and the Lifecourse Approach to Developmental Repercussions of Environmental Agents on Metabolic and Respiratory health (LA DREAMERs) (grant #s UH3OD023287) funded by the National Institutes of Health Office of the Director ECHO Program. The first author was funded by the National Heart, Lung, and Blood Institute’s Predoctoral Training Fellowship [grant # F31HL154716]. The funding agencies had no role in the design of the study, the collection, analysis, or interpretation of data or in the writing of the paper.
Author information
Authors and Affiliations
Contributions
Conceptualization: CVB, TMB, CHN, GFD; Data curation: CHN, AKP, TC; Formal analysis: CHN; Funding acquisition; CVB, TMB, GFD; Investigation: CVB, TMB, GFD; Methodology: BHG, CVB, DL, SPE, NL, TMB, CMT-C, GFD; Project administration: CVB, TMB; Resources: CVB, TMB, GFD; Software: CHN, TC, AKP; Supervision: CVB, TMB, GFD; Validation: CHN, AKP; Visualization: CHN; Writing—original draft: CHN; Writing—review & editing: CVB, TMB, GFD, AKP, TC, CMT-C, SPE, BHG, DL, NL. All authors provided critical feedback and helped shape the research, analysis and paper. All authors approved the final paper as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Naya, C.H., Toledo-Corral, C.M., Chavez, T. et al. Third trimester cortisol is positively associated with gestational weight gain in pregnant women with class one obesity. Int J Obes 46, 366–373 (2022). https://doi.org/10.1038/s41366-021-01009-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-01009-8