Abstract
Background
Growing evidence suggests that prenatal alcohol exposure (PAE) has the potential to impact on a wide range of physical outcomes in offspring, including metabolism and body composition, although the evidence to-date is primarily from preclinical studies. The current clinical study examined the association between heavy PAE and indirect measures of adiposity in adolescence.
Methods
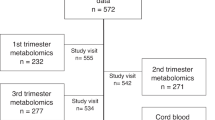
Analyses drew on data from the Longitudinal Study of Australian Children, a national prospective cohort of children and their families from birth to adolescence. Participants included children with heavy PAE (≥70 g/week; n = 46), measured via maternal self-report of alcohol use during pregnancy and a comparison group of children without any PAE (n = 782), frequency matched on sex, ethnicity and socio-economic position. Body mass index (BMI) z-scores, waist-to-height ratios and proportion overweight/obese were calculated from height, weight and waist circumference measured at age 12–13 years. Two (PAE) × two (sex) ANCOVA and logistic regression models were performed, controlling for matching variables, adolescent age, pubertal status and birthweight; maternal age at birth and smoking during pregnancy.
Results
Female adolescents with heavy PAE during late pregnancy had significantly higher BMI z-scores (M = 0.75, SD = 0.69) and proportion overweight/obese (38.5%) than females not exposed to any prenatal alcohol (M = 0.29, SD = 1.07, P = 0.04; 23.8%, P = 0.03, respectively). There was no significant effect of heavy PAE on male adolescent BMI z-scores and proportion overweight/obese or adolescent waist-to-height ratios (all P > 0.05).
Conclusions
Heavy PAE had a sex-specific effect on measures of adiposity in early adolescence, with girls more likely to have increased BMI and overweight/obesity status. Further longitudinal follow-up of children exposed to PAE is required to confirm if maternal alcohol consumption is a risk factor for later life obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Australian Bureau of Statistics. National Health Survey: First results. Australia 2017-2019. 4364.0.55.001. Canberra, ACT:ABS; 2018.
Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;6:CD012651.
Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–25.
Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385:2510–20.
Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days: a systematic review. Am J Prev Med. 2016;50:761–79.
Barker DJP. The origins of the developmental origins theory. J Intern Med. 2007;261:412–7.
Bailey BA, Sokol RJ. Prenatal alcohol exposure and miscarriage, stillbirth, preterm delivery, and sudden infant death syndrome. Alcohol Res Health. 2011;34:86–91.
Mattson SN, Bernes GA, Doyle LR. Fetal alcohol spectrum disorders: a review of the neurobehavioral deficits associated with prenatal alcohol exposure. Alcohol Clin Exp Res. 2019;43:1046–62.
Bower C, Elliott EJ, Zimmet M, Doorey J, Wilkins A, Russell V, et al. Australian guide to the diagnosis of foetal alcohol spectrum disorder: a summary. Journal of paediatrics and child health. 2017;53:1021–3.
Hoyme HE, Kalberg WO, Elliott AJ, Blankenship J, Buckley D, Marais AS, et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;138:e20154256.
Akison LK, Moritz KM, Reid N. Adverse reproductive outcomes associated with fetal alcohol exposure: a systematic review. Reproduction. 2019;157:329–43.
Akison LK, Reid N, Wyllie M, Moritz KM. Adverse health outcomes in offspring associated with fetal alcohol exposure: a systematic review of clinical and preclinical studies with a focus on metabolic and body composition outcomes. Alcohol Clin Exp Res. 2019;43:1324–43.
Reid N, Akison LK, Hoy W, Moritz KM. Adverse health outcomes associated with fetal alcohol exposure: a systematic review focused on cardio–renal outcomes. J Stud Alcohol Drugs. 2019;80:515–23.
Reid N, Moritz KM, Akison LK. Adverse health outcomes associated with fetal alcohol exposure: a systematic review focused on immune-related outcomes. Pediatr Allergy Immunol. 2019;30:698–707.
Amos-Kroohs RM, Fink BA, Smith CJ, Chin L, Van Calcar SC, Wozniak JR, et al. Abnormal eating behaviors are common in children with fetal alcohol spectrum disorder. J Pediatr. 2016;169:194–200.
Carter RC, Jacobson JL, Molteno CD, Jiang H, Meintjes EM, Jacobson SW, et al. Effects of heavy prenatal alcohol exposure and iron deficiency anemia on child growth and body composition through age 9 years. Alcohol Clin Exp Res. 2012;36:1973–82.
Fuglestad AJ, Boys CJ, Chang PN, Miller BS, Eckerle JK, Deling L, et al. Overweight and obesity among children and adolescents with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2014;38:2502–8.
Klug MG, Burd L, Martsolf JT, Ebertowski M. Body mass index in fetal alcohol syndrome. Neurotoxicol Teratol. 2003;25:689–96.
Spohr H-L, Willms J, Steinhausen H-C. Fetal alcohol spectrum disorders in young adulthood. J Pediatr. 2007;150:175–9.
Werts RL, Van Calcar SC, Wargowski DS, Smith SM. Inappropriate feeding behaviors and dietary intakes in children with fetal alcohol spectrum disorder or probable prenatal alcohol exposure. Alcohol Clin Exp Res. 2014;38:871–8.
Popova S, Lange S, Probst C, Gmel G, Rehm J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e290–9.
Australian Institute of Health and Welfare. National Drug Strategy Household Survey detailed report 2013. Drug statistics series no. 28. Cat. no. PHE 183. Canberra: AIHW; 2014.
Muggli E, O’Leary C, Donath S, Orsini F, Forster D, Anderson PJ, et al. “Did you ever drink more?” A detailed description of pregnant women’s drinking patterns. BMC Public Health. 2016;16:683.
Sanson A, Nicholson J, Ungerer J, Zubrick S, Wilson K, Ainley J, et al. Introducing the Longitudinal Study of Australian Children: LSAC discussion paper no. 1. Melbourne: AIFS; 2002.
Sanson A, Johnstone R. ‘Growing up in Australia’ takes its first steps. Family Studies. 2004;67:46–53.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27.
Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–92.
Bini V, Celi F, Berioli MG, Bacosi ML, Stella P, Giglio P, et al. Body mass index in children and adolescents according to age and pubertal stage. Eur J Clin Nutr. 2000;54:214–8.
Yu ZB, Han SP, Zhu GZ, Zhu C, Wang XJ, Cao XG, et al. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obes Rev. 2011;12:525–42.
Wake M, Maguire B. Children’s body mass index. In: Macquire B, Edwards B, editors. The Longitudinal Study of Australian Child Annual Statistical Report 2011. Melbourne: AIFS; 2012.
Ziauddeen N, Wilding S, Roderick PJ, Macklon S, Smith D, Chase D, et al. Predicting the risk of childhood overweight and obesity at 4–5 years using population-level pregnancy and early-life healthcare data. BMC Med. 2020;18:105.
Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: reliability, validity, and initial norms. J Youth Adolesc. 1988;17:117–33.
Blakemore TJ, Gibbings J, Strazdins L. Measurement of the socio-economic position of families. Aust Soc Pol. 2009;8:121–69.
IBM Corp. IBM SPSS Statistics for Windows, version 25.0. Armonk, NY: IBM Corp.; 2017.
Richardson JTE. Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev. 2011;6:135–47.
Sayal K. Commentary: light drinking in pregnancy: can a glass or two hurt? Int J Epidemiol. 2009;38:140–2.
Gijsen V, Fulga N, Bournissen FG, Garcia-Bournissen F, Koren G. Does light drinking during pregnancy improve pregnancy outcome? A critical commentary. Can J Clin Parmacol. 2008;15:e782–6.
Flak AL, Su S, Bertrand J, Denny CH, Kesmodel US, Cogswell ME. The association of mild, moderate, and binge prenatal alcohol exposure and child neuropsychological outcomes: a meta-analysis. Alcohol Clin Exp Res. 2014;38:214–26.
Hutchinson D, Moore EA, Breen C, Burns L, Mattick RP. Alcohol use in pregnancy: prevalence and predictors in the Longitudinal Study of Australian Children. Drug Alcohol Rev. 2013;32:475–82.
Gail MH Frequency Matching. In: Armitage P, Colton T, editors. Encyclopedia of biostatistics. Boston: John Wiley & Sons; 2005.
Cheung Y-B. Analysis of matched case-control data. J Clin Epidemiol. 2003;56:814.
Boslaugh S. Encyclopedia of epidemiology, vol. 1-2. Thousand Oaks, California: SAGE Publications; 2008.
Pearce N. Analysis of matched case-control studies. BMJ. 2016;352:i969.
Sjölander A, Greenland S. Ignoring the matching variables in cohort studies—when is it valid and why? Stat Med. 2013;32:4696–708.
Hutchinson D, Moore EA, Breen C, Burns L, Mattick RP. Alcohol use in pregnancy: prevalence and predictors in the Longitudinal Study of Australian Children. Drug Alcohol Rev. 2013;32:475–82.
National Health and Medical Research Council. Australian alcohol guidelines: health risks and benefits. Canberra, Australian Capital Territory: Commonwealth of Australia; 2001.
National Health and Medical Research Council. Australian guidelines to reduce health risks from drinking alcohol. Canberra, Australian Capital Territory: Commonwealth of Australia; 2009.
National Health and Medical Research Council, Australian Research Council, Universities Australia. Australian guidelines to reduce health risks from drinking alcohol. Canberra, Australian National Territory: National Health and Medical Research Council; 2020.
McMillen IC, Robinson JS. Developmental origins of the metabolic syndrome: prediction, plasticity, and programming. Physiol Rev. 2005;85:571–633.
Bekdash R, Zhang C, Sarkar D. Fetal alcohol programming of hypothalamic proopiomelanocortin system by epigenetic mechanisms and later life vulnerability to stress. Alcohol Clin Exp Res. 2014;38:2323–30.
Gangisetty O, Wynne O, Jabbar S, Nasello C, Sarkar DK. Fetal alcohol exposure reduces dopamine receptor D2 and increases pituitary weight and prolactin production via epigenetic mechanisms. PLoS ONE. 2015;10:e0140699.
O’Keeffe LM, Kearney PM, McCarthy FP, Khashan AS, Greene RA, North RA, et al. Prevalence and predictors of alcohol use during pregnancy: findings from international multicentre cohort studies. BMJ Open. 2015;5:e006323.
Aliyu MH, Wilson RE, Zoorob R, Brown K, Alio AP, Clayton H, et al. Prenatal alcohol consumption and fetal growth restriction: potentiation effect by concomitant smoking. Nicotine Tob Res. 2009;11:36–43.
Ratnasiri AWG, Gordon L, Dieckmann RA, Lee HC, Parry SS, Arief VN, et al. Smoking during pregnancy and adverse birth and maternal outcomes in California, 2007 to 2016. Am J Perinatol. 2019;37:1364–76.
Cho WK, Suh B-K. Catch-up growth and catch-up fat in children born small for gestational age. Korean J Pediatr. 2016;59:1–7.
Ibáñez L, Suárez L, Lopez-Bermejo A, Díaz M, Valls C, de Zegher F. Early development of visceral fat excess after spontaneous catch-up growth in children with low birth weight. J Clin Endocrinol Metab. 2008;93:925–8.
Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89:2548–56.
Symonds ME, Mostyn A, Pearce S, Budge H, Stephenson T. Endocrine and nutritional regulation of fetal adipose tissue development. J Endocrinol. 2003;179:293–9.
Clifford SA, Gillespie AN, Olds T, Grobler AC, Wake M. Body composition: population epidemiology and concordance in Australian children aged 11–12 years and their parents. BMJ Open. 2019;9:95–105.
Kalisch-Smith JI, Steane SE, Simmons DG, Pantaleon M, Anderson ST, Akison LK, et al. Periconceptional alcohol exposure causes female-specific perturbations to trophoblast differentiation and placental formation in the rat. Development. 2019;146:dev172205.
Jacobson SW, Chiodo LM, Sokol RJ, Jacobson JL. Validity of maternal report of prenatal alcohol, cocaine, and smoking in relation to neurobehavioral outcome. Pediatrics. 2002;109:815–25.
Hu Z, Tylavsky FA, Kocak M, Fowke JH, Han JC, Davis RL, et al. Effects of maternal dietary patterns during pregnancy on early childhood growth trajectories and obesity risk: The CANDLE study. Nutrients. 2020;12:465.
Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. 2019;16:e1002744.
Roblin L. Childhood obesity: food, nutrient, and eating-habit trends and influences. Appl Physiol Nutr Metab. 2007;32:635–45.
Acknowledgements
KMM was supported by the National Health and Medical Research Council (APP1078164). This paper uses unit record data from Growing Up in Australia: The Longitudinal Study of Australian Children (LSAC). The LSAC study is conducted in partnership between the Department of Social Services (DSS), the Australian Institute of Family Studies (AIFS) and the Australian Bureau of Statistics (ABS). The findings and views reported in this paper are those of the authors and should not be attributed to the DSS, AIFS, or the ABS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hayes, N., Reid, N., Akison, L.K. et al. The effect of heavy prenatal alcohol exposure on adolescent body mass index and waist-to-height ratio at 12–13 years. Int J Obes 45, 2118–2125 (2021). https://doi.org/10.1038/s41366-021-00884-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00884-5