Abstract
Background
According to the hypothesis of Gluckman and Hanson, mismatch between the developmental and postdevelopmental environments may lead to detrimental health impacts such as obesity. While several animal studies support the mismatch theory, there is a scarcity of evidence from human-based studies.
Objectives
Our study aims to examine whether a mismatch between the developmental and young-adult environments affect obesity in young adults of the Jerusalem Perinatal Family Follow-Up Study.
Methods
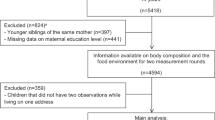
Data from The Jerusalem Perinatal Family Follow-Up Study birth cohort was used to characterize early and late environments using offspring and parental sociodemographic and lifestyle information at birth, age 32 (n = 1140) and 42 (n = 404). Scores characterizing the early and late environments were constructed using factor analysis. To assess associations of mismatch with obesity, regression models were fitted using the first factor of each environment and adiposity measures at age 32 and 42.
Results
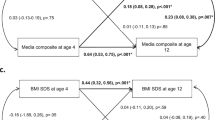
Having a stable non-beneficial environment at birth and young-adulthood was most strongly associated with increased adiposity, while a stable beneficial environment was most favorable. The transition from a beneficial environment at birth to a less beneficial environment at young-adulthood was associated with higher obesity measures, including higher BMI (β = 0.979; 95% CI: 0.029, 1.929), waist circumference (β = 2.729; 95% CI: 0.317, 5.140) and waist-hip ratio (β = 0.017; 95% CI: 0.004, 0.029) compared with those experiencing a beneficial environment at both time points. Transition from a less beneficial environment at birth to a beneficial environment at adulthood was also associated with higher obesity measurements (BMI −β = 1.116; 95% CI: 0.085, 2.148; waist circumference −β = 2.736; 95% CI: 0.215, 5.256).
Conclusions
This study provides some support for the mismatch hypothesis. While there is indication that an accumulation of the effects of the non-beneficial environment has the strongest detrimental impact on obesity outcomes, our results also indicate that a mismatch between the developmental and later environments may result in maladaptation of the individual leading to obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Almond D, Currie J. Killing Me Softly: The Fetal Origins Hypothesis. J Econ Perspect. 2011;25:153–72. https://doi.org/10.1038/jid.2014.371
World Health Organization (WHO). Obesity and Overweight. 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
OECD Health Indicators. Health at a Glance 2017. https://read.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2017_health_glance-2017-8
Scott Yoshizawa R. The Barker hypothesis and obesity: connections for transdisciplinarity and social justice. Soc Theory Heal. 2012;10:348–67. https://doi.org/10.1057/sth.2012.11
Wu DM, Hong Y, Sun CA, Sung PK, Rao DC, Chu NF. Familial resemblance of adiposity-related parameters: results from a health check-up population in Taiwan. Eur J Epidemiol. 2003;18:221–6. https://doi.org/10.1023/A:1023337917377
Magnusson PKE, Rasmussen F. Familial resemblance of body mass index and familial risk of high and low body mass index. A study of young men in Sweden. Int J Obes. 2002;26:1225–31. https://doi.org/10.1038/sj.ijo.0802041
Hochner H, Friedlander Y, Calderon-Margalit R, Meiner M, Sagy Y, Avgil-Tsadok M, et al. Associations of maternal prepregnancy body mass index and gestational weight gain with adult offspring cardiometabolic risk factors: The Jerusalem Perinatal Family Follow-Up Study. Circulation. 2012;125:1381–9. https://doi.org/10.1161/CIRCULATIONAHA.111.070060
Nirmala A, Kanniammal C, Venkataraman P, Arulappan J. Predisposing factors associated with obesity among adolescents-A case control study. Biomed Res. 2018;29:3497–501. https://doi.org/10.4066/biomedicalresearch.29-18-1016
Vlismas K, Stavrinos V, Panagiotakos DB, Socio-economic status, dietary habits and health-related outcomes in various parts of the world: a review. Cent Eur J Public Health. 2009;17:55–63. http://www.ncbi.nlm.nih.gov/pubmed/19662821
Gustafsson PE, Persson M, Hammarström A. Socio-economic disadvantage and body mass over the life course in women and men: results from the Northern Swedish Cohort. Eur J Public Health. 2011;22:1–6. https://doi.org/10.1093/eurpub/ckr061
Barker DJP. The origins of the developmental origins theory. J Intern Med. 2007;261:412–7. https://doi.org/10.1111/j.1365-2796.2007.01809.x
Barker DJ. Maternal nutrition, fetal nutrition, and disease in later life. Nutrition. 1997;13:807–13. http://www.ncbi.nlm.nih.gov/pubmed/9290095
Barker DJ. In utero programming of chronic disease. Clin Sci. 1998;95:115–28. http://www.ncbi.nlm.nih.gov/pubmed/17587272
Hanson MA, Gluckman PD. Early developmental conditioning of later health and disease: physiology or pathophysiology? Physiol Rev. 2018;94:1027–76. https://doi.org/10.1152/physrev.00029.2013
Hanson M, Gluckman P. Commentary: developing the future: life course epidemiology, DOHaD and evolutionary medicine. Int J of Epidemiol. 2016;45. https://doi.org/10.1093/ije/dyw105
Hanson M, Gluckman P. Developmental origins of health and disease. Int J Gynaecol Obs. 2011;115:3–5. https://doi.org/10.1155/2012/838640
Gluckman P, Hanson M. Developmental plasticity and human disease: research directions. J Intern Med. 2007;261:461–71. https://doi.org/10.1111/j.1365-2796.2007.01802.x
Gluckman PD, Hanson MA. Developmental origins of disease paradigm: a mechanistic and evolutionary perspective. Pediatr Res. 2004;56:311–7. https://doi.org/10.1203/01.PDR.0000135998.08025.FB
Hanson MA, Gluckman PD. Developmental origins of health and disease: new insights. Basic Clin Pharmacol Toxicol. 2008;102:90–93. https://doi.org/10.1111/j.1742-7843.2007.00186.x
Gluckman PD, Hanson MA, Low FM. Evolutionary and developmental mismatches are consequences of adaptive developmental plasticity in humans and have implications for later disease risk. Philos Trans R Soc B Biol Sci. 2019;374:20180109. https://doi.org/10.1098/rstb.2018.0109
Gluckman PD, Hanson MA, Spencer HG, Bateson P. Environmental influences during development and their later consequences for health and disease: implications for the interpretation of empirical studies. Proc R Soc B. 2005;272:671–7. https://doi.org/10.1098/rspb.2004.3001
Gluckman P, Hanson M. Mismatch: Why Our World No Longer Fits Our Bodies. Oxford University Press; USA. 2006.
Desai M, Gayle D, Babu J, Ross MG. The timing of nutrient restriction during rat pregnancy/lactation alters metabolic syndrome phenotype. Am J Obstet Gynecol. 2007;196:555.e1–555.e7. https://doi.org/10.1016/j.ajog.2006.11.036
Desai M, Babu J, Ross MG. Programmed metabolic syndrome: prenatal undernutrition and postweaning overnutrition. Am J Physiol Integr Comp Physiol. 2007;293:R2306–R2314. https://doi.org/10.1152/ajpregu.00783.2006
Nielsen MO, Kongsted AH, Thygesen MP, Strathe AB, Caddy S, Quistorff B, et al. Late gestation undernutrition can predispose for visceral adiposity by altering fat distribution patterns and increasing the preference for a high-fat diet in early postnatal life. British Journal of Nutrition. 2017;2013:2098–110. https://doi.org/10.1017/S0007114512004199
Bispham J, Gopalakrishnan GS, Dandrea J, Wilson V, Budge H, Keisler DH, et al. Maternal endocrine adaptation throughout pregnancy to nutritional manipulation: consequences for maternal plasma leptin and cortisol and the programming of fetal adipose tissue development. Endocrinology. 2003;144:3575–85. https://doi.org/10.1210/en.2003-0320
Zambrano E, Bautista CJ, Deás M, Martínez-Samayoa PM, González-Zamorano M, Ledesma H, et al. A low maternal protein diet during pregnancy and lactation has sex- and window of exposure-specific effects on offspring growth and food intake, glucose metabolism and serum leptin in the rat. J Physiol. 2006;571:221–30. https://doi.org/10.1113/jphysiol.2005.100313
Bol VV, Delattre A-I, Reusens B, Raes M, Remacle C. Forced catch-up growth after fetal protein restriction alters the adipose tissue gene expression program leading to obesity in adult mice. Am J Physiol Regul Integr Comp Physiol. 2009;297:R291–9. https://doi.org/10.1152/ajpregu.90497.2008
Howie GJ, Sloboda DM, Vickers MH. Maternal undernutrition during critical windows of development results in differential and sex-specific effects on postnatal adiposity and related metabolic profiles in adult rat offspring. Br J Nutr. 2012;108:298–307. https://doi.org/10.1017/S000711451100554X
Jimenez-Chillaron JC, Hernandez-Valencia M, Lightner A, Faucette RR, Reamer C, Przybyla R, et al. Reductions in caloric intake and early postnatal growth prevent glucose intolerance and obesity associated with low birthweight. Diabetologia. 2006;49:1974–84. https://doi.org/10.1007/s00125-006-0311-7
Rooney BL, Mathiason MA, Schauberger CW. Predictors of obesity in childhood, adolescence, and adulthood in a birth cohort. Matern Child Health J. 2011;15:1166–75. https://doi.org/10.1007/s10995-010-0689-1
Koletzko B, Dodds P, Akerblom H, Ashwell M. Early Nutrition and Its Later Consequences: New Opportunities Perinatal Programming of Adult Health—EC Supported Research. Adv Exp Med Biol. 2005;569:1–12.
Stettler N, Kumanyika SK, Katz SH, Zemel BS, Stallings VA. Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am J Clin Nutr. 2003;77:1374–8. https://doi.org/10.1093/ajcn/77.6.1374
Li C, Goran MI, Kaur H, Nollen N, Ahluwalia JS. Developmental trajectories of overweight during childhood: Role of early life factors. Obesity. 2007;15:760–71. https://doi.org/10.1038/oby.2007.585
Demerath EW, Reed D, Choh AC, Soloway L, Lee M, Czerwinski SA, et al. Rapid postnatal weight gain and visceral adiposity in adulthood: the Fels Longitudinal Study. Obesity. 2009;17:2060–6. https://doi.org/10.1038/oby.2009.105
Taveras EM, Rifas-Shiman SL, Belfort MB, Kleinman KP, Oken E, Gillman MW. Weight Status in the First 6 Months of Life and Obesity at 3 Years of Age. Pediatrics. 2009;123:1177–83. https://doi.org/10.1542/peds.2008-1149
Robertson T, Benzeval M. Do mismatches between pre- and post-natal environments influence adult physiological functioning? PLoS One. 2014;9:1–7. https://doi.org/10.1371/journal.pone.0086953
Lawrence GM, Siscovick DS, Calderon-Margalit R, Enquobahrie DA, Granot-Hershkovitz E, Harlap S, et al. Cohort profile: The Jerusalem Perinatal Family Follow-Up Study. Int J Epidemiol. 2016;45:343–52. https://doi.org/10.1093/ije/dyv120
Harlap S, Davies AM, Deutsch L, Calderon-Margalit R, Manor O, Paltiel O, et al. The Jerusalem Perinatal Study cohort, 1964-2005: methods and a review of the main results. Paediatr Perinat Epidemiol. 2007;21:256–73. https://doi.org/10.1111/j.1365-3016.2007.00799.x
Savitsky B, Manor O, Friedlander Y, Burger A, Lawrence G, Calderon-Margalit R, et al. Associations of socioeconomic position in childhood and young adulthood with cardiometabolic risk factors: The Jerusalem Perinatal Family Follow-Up Study. J Epidemiol Community Health. 2016;71:43–51. https://doi.org/10.1136/jech-2014-204323
Manor O, Eisenbach Z, Friedlander Y, Kark JD. Educational differentials in mortality from cardiovascular disease among men and women: the Israel Longitudinal Mortality Study. Ann Epidemiol. 2004;14:453–60. http://www.ncbi.nlm.nih.gov/pubmed/15301781
Lawrence G, Shulman S, Hochner H, Sitlani CM, Burger A, Savitsky B, et al. Associations of Maternal Pre-pregnancy Body Mass Index and Gestational Weight Gain with Offspring Longitudinal Change In BMI. Obesity. 2014;22:1165–71. https://doi.org/10.1002/oby.20643.
Yeh H-C, Duncan BB, Schmidt MI, Wang N-Y, Brancati FL. Smoking, smoking cessation, and risk for type 2 diabetes mellitus: a cohort study. Ann Intern Med. 2010;152:10–17. http://www.ncbi.nlm.nih.gov/pubmed/20048267
Kyle UG, Bosaeus I, De Lorenzo AD, Ursula G, Deurenberg P, Elia M, et al. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr. 2004;23:1430–53.
Bartholomew D, Knott M, Moustaki I Latent Variable Models and Factor Analysis. Chichester, UK: John Wiley & Sons, Ltd. 2011. https://doi.org/10.1002/9781119970583
Everitt BS, Dunn G Exploratory Factor Analysis. In: Applied Multivariate Data Analysis. West Sussex, United Kingdom: John Wiley & Sons, Ltd; 2013:271–90. https://doi.org/10.1002/9781118887486.ch12
Heraclides A, Brunner E. Social mobility and social accumulation across the life course in relation to adult overweight and obesity: the Whitehall II study. J Epidemiol Community Heal. 2010;64:714–9. http://www.ncbi.nlm.nih.gov/pubmed/19737739
Karnehed NEK, Rasmussen F, Hemmingsson T, Tynelius P. Obesity in young adulthood is related to social mobility among Swedish men. Obesity. 2008;16:654–8. https://doi.org/10.1038/oby.2007.103
Bernardi JR, Goldani MZ, Pinheiro TV, Guimarães LSP, Bettiol H, Moura da Silva AA, et al. Gender and social mobility modify the effect of birth weight on total and central obesity. Nutr J. 2017;16:38. https://doi.org/10.1186/s12937-017-0260-7
Albrecht SS, Gordon-Larsen P. Socioeconomic gradients in body mass index (BMI) in US immigrants during the transition to adulthood: examining the roles of parental education and intergenerational educational mobility. J Epidemiol Community Health. 2014;68:842–8. https://doi.org/10.1136/jech-2014-203814
McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222. https://doi.org/10.1111/j.1749-6632.2009.05331.x
Noppe G, van den Akker ELT, de Rijke YB, Koper JW, Jaddoe VW, van Rossum EFC. Long-term glucocorticoid concentrations as a risk factor for childhood obesity and adverse body-fat distribution. Int J Obes. 2016;40:1503–9. https://doi.org/10.1038/ijo.2016.113
Assari S Race, intergenerational social mobility and stressful life events. Behav Sci. 2018;8. https://doi.org/10.3390/bs8100086
Blum A, Peleg A, Weinberg M. Anti-cytomegalovirus (CMV) IgG antibody titer in patients with risk factors to atherosclerosis. Clin Exp Med. 2003;3:157–60. https://doi.org/10.1007/s10238-003-0019-7
Lawrence GM, Friedlander Y, Calderon-Margalit R, Enquobahrie DA, Huang JY, Tracy RP, et al. Associations of social environment, socioeconomic position and social mobility with immune response in young adults: The Jerusalem Perinatal Family Follow-Up Study. BMJ Open. 2017;7:1–9. https://doi.org/10.1136/bmjopen-2017-016949
Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J. Life course epidemiology. J Epidemiol Community Heal. 2003;57:778–83. https://doi.org/10.1136/jech.57.10.778
Gluckman PD. Early life events and their consequences for later disease: a life history and evolutionary perspective. Am J Hum Biol. 2007;19:1–19. https://doi.org/10.1002/ajhb
Lillycrop KA, Burdge GC. Epigenetic mechanisms linking early nutrition to long term health. Best Pract Res Clin Endocrinol Metab. 2012;26:667–76. https://doi.org/10.1016/j.beem.2012.03.009
Godfrey KM, Lillycrop KA, Burdge GC, Gluckman PD, Hanson MA. Epigenetic mechanisms and the mismatch concept of the developmental origins of health and disease. Pediatr Res. 2007;61:5R–10R. http://www.pedresearch.org/pt/re/pedresearch/abstract.00006450-200705001-00002.htm
Borghol N, Suderman M, McArdle W, Racine A, Hallett M, Pembrey M, et al. Associations with early-life socio-economic position in adult DNA methylation. Int J Epidemiol. 2012;41:62–74. https://doi.org/10.1093/ije/dyr147
Lam LL, Emberly E, Fraser HB, Neumann SM, Chen E, Miller GE, et al. Factors underlying variable DNA methylation in a human community cohort. Proc Natl Acad Sci USA. 2012;109:17253–60. https://doi.org/10.1073/pnas.1121249109
Needham BL, Smith JA, Zhao W, Wang X, Mukherjee B, Kardia SLR, et al. Life course socioeconomic status and DNA methylation in genes related to stress reactivity and inflammation: The multi-ethnic study of atherosclerosis. Epigenetics. 2015;10:958–69. https://doi.org/10.1080/15592294.2015.1085139
Gluckman P, Beedle A, Buklijas T, Low F, Hanson M. Principles of Evolutionary Medicine. 2016. https://books.google.com/books?hl=en&lr=&id=ozzcCwAAQBAJ&oi=fnd&pg=PP1&ots=GiRU0nuVL8&sig=aCbzAPEp0jmekXkaDYifWS-4ypY. Accessed February 24, 2020.
Kuijper B, Hanson MA, Vitikainen EIK, Marshall HH, Ozanne SE, Cant MA, et al. Developing differences: early-life effects and evolutionary medicine. Philos Trans R Soc L B Biol Sci. 2019;374:1–7.
Wallingford J. Breastfeeding in the 21st century. Lancet. 2016;387:2087. https://doi.org/10.1016/S0140-6736(16)30547-5
Templin T, Cravo Oliveira Hashiguchi T, Thomson B, Dieleman J, Bendavid E. The overweight and obesity transition from the wealthy to the poor in low- and middle-income countries: A survey of household data from 103 countries. Popkin BM, ed. PLOS Med. 2019;16:e1002968. https://doi.org/10.1371/journal.pmed.1002968
Yodfat Y. The prevalence of cardiovascular disease in different ethnic and socioeconomic groups in Beit Shemesh, Israel. Isr J Med Sci. 1972;8:1685–94.
Halevi N A Brief Economic History of Modern Israel. https://eh.net/encyclopedia/a-brief-economic-history-of-modern-israel/. Accessed October 27, 2020.
Acknowledgements
We are grateful to the study participants, study coordinators, nurses, and laboratory staff who contributed to the successful completion of the data collection. This study was supported by NIH research grant R01HL088884 and by the Israeli Science Foundation grants No. 1252/07 and 1065/16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Savitsky, B., Manor, O., Lawrence, G. et al. Environmental mismatch and obesity in humans: The Jerusalem Perinatal Family Follow-Up Study. Int J Obes 45, 1404–1417 (2021). https://doi.org/10.1038/s41366-021-00802-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00802-9
This article is cited by
-
Metabolic and fecal microbial changes in adult fetal growth restricted mice
Pediatric Research (2024)