Abstract
Background/objectives
Weight bias among registered dietitians (RDs) is a concern and effective interventions to reduce weight bias are sparse. Our objective was to determine if a short, attribution theory-based online video intervention would reduce weight bias in RDs.
Subjects/methods
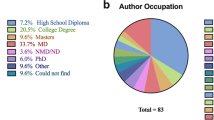
Dietitians from a nationally representative sample were recruited for a randomized, parallel-arm study with online surveys at pre-, post-intervention and 1-month follow-up. One hundred and forty-seven RDs who watched one of three videos embedded in an online survey from June to August 2019 were considered for the analysis. RDs were randomized to watch either the intervention, positive control, or negative control video. The primary outcome was the change in the “blame” component of the Anti-Fat Attitude Test (AFAT) from pre-to immediate post-intervention. Differences in changes in AFAT and Implicit Association Test (IAT) scores across treatment groups were assessed via linear models; multiple imputation were performed for missing data.
Results
Baseline demographics, AFAT and IAT scores of the 147 participants who watched a video were not significantly different between the study groups (p > 0.05). The intervention group’s AFAT-blame score reduced by an average of 0.05 between pre- and immediate post-intervention but was not statistically significant (p = 0.76, confidence intervals (CI) = −0.40, 0.30). Furthermore, there were no significant changes for AFAT-social, AFAT-physical subscores, and IAT within or between groups between pre- and immediate post-intervention (p > 0.05). Due to high attrition rates, the changes at 1-month follow-up are not reported.
Conclusions
This study was the first to explore the effectiveness of an online video intervention to reduce weight bias in RDs. This study was unable to detect a significant impact of a short, attribution theory-based video intervention on weight bias in practicing RDs and future larger studies are needed to confirm our findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–98.
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16:319–26.
Tomiyama AJ, Carr D, Granberg EM, Major B, Robinson E, Sutin AR, et al. How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Med. 2018;16:123.
Alberga AS, Pickering BJ, Alix Hayden K, Ball GD, Edwards A, Jelinski S, et al. Weight bias reduction in health professionals: a systematic review. Clin Obes. 2016;6:175–88.
Phelan SM, Dovidio JF, Puhl RM, Burgess DJ, Nelson DB, Yeazel MW, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity. 2014;22:1201–8.
Puhl R, Wharton C, Heuer C. Weight bias among dietetics students: implications for treatment practices. J Am Diet Assoc. 2009;109:438–44.
Swift JA, Hanlon S, El-Redy L, Puhl RM, Glazebrook C. Weight bias among UK trainee dietitians, doctors, nurses and nutritionists. J Hum Nutr Diet. 2013;26:395–402.
Schwartz MB, Chambliss HON, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–9.
Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes Relat Metab Disord. 2001;25:1525–31.
FUCE Jung, Luck-Sikorski C, Wiemers N, Riedel-Heller SG. Dietitians and nutritionists: stigma in the context of obesity. A systematic review. PLoS ONE. 2015;10:e0140276-e
Diversi TM, Hughes R, Burke KJ. The prevalence and practice impact of weight bias amongst Australian dietitians. Obes Sci Pract. 2016;2:456–65.
Oberrieder H, Walker R, Monroe D, Adeyanju M. Attitude of dietetics students and registered dietitians toward obesity. J Acad Nutr Diet. 1995;95:914–6.
Edelstein S, Silva N, Mancini L. Obesity bias among dietitians by using the fat people-thin people implicit association test. Top Clin Nutr. 2009;24:67–72.
Mason TB, Smith KE, Lavender JM. Stigma control model of dysregulated eating: a momentary maintenance model of dysregulated eating among marginalized/stigmatized individuals. Appetite. 2019;132:67–72.
Hunger JM, Major B, Blodorn A, Miller CT. Weighed down by stigma: how weight-based social identity threat contributes to weight gain and poor health. Soc Pers Psychol Compass. 2015;9:255–68.
Tomiyama AJ. Weight stigma is stressful. a review of evidence for the Cyclic Obesity/Weight-Based Stigma model. Appetite. 2014;82:8–15.
Schvey NA, Puhl RM, Brownell KD. The stress of stigma: exploring the effect of weight stigma on cortisol reactivity. Psychosom Med. 2014;76:156–62.
Tomiyama AJ, Epel ES, McClatchey TM, Poelke G, Kemeny ME, McCoy SK, et al. Associations of weight stigma with cortisol and oxidative stress independent of adiposity. Health Psychol. 2014;33:862–7.
Himmelstein MS, Incollingo Belsky AC, Tomiyama AJ. The weight of stigma: cortisol reactivity to manipulated weight stigma. Obesity. 2015;23:368–74.
McGuigan RD, Wilkinson JM. Obesity and healthcare avoidance: a systematic review. AIMS Public Health. 2015;2:56–63.
Alegria Drury CA, Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. J Am Acad Nurse Pract. 2002;14:554–61.
Sutin AR, Stephan Y, Terracciano A. Weight discrimination and risk of mortality. Psychol Sci. 2015;26:1803–11.
The Lancet Public Health. Addressing weight stigma. Lancet Public Health. 2019;4:e168.
Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805.
Fontaine KR, Cheskin LJ. Optimism and obesity treatment outcomes. J Clin Psychol. 1999;55:141–3.
Harvey EL, Summerbell CD, Kirk SFL, Hill AJ. Dietitians’ views of overweight and obese people and reported management practices. J Hum Nutr Diet. 2002;15:331–47.
Campbell K, Crawford D. Management of obesity: attitudes and practices of Australian dietitians. Int J Obes Relat Metab Disord. 2000;24:701–10.
Barr SI, Yarker KV, Levy-Milne R, Chapman GE. Canadian dietitians’ views and practices regarding obesity and weight management. J Hum Nutr Diet. 2004;17:503–12.
Lewis RJ, Cash TF, Bubb-Lewis C. Prejudice toward fat people: the development and validation of the antifat attitudes test. Obes Res. 1997;5:297–307.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. https://www.R-project.org/.
van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011;45:67.
Wijayatunga NN, Kim Y, Butsch WS, Dhurandhar EJ. The effects of a teaching intervention on weight bias among kinesiology undergraduate students. Int J Obes. 2019;43:2273–81.
Nutter S, Russell-Mayhew S, Alberga AS, Arthur N, Kassan A, Lund DE, et al. Positioning of weight bias: moving towards social justice. J Obes. 2016;2016:10.
Harris MB, Walters LC, Waschull S. Altering attitudes and knowledge about obesity. J Soc Psychol. 1991;131:881–4.
Persky S, Eccleston CP. Impact of genetic causal information on medical students’ clinical encounters with an obese virtual patient: health promotion and social stigma. Ann Behav Med. 2011;41:363–72.
Rukavina PB, Li W, Shen B, Sun H. A service learning based project to change implicit and explicit bias toward obese individuals in kinesiology pre-professionals. Obes Facts. 2010;3:117–26.
Swift JA, Tischler V, Markham S, Gunning I, Glazebrook C, Beer C, et al. Are anti-stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized control trial. Obes Facts. 2013;6:91–102.
Acknowledgements
This study was funded by startup funds from Texas Tech University, Lubbock, TX, USA. We acknowledge Sydney Han for her contribution to editing the videos.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wijayatunga, N.N., Bailey, D., Klobodu, S.S. et al. A short, attribution theory-based video intervention does not reduce weight bias in a nationally representative sample of registered dietitians: a randomized trial. Int J Obes 45, 787–794 (2021). https://doi.org/10.1038/s41366-021-00740-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00740-6