Abstract
Background
In the general population, body mass index (BMI = weight (kg)/(height (m))2) shows a U-shaped relation to mortality, which is attributable to a combination of an inverse association with fat-free mass index (FFMI) and a direct association with fat mass index (FMI). However, preceding changes in body composition related to diseases, health behaviors, or social conditions that are also influencing later mortality may confound these associations.
Objective
To examine associations of FFMI and FMI, adjusted for preceding changes in FFMI and FMI over a 6 years period, with all-cause mortality in a healthy general population.
Methods
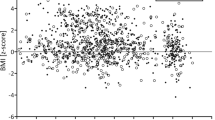
The study population was a random subset of adult Danes, participating in the Danish MONICA project; 989 men and 962 women, born 1922, 1932, 1942, and 1952, and examined in 1987–88 and 1993–94. They had no known major co-morbidities until start of follow-up in 1993–94, and were followed up for 18 years. Measures included height, weight, and bio-impedance, from which BMI, FFMI, and FMI were calculated, and information on educational level, smoking, alcohol drinking, leisure-time physical activity, which were obtained by questionnaires. We analyzed the relation between body composition and all-cause mortality by Cox proportional hazards model with splines, stratified by birth cohorts, and with adjustment for preceding changes in body composition and for the covariates including gender. We estimated hazard ratios (HR) with 95% confidence intervals (CI) relative to HR = 1.00 at the median values of BMI, FMI, and FFMI.
Results
During 18 years of follow-up, 286 men and 200 women died. BMI showed the well-known U-shaped association with mortality, and FMI was directly and FFMI inversely associated with mortality. Associations were not significantly modified by gender. Preceding changes in BMI, FMI, and FFMI were only weakly and not significantly associated with mortality. Associations for FMI and FFMI were monotonic, but curve-linear with a higher mortality above and below the respective median values of FMI and FFMI: at the 5th percentiles of FMI and FFMI, HRs were 0.80 (CI 0.57–1.13) and 2.01 (1.24–3.27), and at the 95th percentiles, HRs were 2.16 (1.38–3.38) and 0.81 (0.52–1.27), respectively.
Conclusions
In an apparently healthy general population, a large fat mass and a small fat-free mass are associated with greater risk of early mortality, also after adjusting for preceding changes in body composition, health behaviors, and educational level.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diab Endocrinol. 2018;6:944–53.
Allison DB, Faith MS, Heo M, Kotler DP. Hypothesis concerning the U-shaped relation between body mass index and mortality. Am J Epidemiol. 1997;146:339–49.
Allison DB, Zhu SK, Plankey M, Faith MS, Heo M. Differential associations of body mass index and adiposity with all-cause mortality among men in the first and second National Health and Nutrition Examination Surveys (NHANES I and NHANES II) follow-up studies. Int J Obes Relat Metab Disord. 2002;26:410–6.
Zhu S, Heo M, Plankey M, Faith MS, Allison DB. Associations of body mass index and anthropometric indicators of fat mass and fat free mass with all-cause mortality among women in the first and second National Health and Nutrition Examination Surveys follow-up studies. Ann Epidemiol. 2003;13:286–93.
Heitmann BL, Erikson H, Ellsinger BM, Mikkelsen KL, Larsson B. Mortality associated with body fat, fat-free mass and body mass index among 60-year-old Swedish men-a 22-year follow-up. The study of men born in 1913. Int J Obes Relat Metab Disord. 2000;24:33–7.
Bigaard J, Frederiksen K, Tjønneland A, Thomsen BL, Overvad K, Heitmann BL, et al. Body fat and fat-free mass and all-cause mortality. Obes Res. 2004;12:1042–9.
Lee DH, Giovannucci EL. Body composition and mortality in the general population: a review of epidemiologic studies. Exp Biol Med. 2018;243:1275–85.
Carslake D, Davey Smith G, Gunnell D, Davies N, Nilsen TIL, Romundstad P. Confounding by ill health in the observed association between BMI and mortality: evidence from the HUNT Study using offspring BMI as an instrument. Int J Epidemiol. 2018;47:760–70.
De Stefani FDC, Pietraroia PS, Fernandes-Silva MM, Faria-Neto J, Baena CP. Observational evidence for unintentional weight loss in all-cause mortality and major cardiovascular events: a systematic review and meta-analysis. Sci Rep. 2018;8:15447.
Heitmann BL. Body fat in the adult Danish population aged 35-65 years: an epidemiological study. Int J Obes. 1991;15:535–45.
World Health Organization. The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41:105–14.
World Health Organization. Measuring obesity—classification and description of anthropometric data. Report on a WHO consultation of the epidemiology of obesity. Warsaw 21–23 October 1987. Nutrition Unit document, EUR/ICP/NUT 123. Copenhagen: WHO; 1989.
Heitmann BL. Prediction of body water and fat in adult Danes from measurement of electrical impedance. A validation study. Int J Obes. 1990;14:789–802.
Cox DR. Regression models and life-tables. J R Stat Soc (B). 1972;34:187–220.
Korn EL, Graubard BI, Midthune. Time-to-event analysis of longitudinal follow-up of a survey: choise of the time-scale. Am J Epidemiol. 1997;145:72–80.
Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. New York: Springer; 2000.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. https://www.R-project.org/.
Wood SN. Thin-plate regression splines. J Royal Stat Soc (B). 2003;65:95–114.
Wood SN, Pya N, Saefken B. Smoothing parameter and model selection for general smooth models (with discussion). J Am Stat Assoc. 2016;111:1548–75.
Lee DH, Keum N, Hu FB, Orav EJ, Rimm EB, Willett WC, et al. Predicted lean body mass, fat mass, and all cause and cause specific mortality in men: prospective US cohort study. BMJ. 2018;362:k2575.
Mulasi U, Kuchnia AJ, Cole AJ, Earthman CP. Bioimpedance at the bedside: current applications, limitations, and opportunities. Nutr Clin Pract. 2015;30:180–93.
Tournadre A, Vial G, Capel F, Soubrier M, Boirie Y. Sarcopenia. Joint Bone Spine. 2019;86:309–14.
Afzal S, Tybjærg-Hansen A, Jensen GB, Nordestgaard BG. Change in body mass index associated with lowest mortality in Denmark, 1976–2013. JAMA. 2016;315:1989–96.
St-Onge MP. Relationship between body composition changes and changes in physical function and metabolic risk factors in aging. Curr Opin Clin Nutr Metab Care. 2005;8:523–8.
Ma C, Avenell A, Bolland M, Hudson J, Stewart F, Robertson C, et al. Effects of weight loss interventions for adults who are obese on mortality, cardiovascular disease, and cancer: systematic review and meta-analysis. BMJ. 2017;359:j4849.
Berentzen T, Sørensen TI. Effects of intended weight loss on morbidity and mortality: possible explanations of controversial results. Nutr Rev. 2006;64:502–7.
Karahalios A, English DR, Simpson JA. Change in body size and mortality: a systematic review and meta-analysis. Int J Epidemiol. 2017;46:526–46.
Kim YH, Kim SM, Han KD, Son JW, Lee SS, Oh SW, et al. Taskforce Team of the obesity fact sheet of the Korean Society for the Study of Obesity. Change in weight and body mass index associated with all-cause mortality in Korea: a nationwide longitudinal study. J Clin Endocrinol Metab. 2017;102:4041–50.
Allison DB, Zannolli R, Faith MS, Heo M, Pietrobelli A, VanItallie TB, et al. Weight loss increases and fat loss decreases all-cause mortality rate: results from two independent cohort studies. Int J Obes Relat Metab Disord. 1999;23:603–11.
Graf CE, Herrmann FR, Spoerri A, Makhlouf AM, Sørensen TIA, Ho S, et al. Impact of body composition changes on risk of all-cause mortality in older adults. Clin Nutr. 2016;35:1499–505.
Østergaard JN, Grønbaek M, Schnohr P, Sørensen TI, Heitmann BL. Combined effects of weight loss and physical activity on all-cause mortality of overweight men and women. int J Obes. 2010;34:760–9.
Heitmann BL, Hills AP, Frederiksen P, Ward LC. Obesity, leanness, and mortality: effect modification by physical activity in men and women. Obesity. 2009;17:136–42.
Bigaard J, Frederiksen K, Tjønneland A, Thomsen BL, Overvad K, Heitmann BL, et al. Waist circumference and body composition in relation to all-cause mortality in middle-aged men and women. Int J Obes. 2005;29:778–84.
Kim YH, Kim SM, Han KD, Jung JH, Lee SS, Oh SW, et al. Waist circumference and all-cause mortality independent of body mass index in Korean population from the National Health Insurance Health Check-up 2009–2015. J Clin Med. 2019;8:1–10.
Funding
The Parker Institute, Bispebjerg and Frederiksberg Hospital is supported by a core grant from the Oak Foundation (OCAY-13-309). The Novo Nordisk Foundation Center for Basic Metabolic is supported by The Novo Nordisk Foundation. Sources of funding had no role in the design, implementation, analysis, or interpretation of the data.
Author information
Authors and Affiliations
Contributions
Conceptualization: TIAS and BLH; study design: BLH; data collection: BLH; statistical analyses: PF; interpretation of results: TIAS, PF, and BLH; writing of first draft: TIAS; revision of the manuscript: TIAS, PF, and BLH; approval of the final version for submission: TIAS, PF, and BLH.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sørensen, T.I.A., Frederiksen, P. & Heitmann, B.L. Levels and changes in body mass index decomposed into fat and fat-free mass index: relation to long-term all-cause mortality in the general population. Int J Obes 44, 2092–2100 (2020). https://doi.org/10.1038/s41366-020-0613-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-0613-8
This article is cited by
-
Muscle distribution in relation to all-cause and cause-specific mortality in young and middle-aged adults
Journal of Translational Medicine (2023)
-
Body fat and risk of all-cause mortality: a systematic review and dose-response meta-analysis of prospective cohort studies
International Journal of Obesity (2022)
-
Prevalence of obesity and diabetes in older people with sarcopenia defined according to EWGSOP2 and FNHI criteria
Aging Clinical and Experimental Research (2022)
-
Instrumental variable analysis using offspring BMI in childhood as an indicator of parental BMI in relation to mortality
Scientific Reports (2021)