Abstract
Background
An association between sleep and obesity has been suggested in several studies, but many previous studies relied on self-reported sleep and on BMI as the only adiposity measure. Moreover, a relationship between weight loss history and attained sleep duration has not been thoroughly explored.
Design
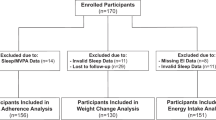
The study comprised of 1202 participants of the European NoHoW trial who had achieved a weight loss of ≥5% and had a BMI of ≥25 kg/m2 prior to losing weight. Information was available on objectively measured sleep duration (collected during 14 days), adiposity measures, weight loss history and covariates. Regression models were conducted with sleep duration as the explanatory variable and BMI, fat mass index (FMI), fat-free mass index (FFMI) and waist-hip ratio (WHR) as response variables. Analyses were conducted with 12-month weight loss, frequency of prior weight loss attempts or average duration of weight maintenance after prior weight loss attempts as predictors of measured sleep duration.
Results
After adjusting for physical activity, perceived stress, smoking, alcohol consumption, education, sex and age, sleep duration was associated to BMI (P < 0.001), with the highest BMI observed in the group of participants sleeping <6 h a day [34.0 kg/m2 (95% CI: 31.8–36.1)]. Less difference in BMI was detected between the remaining groups, with the lowest BMI observed among participants sleeping 8–<9 h a day [29.4 kg/m2 (95% CI: 28.8–29.9)]. Similar results were found for FMI (P = 0.008) and FFMI (P < 0.001). We found no association between sleep duration and WHR. Likewise, we found no associations between weight loss history and attained sleep duration.
Conclusion
In an overweight population who had achieved a clinically significant weight loss, short sleep duration was associated with higher BMI, with similar associations for fat and lean mass. We found no evidence of association between weight loss history and attained sleep duration.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
National Sleep Foundation. Sleep in America poll—adult sleep habits and styles. Washington, D.C.: National Sleep Foundation; 2005.
Currie A, Cappuccio FP, Stranges S, Taggart FM, Miller MA, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26.
Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep Med Rev. 2012;16:231–41.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring). 2008;106:643–53.
Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12:289–98.
Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLOS Med. 2004;1:e62.
Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6.
Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15:1456–62.
Knutson KL, Spiegel K, Penev P, Van CE. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11:163–78.
Liu C, Chen MS, Yu H. The relationship between obstructive sleep apnea and obesity hypoventilation syndrome: a systematic review and meta-analysis. Oncotarget. 2017;8:93168–78.
Anandam A, Akinnusi M, Kufel T, Porhomayon J, El-Solh AA. Effects of dietary weight loss on obstructive sleep apnea: a meta-analysis. Sleep Breath. 2013;17:227–34.
Greenburg DL, Lettieri CJ, Eliasson AH. Effects of surgical weight loss on measures of obstructive sleep apnea: a meta-analysis. Am J Med. 2009;122:535–42.
Nam S, Stewart KJ, Dobrosielski DA. Lifestyle intervention for sleep disturbances among overweight or obese individuals. Behav Sleep Med. 2016;14:343–50.
Kalra M, Mannaa M, Fitz K, Kumar S, Chakraborty R, Sheng X, et al. Effect of surgical weight loss on sleep architecture in adolescents with severe obesity. Obes Surg. 2008;18:675–9.
Andreeva VA, Torres MJ, Léger D, Bayon V, Gonzalez P, de Edelenyi FS, et al. Major change in body weight over 5-áyears and total sleep time: investigation of effect modification by sex and obesity in a large e-cohort. Int J Behav Med. 2017;24:493–500.
Schwartz AR, Patil SP, Laffan AM, Polotsky V, Schneider H, Smith PL. Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc Am Thorac Soc. 2008;5:185–92.
Davies RJ, Stradling JR. The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apnoea syndrome. Eur Respir J. 1990;3:509–14.
Schwab RJ, Pasirstein M, Pierson R, Mackley A, Hachadoorian R, Arens R, et al. Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med. 2003;168:522–30.
Sharp JT, Henry JP, Sweany SK, Meadows WR, Pietras RJ. Effects of mass loading the respiratory system in man. J Appl Physiol. 1964;19:959–66.
Parra MD, Martinez de Morentin BE, Alfredo MJ. Impact of weight loss on cortisol secretion in obese men with and without metabolic syndrome features. Nutr Metab Cardiovasc Dis. 2006;16:28–34.
Bjorntorp P, Rosmond R. Obesity and cortisol. Nutrition. 2000;16:924–36.
Fehm HL, Benkowitsch R, Kern W, Fehm-Wolfsdorf G, Pauschinger P, Born J. Influences of corticosteroids, dexamethasone and hydrocortisone on sleep in humans. Neuropsychobiology. 1986;16:198–204.
Scott SE, Duarte C, Encantado J, Evans EH, Harjumaa M, Heitmann BL, et al. The NoHoW protocol: a multicenter 2 × 2 factorial randomized controlled trial investigating an evidence-based digital toolkit for weight loss maintenance in European adults. BMJ Open. 2019;9:e029425.
Fitbit Charge 2. User Manual: Version 1.2. 2019. https://staticcs.fitbit.com/content/assets/help/manuals/manual_charge_2_en_US.pdf.
Fitbit Help: What should I know about sleep stages? 2019. https://help.fitbit.com/articles/en_US/Help_article/2163.
Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A, et al. Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas. 2006;27:921–33.
UNESCO Institute for Statistics. International Standard Classification of Education: ISCED 2011. UNESCO Institute for Statistics. Montreal. 2012.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96.
Gray DS, Bauer M. The relationship between body fat mass and fat-free mass. J Am Coll Nutr. 1991;10:63–8.
Bjorvatn B, Sagen IM, Øyane N, Waage S, Fetveit A, Fetveit A, et al. The association between sleep duration, body mass index and metabolic measures in the Hordaland Health Study. J Sleep Res. 2007;16:66–76.
Chaput JP, Després JP, Bouchard C, Tremblay A. Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Qubec family study. Obesity. 2007;15:253–61.
Singh M, DrakeCL, Roehrs T, Hudgel DW, Roth T. The association between obesity and short sleep duration: a population-based study. J Clin Sleep Med. 2005;1:357–63.
Zimberg IZ, Dâmaso A, Del Re M, Carneiro AM, de Sá Souza H, de Lira FS, et al. Short sleep duration and obesity: mechanisms and future perspectives. Cell Biochem Funct. 2012;30:524–9.
Kim K, Shin D, Jung GU, Lee D, Park SM. Association between sleep duration, fat mass, lean mass and obesity in Korean adults: the fourth and fifth Korea National Health and Nutrition Examination Surveys. J Sleep Res. 2017;26:453–60.
Baird J, Hill CM, Harvey NC, Crozier S, Robinson SM, Godfrey KM, et al. Duration of sleep at 3-áyears of age is associated with fat and fat-free mass at 4-áyears of age: the Southampton Women’s Survey. J Sleep Res. 2016;25:412–8.
Lane JM, Liang J, Vlasac I, Anderson SG, Bechtold DA, Bowden J, et al. Genome-wide association analyses of sleep disturbance traits identify new loci and highlight shared genetics with neuropsychiatric and metabolic traits. Nature Genet. 2016;49:274.
Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206.
Karasik D, Chou WC, Kiel DP, Hsu YH, Amin N, van-áDuijn CM, et al. Disentangling the genetics of lean mass. Am J Clin Nutr. 2019;109:276–87.
Valladares M, Obregón AM, Chaput JP. Association between genetic variants of the clock gene and obesity and sleep duration. J Physiol Biochem. 2015;71:855–60.
de Zambotti M, Goldstone A, Claudatos S, Colrain IM, Baker FC. A validation study of Fitbit Charge 2 compared with polysomnography in adults. Chronobiol Int. 2018;35:465–76.
Dahl AK, Reynolds CA. Accuracy of recalled body weight—a study with 20-years of follow-up. Obesity. 2013;21:1293–8.
Acknowledgements
The NoHoW study has received founding from the European Union’s Horizon 2020 Research and Innovation Programme (grant agreement number: 643309). The Parker Institute is supported by a core grant from the Oak Foundation (grant agreement number: OCAY-18-774-OFIL).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was conducted in accordance with the Helsinki Declaration. Ethical approval has been granted by local institutional ethics committees at the Universities of Leeds (17-0082; 27-Feb-2017), Lisbon (17/2016; 20-Feb-2017) and the Capital Region of Denmark (H-16030495; 8-Mar-2017).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Larsen, S.C., Horgan, G., Mikkelsen, ML.K. et al. Association between objectively measured sleep duration, adiposity and weight loss history. Int J Obes 44, 1577–1585 (2020). https://doi.org/10.1038/s41366-020-0537-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-0537-3
This article is cited by
-
Role of Sleep and Sleep Disorders in Cardiometabolic Risk: a Review and Update
Current Sleep Medicine Reports (2024)