Abstract
Background
Exercise is recognized to evoke multisystemic adaptations that, particularly in obese subjects, reduce body weight, improve glucometabolic control, counteract sarcopenia, and lower the risk of cardiometabolic diseases. Understanding the molecular and cellular mechanisms of exercise-induced benefits is of great interest due to the therapeutic implications against obesity.
Objectives and methods
The aim of the present study was to evaluate time-related changes in size distribution and cell origin of extracellular vesicles (EVs) in obese and normal-weight subjects who underwent a moderate-intensity exercise on a treadmill (at 60% of their VO2max). Blood samples were drawn before, immediately at the end of the exercise and during the postexercise recovery period (3 and 24 h). Circulating EVs were analyzed by a nanoparticle tracking analysis and flow cytometry after labeling with the following cell-specific markers: CD14 (monocyte/macrophage), CD61 (platelet), CD62E (activated endothelium), CD105 (total endothelium), SCGA (skeletal muscle), and FABP (adipose tissue).
Results
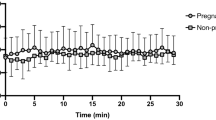
In all subjects, acute exercise reduced the release of total (i.e., 30–700 nm) EVs in circulation, predominantly EVs in the microvesicle size range (i.e., 130–700 nm EVs). The postexercise release of microvesicles was higher in normal-weight than obese subjects; after exercise, circulating levels of exosomes (i.e., 30–130 nm EVs) and microvesicles were, respectively, lower and higher in females than males. In all experimental subgroups (males vs. females and obese vs. normal-weight subjects), acute exercise reduced and increased, respectively, CD61 + and SCGA + EVs, being the effect on CD61 + EVs prolonged up to 24 h after the end of the test with subjects in resting conditions. Total EVs, exosomes, and CD61 + EVs were associated with HOMA-IR.
Conclusions
Though preliminary, the results of the present study show that a single bout of acute exercise modulates the release of EVs in circulation, which are tissue-, sex-, and BMI specific, suggesting that the exercise-related benefits might depend upon a complex interaction of tissue, endocrine, and metabolic factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets used and/or analyzed in the present study are available from the corresponding author on reasonable request.
References
Lin X, Zhang X, Guo J, Roberts CK, McKenzie S, Wu WC, et al. Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 2015;4:e002014.
Kasargod Prabhakar CR, Stewart R. Physical activity and mortality in patients with stable coronary heart disease. Curr Opin Cardiol. 2018;33:653–9.
Boniol M, Dragomir M, Autier P, Boyle P. Physical activity and change in fasting glucose and HbA1c: a quantitative meta-analysis of randomized trials. Acta Diabetol. 2017;54:983–91.
Pan B, Ge L, Xun YQ, Chen YJ, Gao CY, Han X, et al. Exercise training modalities in patients with type 2 diabetes mellitus: a systematic review and network meta-analysis. Int J Behav Nutr Phys Act. 2018;15:72.
Petridou A, Siopi A, Mougios V. Exercise in the management of obesity. Metabolism. 2019;92:163–9.
Lee DC, Shook RP, Drenowatz C, Blair SN. Physical activity and sarcopenic obesity: definition, assessment, prevalence and mechanism. Future Sci OA. 2016;2:FSO127.
Polyzos SA, Margioris AN. Sarcopenic obesity. Hormones. 2018;17:321–31.
Sartorio A, Lafortuna CL, Maffiuletti NA, Agosti F, Marazzi N, Rastelli F, et al. GH responses to two consecutive bouts of whole body vibration, maximal voluntary contractions or vibration alternated with maximal voluntary contractions administered at 2 h intervals in healthy adults. Growth Horm IGF Res. 2010;20:416–21.
Giunta M, Rigamonti AE, Agosti F, Patrizi A, Compri E, Cardinale M, et al. Combination of external load and whole body vibration potentiates the GH-releasing effect of squatting in healthy females. Horm Metab Res. 2013;45:611–6.
Rigamonti AE, Haenelt M, Bidlingmaier M, De Col A, Tamini S, Tringali G, et al. Obese adolescents exhibit a constant ratio of GH isoforms after whole body vibration and maximal voluntary contractions. BMC Endocr Disord. 2018;18:96.
Wannamethee SG, Atkins JL. Muscle loss and obesity: the health implications of sarcopenia and sarcopenic obesity. Proc Nutr Soc. 2015;74:405–12.
Rigamonti AE, De Col A, Tamini S, Cicolini S, Caroli D, De Micheli R, et al. Multidisciplinary integrated metabolic rehabilitation in elderly obese patients: effects on cardiovascular risk factors, fatigue and muscle performance. Nutrients. 2019;11:E1240.
Piccirillo R. Exercise-induced myokines with therapeutic potential for muscle wasting. Front Physiol. 2019;10:287.
Safdar A, Tarnopolsky MA. Exosomes as mediators of the systemic adaptations to endurance exercise. Cold Spring Harb Perspect Med. 2018;8:a029827.
Safdar A, Saleem A, Tarnopolsky MA. The potential of endurance exercise-derived exosomes to treat metabolic diseases. Nat Rev Endocrinol. 2016;12:504–17.
van Niel G, D’Angelo G, Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat Rev Mol Cell Biol. 2018;19:213–28.
Demonbreun AR, McNally EM. Muscle cell communication in development and repair. Curr Opin Pharmacol. 2017;34:7–14.
Whitham M, Parker BL, Friedrichsen M, Hingst JR, Hjorth M, Hughes WE, et al. Extracellular vesicles provide a means for tissue crosstalk during exercise. Cell Metab. 2018;27:237–51.
Eichner NZM, Erdbrügger U, Malin SK. Extracellular vesicles: a novel target for exercise-mediated reductions in type 2 diabetes and cardiovascular disease risk. J Diabetes Res. 2018;2018:7807245.
Wilhelm EN, González-Alonso J, Parris C, Rakobowchuk M. Exercise intensity modulates the appearance of circulating microvesicles with proangiogenic potential upon endothelial cells. Am J Physiol Heart Circ Physiol. 2016;311:H1297–310.
Wilhelm EN, Mourot L, Rakobowchuk M. Exercise-derived microvesicles: a review of the literature. Sports Med. 2018;48:2025–39.
Pergoli L, Cantone L, Favero C, Angelici L, Iodice S, Pinatel E, et al. Extracellular vesicle-packaged miRNA release after short-term exposure to particulate matter is associated with increased coagulation. Part Fibre Toxicol. 2017;14:32.
Davidson SM, Takov K, Yellon DM. Exosomes and cardiovascular protection. Cardiovasc Drugs Ther. 2017;31:77–86.
Csongrádi É, Nagy B Jr, Fulop T, Varga Z, Karányi Z, Magyar MT, et al. Increased levels of platelet activation markers are positively associated with carotid wall thickness and other atherosclerotic risk factors in obese patients. Thromb Haemost. 2011;106:683–92.
Borg GA. Perceived exertion: a note on “history” and methods. Med Sci Sports. 1973;5:90–3.
Xu R, Greening DW, Zhu HJ, Takahashi N, Simpson RJ. Extracellular vesicle isolation and characterization: toward clinical application. J Clin Investig. 2016;126:1152–62.
Milioli M, Ibáñez-Vea M, Sidoli S, Palmisano G, Careri M, Larsen MR. Quantitative proteomics analysis of platelet-derived microparticles reveals distinct protein signatures when stimulated by different physiological agonists. J Proteomics. 2015;121:56–66.
Durrer C, Robinson E, Wan Z, Martinez N, Hummel ML, Jenkins NT, et al. Differential impact of acute high-intensity exercise on circulating endothelial microparticles and insulin resistance between overweight/obese males and females. PLoS ONE. 2015;10:e0115860.
Lansford KA, Shill DD, Dicks AB, Marshburn MP, Southern WM, Jenkins NT. Effect of acute exercise on circulating angiogenic cell and microparticle populations. Exp Physiol. 2016;101:155–67.
Toth B, Nikolajek K, Rank A, Nieuwland R, Lohse P, Pihusch V, et al. Gender-specific and menstrual cycle dependent differences in circulating microparticles. Platelets. 2007;18:515–21.
Pardo F, Villalobos-Labra R, Sobrevia B, Toledo F, Sobrevia L. Extracellular vesicles in obesity and diabetes mellitus. Mol Aspects Med. 2018;60:81–91.
Tarakci H, Berger J. The sarcoglycan complex in skeletal muscle. Front Biosci. 2016;21:744–56.
Liu LA, Engvall E. Sarcoglycan isoforms in skeletal muscle. J Biol Chem. 1999;274:38171–6.
Guescini M, Canonico B, Lucertini F, Maggio S, Annibalini G, Barbieri E, et al. Muscle releases alpha-sarcoglycan positive extracellular vesicles carrying miRNAs in the bloodstream. PLoS ONE. 2015;10:e0125094.
Guiraud T, Gayda M, Juneau M, Bosquet L, Meyer P, Théberge-Julien G, et al. A single bout of high-intensity interval exercise does not increase endothelial or platelet microparticles in stable, physically fit men with coronary heart disease. Can J Cardiol. 2013;29:1285–91.
Chanda M, Nantakomol D, Suksom D, Palasuwan A. Cell-derived microparticles after exercise in individuals with G6PD Viangchan. Clin Hemorheol Microcirc. 2015;60:241–51.
Tao SC, Guo SC, Zhang CQ. Platelet-derived extracellular vesicles: an emerging therapeutic approach. Int J Biol Sci. 2017;13:828–34.
Wang ZT, Wang Z, Hu YW. Possible roles of platelet-derived microparticles in atherosclerosis. Atherosclerosis. 2016;248:10–6.
Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. 2018;5:135.
Ribeiro J, Almeida-Dias A, Ascensão A, Magalhães J, Oliveira AR, Carlson J, et al. Hemostatic response to acute physical exercise in healthy adolescents. J Sci Med Sport. 2007;10:164–9.
Maruyama K, Kadono T, Morishita E. Plasma levels of platelet-derived microparticles are increased after anaerobic exercise in healthy subjects. J Atheroscler Thromb. 2012;19:585–7.
Rigamonti AE, Resnik M, Compri E, Agosti F, De Col A, Monteleone P, et al. The cholestyramine-induced decrease of PYY postprandial response is negatively correlated with fat mass in obese women. Horm Metab Res. 2011;43:569–73.
Acknowledgements
The authors acknowledge the head-nurse Angela Seddone and the nursing staff at the Division of Auxology, Istituto Auxologico Italiano, Piancavallo, VB, Italy. Our special thanks go to the subjects and their families for their willingness to participate in this research. The authors thank Dr S. Zajac for the careful English revision.
Funding
The study was supported by Progetti di Ricerca Corrente, Istituto Auxologico Italiano, IRCCS, Milan, Italy.
Author information
Authors and Affiliations
Contributions
AER, together with VB and AS, designed the study. ADC, ST, and SC enrolled the subjects and performed the tests. RDM and GT performed the evaluation of body composition of all patients. ADC performed the biochemical determinations, while LP isolated and characterized plasma EVs. ST, ADC, and SC elaborated the database. SI and AER analyzed the data. AER, together with AS, wrote the manuscript. VB and SGC contributed to data interpretation and discussion writing. All authors contributed to the manuscript revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The patients and their parents (for the subjects younger than 18 years) and the healthy controls were fully informed of the procedures and possible risks associated with the experiments before giving their written consent to participate to the study. The protocol was approved by the local ethics committee (reference code: 01C825-2018; acronym: VESCIOBES). All procedures were in accordance with the Declaration of Helsinki (2000) of the World Medical Association.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rigamonti, A.E., Bollati, V., Pergoli, L. et al. Effects of an acute bout of exercise on circulating extracellular vesicles: tissue-, sex-, and BMI-related differences. Int J Obes 44, 1108–1118 (2020). https://doi.org/10.1038/s41366-019-0460-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0460-7
This article is cited by
-
Exploiting the therapeutic potential of contracting skeletal muscle-released extracellular vesicles in cancer: Current insights and future directions
Journal of Molecular Medicine (2024)
-
Extracellular vesicle distribution and localization in skeletal muscle at rest and following disuse atrophy
Skeletal Muscle (2023)
-
Sex differences in the transcriptome of extracellular vesicles secreted by fetal neural stem cells and effects of chronic alcohol exposure
Biology of Sex Differences (2023)
-
Transplantation of Exercise-Induced Extracellular Vesicles as a Promising Therapeutic Approach in Ischemic Stroke
Translational Stroke Research (2023)
-
Effects of Exercise on Extracellular Vesicles in Patients with Metabolic Dysfunction: a Systematic Review
Journal of Cardiovascular Translational Research (2023)