Abstract
Objectives
The aims of the present study were: (i) to analyze the associations of the time spent in daily activities (i.e., lie, recline, passive sit, active sit, stand, walk at slow pace, walk at average pace, walk at brisk pace, and other activities) with body mass index (BMI) and waist circumference (WC); and (ii) to examine how theoretically reallocating time between these daily activities is associated with BMI and WC.
Methods
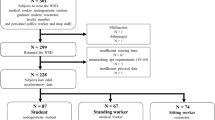
The sample included 437 older adults (288 women), aged 65 to 92 years, participating in the IMPACT65+ study. The time in daily activities was assessed by the Intelligent Device for Energy Expenditure and Activity (IDEEA). BMI and WC were measured following standardized procedures. Associations of daily activities with BMI and WC were examined using linear regression models adjusting for potential confounders. Isotemporal substitution models were performed to estimate the theoretical effect of replacing one activity with another activity while holding total time constant.
Results
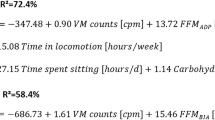
The time spent lying and reclining was associated with increased BMI and WC, while the time spent standing, walking at average pace, and walking at brisk pace was associated with decreased BMI and WC. Isotemporal substitution analyses revealed significant hypothetical reductions in BMI and WC when reallocating 15 min from lying or reclining to standing or walking at average pace. Moreover, replacing 15 min from any sedentary activity or light physical activity (except for walking at average pace) with an equal amount of time in walking at brisk pace was associated with lower BMI and WC.
Conclusions
This is the first study examining the activity specific and isotemporal associations of daily behaviors (considering body postures and movements) with overall and abdominal obesity in older people. The results could be used in the development of specific recommendations encouraging an active lifestyle in older people.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Peralta M, Ramos M, Lipert A, Martins J, Marques A. Prevalence and trends of overweight and obesity in older adults from 10 European countries from 2005 to 2013. Scand J Public Health. 2018;46:522–9.
García-Esquinas E, José García-García F, León-Muñoz LM, Carnicero JA, Guallar-Castillón P, Gonzalez-Colaço Harmand M, et al. Obesity, fat distribution, and risk of frailty in two population-based cohorts of older adults in Spain. Obesity. 2015;23:847–55.
Orces CH, Montalvan M, Tettamanti D. Prevalence of abdominal obesity and its association with cardio metabolic risk factors among older adults in Ecuador. Diabetes Metab Syndr. 2017;11:S727–33.
Gretebeck KA, Sabatini LM, Black DR, Gretebeck RJ. Physical activity, functional ability, and obesity in older adults: a gender difference. J Gerontol Nurs. 2017;43:38–46.
Cohen A, Ardern CI, Baker J. Inter-relationships between physical activity, body mass index, sedentary time, and cognitive functioning in younger and older adults: cross-sectional analysis of the Canadian Community Health Survey. Public Health. 2017;151:98–105.
Batsis JA, Germain CM, Vásquez E, Lopez-Jimenez F, Bartels SJ. Waist circumference, physical activity, and functional impairments in older U.S. dults: results from the NHANES 2005-2010. J Aging Phys Act. 2015;23:369–76.
Colley RC, Michaud I, Garriguet D. Reallocating time between sleep, sedentary and active behaviours: associations with obesity and health in Canadian adults. Health Rep. 2018;29:3–13.
Amireault S, Baier JM, Spencer JR. Physical activity preferences among older adults: a systematic review. J Aging Phys Act. 2017;27:1–38.
De Rezende LFM, Rey-López JP, Matsudo VKR, Luiz ODC. Sedentary behavior and health outcomes among older adults: a systematic review. BMC Public Health. 2014;14:333 https://doi.org/10.1186/1471-2458-14-333.
Gennuso KP, Gangnon RE, Matthews CE, Thraen-Borowski KM, Colbert LH. Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc. 2013;45:1493–500.
Rosique-Esteban N, Babio N, Díaz-López A, Romaguera D, Alfredo Martínez J, Sanchez VM, et al. Leisure-time physical activity at moderate and high intensity is associated with parameters of body composition, muscle strength and sarcopenia in aged adults with obesity and metabolic syndrome from the PREDIMED-Plus study. Clin Nutr. 2018;2018:1–8.
Jefferis BJ, Parsons TJ, Sartini C, Ash S, Lennon LT, Wannamethee SG, et al. Does duration of physical activity bouts matter for adiposity and metabolic syndrome? A cross-sectional study of older British men. Int J Behav Nutr Phys Act. 2016;13:36.
Füzéki E, Engeroff T, Banzer W. Health benefits of light-intensity physical activity: a systematic review of accelerometer data of the National Health and Nutrition Examination Survey (NHANES). Sports Med. 2017;47:1769–93.
Loprinzi PD, Lee H, Cardinal BJ. Evidence to support including lifestyle light-intensity recommendations in physical activity guidelines for older adults. Am J Health Promot. 2015;29:277–84.
Aggio DA, Sartini C, Papacosta O, Lennon LT, Ash S, Whincup PH, et al. Cross-sectional associations of objectively measured physical activity and sedentary time with sarcopenia and sarcopenic obesity in older men. Prev Med. 2016;91:264–72.
Buman MP, Hekler EB, Haskell WL, Pruitt L, Conway TL, Cain KL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172:1155–65.
Healy GN, Winkler EAH, Owen N, Anuradha S, Dunstan DW. Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur Heart J. 2015;36:2643–9.
Aguilar-Farías N, Brown WJ. Peeters GMEEG. ActiGraph GT3X+ cut-points for identifying sedentary behaviour in older adults in free-living environments. J Sci Med Sport. 2014;17:293–9.
Dumuid D, Lewis LK, Olds TS, Maher C, Bondarenko C, Norton L. Relationships between older adults’ use of time and cardio-respiratory fitness, obesity and cardio-metabolic risk: a compositional isotemporal substitution analysis. Maturitas. 2018;110:104–10.
Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009;170:519–27.
Mekary RA, Ding EL. Isotemporal substitution as the gold standard model for physical activity epidemiology: why it is the most appropriate for activity time research. Int J Environ Res Public Health. 2019;16:797.
Cabanas-Sánchez V, Higueras-Fresnillo S, de la Cámara MA, Esteban-Cornejo I, Martinez-Gomez D. 24-hour movement and non-movement behaviors in older adults. The IMPACT65 + study. Med Sci Sports Exerc. 2019;51:671–80.
Zhang K, Werner P, Sun M. Pi‐Sunyer FX, Boozer CNCN, Pi-Sunyer FX. Measurement of human daily physical activity. Obes Res. 2003;11:33–40.
Marsh AP, Vance RM, Frederick TL, Hesselmann SA, Rejeski WJ. Objective assessment of activity in older adults at risk for mobility disability. Med Sci Sports Exerc. 2007;39:1020–26.
Cabanas-Sanchez V, Higueras-Fresnillo S, De La Camara M, Veiga OL, Martinez-Gomez D. Automated algorithms for detecting sleep period time using a multi-sensor pattern-recognition activity monitor from 24-h free-living data in older adults. Physiol Meas. 2018;39:055002.
Gutiérrez-Fisac JL, López E, Banegas JR, Graciani A, Rodríguez-Artalejo F. Prevalence of overweight and obesity in elderly people in Spain. Obes Res. 2004;12:710–15.
Grundy SM, Brewer HB, Cleeman JI, Smith SC, Lenfant C. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on Scientific Issues Related to Definition. Circulation. 2004;109:433–8.
Ware JJ, Sherbourne C. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B. 1995;57:289–300.
Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31:369–71.
Swartz AM, Tarima S, Miller NE, Hart TL, Grimm EK, Rote AE, et al. Prediction of body fat in older adults by time spent in sedentary behavior. J Aging Phys Act. 2012;20:332–44.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, et al. 2011 compendium of physical activities: asecond update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81.
Júdice PB, Silva AM, Sardinha LB. Sedentary bout durations are associated with abdominal obesity in older adults. J Nutr Health Aging. 2015;19:798–804.
Stamatakis E, Rogers K, Ding D, Berrigan D, Chau J, Hamer M, et al. All-cause mortality effects of replacing sedentary time with physical activity and sleeping using an isotemporal substitution model: a prospective study of 201,129 mid-aged and older adults. Int J Behav Nutr Phys Act. 2015;12:121.
Kuhle CL, Steffen MW, Anderson PJ, Murad MH. Effect of exercise on anthropometric measures and serum lipids in older individuals: a systematic review and meta-analysis. BMJ Open. 2014;4:e005283.
Hamer M, Stamatakis E, Steptoe A. Effects of substituting sedentary time with physical activity on metabolic risk. Med Sci Sports Exerc. 2014;46:1946–50.
Boyle T, Vallance JK, Buman MP, Lynch BM. Reallocating time to sleep, sedentary time, or physical activity: associations with waist circumference and body mass index in breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2017;26:254–60.
Falconer CL, Page AS, Andrews RC, Cooper AR. The potential impact of displacing sedentary time in adults with type 2 diabetes. Med Sci Sports Exerc. 2015;47:2070–5.
Dahl-Petersen IK, Brage S, Bjerregaard P, Tolstrup JS, Jørgensen ME. Physical activity and abdominal fat distribution in Greenland. Med Sci Sports Exerc. 2017;49:2064–70.
Ekblom-Bak E, Ekblom Ö, Bergström G, Börjesson M. Isotemporal substitution of sedentary time by physical activity of different intensities and bout lengths, and its associations with metabolic risk. Eur J Prev Cardiol. 2016;23:967–74.
Nilsson A, Wåhlin-Larsson B, Kadi F. Physical activity and not sedentary time per se influences on clustered metabolic risk in elderly community-dwelling women. PLoS ONE. 2017;12:e0175496.
Waters DL, Ward AL, Villareal DT. Weight loss in obese adults 65 years and older: a review of the controversy. Exp Gerontol. 2013;48:1054–61.
Batsis JA, Gill LE, Masutani RK, Adachi-Mejia AM, Blunt HB, Bagley PJ, et al. Weight loss interventions in older adults with obesity: a systematic review of randomized controlled trials since 2005. J Am Geriatr Soc. 2017;65:257–68.
de la Cámara MÁ, Higueras-Fresnillo S, Martinez-Gomez D, Veiga OL. Inter-day reliability of the IDEEA activity monitor for measuring movement and non-movement behaviors in older adults. J Aging Phys Act. 2018;29:1–33.
Acknowledgements
This work was supported by Grants from MINECO I + D + i (DEP2013–47786-R), UAM-Santander (CEAL-AL/2015–20), and Real Madrid-UEM (P2016/RM09). SHF and MAC were supported by FPI grants from the Autonomous University of Madrid. The funding organizations had no role in the study design, the collection, analysis or interpretation of the data or the decision to submit the paper for publication.
Authors contributions
Designed research (project conception, development of overall research plan, and study oversight): DMG. Conducted research (hands-on conduct of the experiments and data collection): VCS, MAC, KPS, SHF, and DMG. Analyzed data or performed statistical analysis: VCS, DMG. Wrote paper (only authors who made a major contribution): VCS. Revised and approved the final version of the paper: VCS, MAC, KPS, SHF, and DMG. Had primary responsibility for final content: VCS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Cabanas-Sánchez, V., De la Cámara, M.A., Sadarangani, K.P. et al. Associations of daily activities measured by a pattern-recognition activity monitor with overall and abdominal obesity in older people: the IMPACT65+ study. Int J Obes 43, 2545–2554 (2019). https://doi.org/10.1038/s41366-019-0439-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0439-4