Abstract
Background
Different directions of the association of birthweight with cardio-metabolic health have been found, especially in children, which may be explained by the mediating effect of attained adiposity. We aimed to untangle direct and BMI-mediated associations of birthweight with childhood cardio-metabolic indicators.
Methods
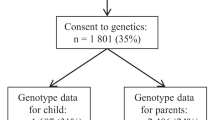
Children from Generation XXI birth cohort were included (n = 4881). Birthweight was abstracted from clinical files. At age 4 and 7, children were re-evaluated. Glucose, triglycerides, LDL-cholesterol, systolic (SBP) and diastolic blood pressure (DBP) z-scores were the cardio-metabolic traits analyzed. Regression coefficients and respective 95% confidence intervals [β (95%CI)] were computed using path analysis.
Results
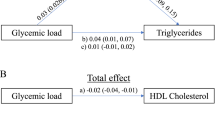
Birthweight had inverse total effect on SBP at age 4 [−0.005 (−0.010; −0.001)] and 7 [−0.011 (−0.017; −0.006)] and DBP at 7 [−0.008 (−0.012; −0.004)]. Direct effects were found for SBP at 4 [−0.013 (−0.018; −0.009)] and 7 [−0.014 (−0.019; −0.009)], and DBP at 7 [−0.010 (−0.015; −0.006)], explaining the inverse total effects. Positive BMI-mediated indirect effects were found for all cardio-metabolic traits: higher birthweight was associated with higher childhood BMI, which in turn was associated with higher levels of cardio-metabolic traits.
Conclusions
Positive BMI-mediated effect of birthweight on all cardio-metabolic traits was found. However, direct effects were in the opposite direction, significant for blood pressure, which may explain the diversity of results observed in the literature. Combining the direct and BMI-mediated effects, higher birthweight was associated with lower blood pressure at age 7 and have no effect on other cardio-metabolic traits.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5.
Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350(23):2362–74.
Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia. 1993;36(1):62–7.
Barker DJ, Eriksson JG, Forsen T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol. 2002;31(6):1235–9.
Hales CN, Barker DJ. The thrifty phenotype hypothesis. Br Med Bull. 2001;60:5–20.
Lakshmy R. Metabolic syndrome: role of maternal undernutrition and fetal programming. Rev Endocr Metab Disord. 2013;14(3):229–40.
Wells JC. The programming effects of early growth. Early Hum Dev. 2007;83(12):743–8.
Beilin L, Huang RC. Childhood obesity, hypertension, the metabolic syndrome and adult cardiovascular disease. Clin Exp Pharmacol Physiol. 2008;35(4):409–11.
Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115(3):e290–6.
Lucas A. Programming by early nutrition in man. Ciba Found Symp. 1991;156:38–50. discussion-5.
Young JB. Programming of sympathoadrenal function. Trends Endocrinol Metab. 2002;13(9):381–5.
Twisk JW, Kemper HC, Mellenbergh GJ. Mathematical and analytical aspects of tracking. Epidemiol Rev. 1994;16(2):165–83.
Larsen PS, Kamper-Jorgensen M, Adamson A, Barros H, Bonde JP, Brescianini S, et al. Pregnancy and birth cohort resources in europe: a large opportunity for aetiological child health research. Paediatr Perinat Epidemiol. 2013;27(4):393–414.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry. 1972;18(6):499–502.
National High Blood Pressure Education Program Working Group on High Blood Pressure in C, Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–76.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. Geneva: World Health Organization; 2006.
Stine RA. Graphical interpretation of variance inflation factors. Am Stat. 1995;49:53–6.
Rosseel Y. lavaan: an R package for structural equation modeling. J Stats Softw. 2012;48:1–36.
Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238–46.
Tucker L, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10.
Steiger JH. Structural model evaluation and modification. an interval estimation approach. Multivar Behav Res. 1990;25:173–80.
Hu L, Bentler P. Cutoff criteria for fit indices in covariance structure analysis. Conventional criteria versus new alternatives. Struct Equ Model. 1999;6:1–55.
Browne MW, Cudeck C. Alternative ways of assessing model fit. Sociol Method Res. 1993;21:230–58.
Friend A, Craig L, Turner S. The prevalence of metabolic syndrome in children: a systematic review of the literature. Metab Syndr Relat Disord. 2013;11(2):71–80.
Eriksson JG, Forsen T, Tuomilehto J, Osmond C, Barker DJ. Early growth and coronary heart disease in later life: longitudinal study. BMJ. 2001;322(7292):949–53.
Parsons TJ, Power C, Manor O. Fetal and early life growth and body mass index from birth to early adulthood in 1958 British cohort: longitudinal study. BMJ. 2001;323(7325):1331–5.
Wells JC, Chomtho S, Fewtrell MS. Programming of body composition by early growth and nutrition. Proc Nutr Soc. 2007;66(3):423–34.
Druet C, Ong KK. Early childhood predictors of adult body composition. Best Pract Res Clin Endocrinol Metab. 2008;22(3):489–502.
Sacco MR, de Castro NP, Euclydes VL, Souza JM, Rondo PH. Birth weight, rapid weight gain in infancy and markers of overweight and obesity in childhood. Eur J Clin Nutr. 2013;67(11):1147–53.
Jaiswal M, Crume T, Vehik K, Scherzinger A, Stamm E, Hamman RF, et al. Is low birth weight associated with adiposity in contemporary U.S. youth? The Exploring Perinatal Outcomes among Children (EPOCH) Study. J Dev Orig Health Dis. 2012;3(3):166–72.
Rogers IS, Ness AR, Steer CD, Wells JC, Emmett PM, Reilly JR, et al. Associations of size at birth and dual-energy X-ray absorptiometry measures of lean and fat mass at 9 to 10 y of age. Am J Clin Nutr. 2006;84(4):739–47.
Willig AL, Hanks LJ, Fernandez JR. Birth weight is associated with body composition in a multiethnic pediatric cohort. Open Obes J. 2011;3:4–8.
Huxley RR, Shiell AW, Law CM. The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: a systematic review of the literature. J Hypertens. 2000;18(7):815–31.
Zhang Y, Li H, Liu SJ, Fu GJ, Zhao Y, Xie YJ, et al. The associations of high birth weight with blood pressure and hypertension in later life: a systematic review and meta-analysis. Hypertens Res. 2013;36(8):725–35.
Jaquet D, Leger J, Levy-Marchal C, Czernichow P. Low birth weight: effect on insulin sensitivity and lipid metabolism. Horm Res. 2003;59(1):1–6.
Kajantie E, Barker DJ, Osmond C, Forsen T, Eriksson JG. Growth before 2 years of age and serum lipids 60 years later: the Helsinki Birth Cohort study. Int J Epidemiol. 2008;37(2):280–9.
Newsome CA, Shiell AW, Fall CH, Phillips DI, Shier R, Law CM. Is birth weight related to later glucose and insulin metabolism?–A systematic review. Diabet Med. 2003;20(5):339–48.
Law CM, Gordon GS, Shiell AW, Barker DJ, Hales CN. Thinness at birth and glucose tolerance in seven-year-old children. Diabet Med. 1995;12(1):24–9.
Hofman PL, Cutfield WS, Robinson EM, Bergman RN, Menon RK, Sperling MA, et al. Insulin resistance in short children with intrauterine growth retardation. J Clin Endocrinol Metab. 1997;82(2):402–6.
Whincup PH, Cook DG, Adshead F, Taylor SJ, Walker M, Papacosta O, et al. Childhood size is more strongly related than size at birth to glucose and insulin levels in 10-11-year-old children. Diabetologia. 1997;40(3):319–26.
Bavdekar A, Yajnik CS, Fall CH, Bapat S, Pandit AN, Deshpande V, et al. Insulin resistance syndrome in 8-year-old Indian children: small at birth, big at 8 years, or both? Diabetes. 1999;48(12):2422–9.
Lawlor DA. The Society for Social Medicine John Pemberton Lecture 2011. Developmental overnutrition-an old hypothesis with new importance? Int J Epidemiol. 2013;42(1):7–29.
Howe LD, Tilling K, Galobardes B, Lawlor DA. Loss to follow-up in cohort studies: bias in estimates of socioeconomic inequalities. Epidemiology. 2013;24(1):1–9.
Expert Panel on Integrated Guidelines for Cardiovascular, Health Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213–56.
Gamborg M, Andersen PK, Baker JL, Budtz-Jorgensen E, Jorgensen T, Jensen G, et al. Life course path analysis of birth weight, childhood growth, and adult systolic blood pressure. Am J Epidemiol. 2009;169(10):1167–78.
Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42(5):1511–9.
Acknowledgements
The authors gratefully acknowledge the families enrolled in Generation XXI for their kindness, all members of the research team for their enthusiasm and perseverance and the participating hospitals and their staff for their help and support. They also acknowledge the project DOCnet (NORTE-01-0145-FEDER-000003), supported by Norte Portugal Regional Operational Programme (NORTE 2020), under the PORTUGAL 2020 Partnership Agreement, through the European Regional Development Fund (ERDF).
Funding
This work was supported by Programa Operacional de Saúde – Saúde XXI, Quadro Comunitário de Apoio III and Administração Regional de Saúde Norte (Regional Department of Ministry of Health); FEDER through the Operational Programme Competitiveness and Internationalization and national funding from the Foundation for Science and Technology – FCT (Portuguese Ministry of Science, Technology and Higher Education) [POCI-01- 0145-FEDER-016837], under the project “PathMOB.: Risco cardiometabólico na infância: desde o início da vida ao fim da infância” [Ref. FCT PTDC/DTP-EPI/3306/2014], and FCT Investigator contract [IF/01060/2015] to ACS; Unidade de Investigação em Epidemiologia - Instituto de Saúde Pública da Universidade do Porto (EPIUnit) [POCI-01-0145-FEDER-006862; Ref. UID/DTP/04750/2013]; European Commission [project reference FP7-ENV-2013-603946]; and UK Medical Research Council [MC_UU_12013/5] and UK National Institute of Health Research Senior Investigator [NF-SI-0611-10196] to DAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Fonseca, M.J., Severo, M., Lawlor, D.A. et al. Direct and BMI-mediated effect of birthweight on childhood cardio-metabolic health—a birth cohort study. Int J Obes 43, 1923–1931 (2019). https://doi.org/10.1038/s41366-019-0413-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0413-1
This article is cited by
-
The impact of macrosomia on cardiometabolic health in preteens: findings from the ROLO longitudinal birth cohort study
Nutrition & Metabolism (2023)