Abstract
Background
In recent decades, the prevalence of gastroesophageal reflux disease (GERD) and obesity has been increasing while Helicobacter pylori infection has been decreasing.
Objective
To evaluate if H. pylori treatment, excess body weight and other anthropometric measurements are associated with incident erosive esophagitis, as a secondary objective of a trial which tested the efficacy of treatment of H. pylori on the symptoms of functional dyspepsia.
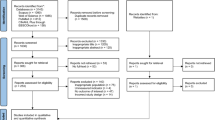
Subjects/methods
Upper gastrointestinal endoscopy and anthropometric assessments were performed, at baseline and after 12 months, in H. pylori positive patients with functional dyspepsia who had no baseline reflux symptoms or esophagitis. Patients were randomly assigned to receive omeprazole, amoxicillin, and clarithromycin (antibiotic group; n = 201) or omeprazole plus placebo (control group; n = 203). The primary outcome was the incidence of esophagitis 12 months after randomization, according to treatment groups, and the association of BMI and other anthropometric measurements.
Results
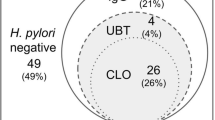
Four hundred and four patients were included (mean age, 46.1 years; 78.7% women). The 12-month follow-up endoscopic esophagitis rates for the antibiotic and control groups were 10.9% (22/201) and 9.4% (19/203), respectively (p = 0.60). The number needed to harm was 67. Baseline anthropometric measurements were performed in 94% (380/404) of patients. The 12-month follow-up esophagitis rates for overweight and normal body weight patients were 13.6% (29/213) and 6.0% (10/167), respectively (p = 0.015); rates for patients with and without increased baseline waist circumference were 15.4% (24/156) and 6.7% (15/224), respectively (p = 0.006). Following logistic regression, only the combination of increased baseline body mass index and waist, but not H. pylori treatment, was independently associated with new-onset esophagitis (OR 2.88; 95% CI: 1.28–6.45).
Conclusions
Excess body weight and concomitant increased waist circumference, but not H. pylori treatment, predicts new-onset esophagitis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author on request.
References
El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63:871–80.
Yaghoobi M, Farrokhyar F, Yuan Y, Hunt RH. Is there an increased risk of GERD after Helicobacter pylori eradication?: a meta-analysis. Am J Gastroenterol. 2010;105:1007–13. quiz 1006, 1014
Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28.
Nordenstedt H, Nilsson M, Johnsen R, Lagergren J, Hveem K. Helicobacter pylori infection and gastroesophageal reflux in a population-based study (The HUNT Study). Helicobacter. 2007;12:16–22.
Chang P, Friedenberg F. Obesity and GERD. Gastroenterol Clin North Am. 2014;43:161–73.
Talley NJ, Howell S, Poulton R. Obesity and chronic gastrointestinal tract symptoms in young adults: a birth cohort study. Am J Gastroenterol. 2004;99:1807–14.
Breckan RK, Paulssen EJ, Asfeldt AM, Mortensen L, Straume B, Florholmen J. The impact of body mass index and Helicobacter pylori infection on gastro-oesophageal reflux symptoms: a population-based study in Northern Norway. Scand J Gastroenterol. 2009;44:1060–6.
Gunji T, Sato H, Iijima K, et al. Risk factors for erosive esophagitis: a cross-sectional study of a large number of Japanese males. J Gastroenterol. 2011;46:448–55.
Chiba H, Gunji T, Sato H, et al. A cross-sectional study on the risk factors for erosive esophagitis in young adults. Intern Med. 2012;51:1293–9. http://www.ncbi.nlm.nih.gov/pubmed/22687832.
Minatsuki C, Yamamichi N, Shimamoto T, et al. Background factors of reflux esophagitis and non-erosive reflux disease: a cross-sectional study of 10,837 subjects in Japan. PLoS One. 2013;8:e69891.
Labenz J, Blum AL, Bayerdörffer E, Meining A, Stolte M, Börsch G. Curing Helicobacter pylori infection in patients with duodenal ulcer may provoke reflux esophagitis. Gastroenterology. 1997;112:1442–7. http://www.ncbi.nlm.nih.gov/pubmed/9136820
Hamada H, Haruma K, Mihara M, et al. High incidence of reflux oesophagitis after eradication therapy for Helicobacter pylori: impacts of hiatal hernia and corpus gastritis. Aliment Pharmacol Ther. 2000;14:729–35. http://www.ncbi.nlm.nih.gov/pubmed/10848656
Ott EA, Mazzoleni LE, Edelweiss MI, et al. Helicobacter pylori eradication does not cause reflux oesophagitis in functional dyspeptic patients: a randomized, investigator-blinded, placebo-controlled trial. Aliment Pharmacol Ther. 2005;21:1231–9.
Kim N, Lee SW, Kim JIl, et al. Effect of Helicobacter pylori eradication on the development of reflux Esophagitis and gastroesophageal reflux symptoms: a Nationwide Multi-Center Prospective Study. Gut Liver. 2011;5:437–46.
Malfertheiner P, Dent J, Zeijlon L, et al. Impact of Helicobacter pylori eradication on heartburn in patients with gastric or duodenal ulcer disease—results from a randomized trial programme. Aliment Pharmacol Ther. 2002;16:1431–42. http://www.ncbi.nlm.nih.gov/pubmed/12182742
Singh S, Sharma AN, Murad MH, et al. Central adiposity is associated with increased risk of esophageal inflammation, metaplasia, and adenocarcinoma: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2013;11:1399–1412.e7.
Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143:199–211. http://www.ncbi.nlm.nih.gov/pubmed/16061918.
Nam SY, Choi IJ, Ryu KH, Park BJ, Kim HB, Nam B-H. Abdominal visceral adipose tissue volume is associated with increased risk of erosive esophagitis in men and women. Gastroenterology. 2010;139:1902–11.e2.
El-Serag HB, Graham DY, Satia JA, Rabeneck L. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol. 2005;100:1243–50.
Chung SJ, Kim D, Park MJ, et al. Metabolic syndrome and visceral obesity as risk factors for reflux oesophagitis: a cross-sectional case-control study of 7078 Koreans undergoing health check-ups. Gut. 2008;57:1360–5.
Kubo A, Cook MB, Shaheen NJ, et al. Sex-specific associations between body mass index, waist circumference and the risk of Barrett’s oesophagus: a pooled analysis from the international BEACON consortium. Gut. 2013;62:1684–91.
Chen T, Lu M, Wang X, et al. Prevalence and risk factors of gastroesophageal reflux symptoms in a Chinese retiree cohort. BMC Gastroenterol. 2012;12:161.
Zagari RM, Fuccio L, Wallander M-A, et al. Gastro-oesophageal reflux symptoms, oesophagitis and Barrett’s oesophagus in the general population: the Loiano-Monghidoro study. Gut. 2008;57:1354–9.
Lagergren J, Bergström R, Nyrén O. No relation between body mass and gastro-oesophageal reflux symptoms in a Swedish population based study. Gut. 2000;47:26–29. http://www.ncbi.nlm.nih.gov/pubmed/10861260.
Zalar A, Haddouche B, Antonietti M, et al. Lack of correlation between morbid obesity and severe gastroesophageal reflux disease in candidates for bariatric surgery: results of a large prospective study. Obes Surg. 2013;23:1939–41.
Mazzoleni LE, Sander GB, Francesconi CF, de M, et al. Helicobacter pylori eradication in functional dyspepsia: HEROES trial. Arch Intern Med. 2011;171:1929–36.
Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–79.
Sami S, Ragunath K. The los angeles classification of gastroesophageal reflux disease. Video J Encycl GI Endosc. 2013;1:103–4. http://www.video-endoscopy.com/article/S2212097113700463/fulltext.
Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161–81. http://www.ncbi.nlm.nih.gov/pubmed/8827022.
Faulkner JA. Physiology of swimming. Res Q. 1966;37:41–54. http://www.ncbi.nlm.nih.gov/pubmed/5217133.
Pollock ML, Wilmore J. Exercise in health and disease: Evaluation and prescription for prevention and rehabilitation. 2nd ed. Philadelphia: W.B.Saunders Co. 1990.
World Health Organization. Obesity: preventing and managing the global epidemic: Report on a WHO Consultation. WHO Tech Rep Ser. 2000;894:252. http://www.who.int/iris/handle/10665/42330#sthash.bTJ38E0Q.dpuf.
Cremonini F, Di Caro S, Delgado-Aros S, et al. Meta-analysis: the relationship between Helicobacter pylori infection and gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2003;18:279–89. http://www.ncbi.nlm.nih.gov/pubmed/12895212.
Xie T, Cui X, Zheng H, Chen D, He L, Jiang B. Meta-analysis: eradication of Helicobacter pylori infection is associated with the development of endoscopic gastroesophageal reflux disease. Eur J Gastroenterol Hepatol. 2013;25:1195–205.
Qian B, Ma S, Shang L, Qian J, Zhang G. Effects of Helicobacter pylori eradication on gastroesophageal reflux disease. Helicobacter. 2011;16:255–65.
Raghunath AS, Hungin APS, Wooff D, Childs S. Systematic review: the effect of Helicobacter pylori and its eradication on gastro-oesophageal reflux disease in patients with duodenal ulcers or reflux oesophagitis. Aliment Pharmacol Ther. 2004;20:733–44.
Saad AM, Choudhary A, Bechtold ML. Effect of Helicobacter pylori treatment on gastroesophageal reflux disease (GERD): meta-analysis of randomized controlled trials. Scand J Gastroenterol. 2012;47:129–35.
Erőss B, Farkas N, Vincze Á, et al. Helicobacter pylori infection reduces the risk of Barrett’s esophagus: a meta-analysis and systematic review. Helicobacter. 2018;23:e12504.
Vakil N, Talley NJ, Stolte M, Sundin M, Junghard O, Bolling-Sternevald E. Patterns of gastritis and the effect of eradicating Helicobacter pylori on gastro-oesophageal reflux disease in Western patients with non-ulcer dyspepsia. Aliment Pharmacol Ther. 2006;24:55–63.
Fornari F, Callegari-Jacques SM, Dantas RO, Scarsi AL, Ruas LO, de Barros SGS. Obese patients have stronger peristalsis and increased acid exposure in the esophagus. Dig Dis Sci. 2011;56:1420–6.
Jacobson BC, Chan AT, Giovannucci EL, Fuchs CS. Body mass index and Barrett’s oesophagus in women. Gut. 2009;58:1460–6.
Kendall BJ, Rubenstein JH, Cook MB, et al. Inverse Association Between Gluteofemoral Obesity and Risk of Barrett’s Esophagus in a Pooled Analysis. Clin Gastroenterol Hepatol. 2016;14:1412–19.e3.
Emerenziani S, Rescio MP, Guarino MPL, Cicala M. Gastro-esophageal reflux disease and obesity, where is the link? World J Gastroenterol. 2013;19:6536–9.
Trasande L, Blustein J, Liu M, Corwin E, Cox LM, Blaser MJ. Infant antibiotic exposures and early-life body mass. Int J Obes. 2013. https://doi.org/10.1038/ijo.2012.132.
Mueller NT, Whyatt R, Hoepner L, et al. Prenatal exposure to antibiotics, cesarean section and risk of childhood obesity. Int J Obes. 2015;39:665–70.
Lane JA, Murray LJ, Harvey IM, Donovan JL, Nair P, Harvey RF. Randomised clinical trial: Helicobacter pylori eradication is associated with a significantly increased body mass index in a placebo-controlled study. Aliment Pharmacol Ther. 2011. https://doi.org/10.1111/j.1365-2036.2011.04610.x.
Kamada T, Hata J, Kusunoki H, et al. Eradication of Helicobacter pylori increases the incidence of hyperlipidaemia and obesity in peptic ulcer patients. Dig Liver Dis. 2005. https://doi.org/10.1016/j.dld.2004.07.017.
Kasai C, Sugimoto K, Moritani I, et al. Changes in plasma ghrelin and leptin levels in patients with peptic ulcer and gastritis following eradication of Helicobacter pylori infection. BMC Gastroenterol. 2016. https://doi.org/10.1186/s12876-016-0532-2.
Yanagi H, Tsuda A, Matsushima M, et al. Changes in the gut microbiota composition and the plasma ghrelin level in patients with Helicobacter pylori-infected patients with eradication therapy. BMJ Open Gastroenterol. 2017. https://doi.org/10.1136/bmjgast-2017-000182.
Moayyedi P, Soo S, Deeks J, et al. Eradication of Helicobacter pylori for non-ulcer dyspepsia. Cochrane database Syst Rev. 2006;2:CD002096.
Acknowledgements
We are grateful to our study participants. The investigators thank Aché Laboratórios Farmacêuticos for unrestricted donation of the study drugs and the gastroscope.
Funding
The study drugs and a gastroscope, used to perform the endoscopies during the study, were obtained through unrestricted donation from the Aché Laboratórios Farmacêuticos SA, São Paulo, Brazil.
Author information
Authors and Affiliations
Contributions
Conception and design: FM, LEM, GBS, CFMF, PSVR; acquisition, analysis or interpretation of data: all authors; drafting of the article: FM, RVCP, DS, CFMF, NJT, LEM, TCM; critical revision of the article: all authors; final approval of the article: all authors; provision of study materials or patients: FM, TCM, LRB, PSVR, LL, NFT; statistical expertise: FM, LEM, RVCP, DS, NJT, TCM; obtaining of funding: FM, LEM; administrative, technical, or logistic support: FM, LEM, TCM, LRB, PSVR, LL, NFT; collection and assembly of data: FM, LEM, GBS, CFMF, PSVR. All authors read and approved the final version of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mazzoleni, F., Mazzoleni, L.E., de Magalhães Francesconi, C.F. et al. Potential roles of Helicobacter pylori treatment, body mass index and waist circumference in the causation of erosive esophagitis: a randomized clinical trial (HEROES-GERD). Int J Obes 44, 147–158 (2020). https://doi.org/10.1038/s41366-019-0391-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0391-3
This article is cited by
-
Dietary Habits and Risk of Esophagitis and Barrett’s Esophagus: A Multicenter Italian Case–Control Study
Digestive Diseases and Sciences (2021)