Abstract
Background/objectives
The waist-to-height ratio (WHtR) estimates cardiometabolic risk in youth without need for growth charts by sex and age. Questions remain about whether waist circumference measured per protocol of the National Health and Nutrition Examination Survey (WNHAHtR) or World Health Organization (WWHOHtR) can better predict blood pressures and lipid parameters in youth.
Participants/methods
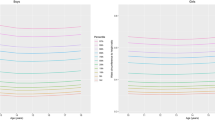
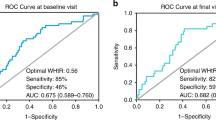
WHtR was measured under both anthropometric protocols among participants in the SEARCH Study, who were recently diagnosed with diabetes (ages 5–19 years; N = 2 773). Biomarkers were documented concurrently with baseline anthropometry and again ~7 years later (ages 10–30 years; N = 1 712). For prediction of continuous biomarker outcomes, baseline WNHAHtR or WWHOHtR entered semiparametric regression models employing restricted cubic splines. To predict binary biomarkers (high-risk group defined as the most adverse quartile) linear WNHAHtR or WWHOHtR terms entered logistic models. Model covariates included demographic characteristics, pertinent medication use, and (for prospective predictions) the follow-up time since baseline. We used measures of model fit, including the adjusted-R2 and the area under the receiver operator curves (AUC) to compare WNHAHtR and WWHOHtR.
Results
For the concurrent biomarkers, the proportion of variation in each outcome explained by full regression models ranged from 23 to 46%; for the prospective biomarkers, the proportions varied from 11 to 30%. Nonlinear relationships were recognized with the lipid outcomes, both at baseline and at follow-up. In full logistic models, the AUCs ranged from 0.75 (diastolic pressure) to 0.85 (systolic pressure) at baseline, and from 0.69 (triglycerides) to 0.78 (systolic pressure) at the prospective follow-up. To predict baseline elevations of the triglycerides/HDL cholesterol ratio, the AUC was 0.816 for WWHOHtR compared with 0.810 for WNHAHtR (p = 0.003), but otherwise comparisons between alternative WHtR protocols were not significantly different.
Conclusions
Among youth with recently diagnosed diabetes, measurements of WHtR by either waist circumference protocol similarly helped estimate current and prospective cardiometabolic risk biomarkers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes Rev. 2012;13:275–86.
Savva SC, Lamnisos D, Kafatos AG. Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes Metab Syndr Obes. 2013;6:403–19. https://doi.org/10.2147/DMSO.S34220.
Kahn HS, Cheng YJ. Comparison of adiposity indicators associated with fasting-state insulinemia, triglyceridemia, and related risk biomarkers in a nationally representative, adult population. Diabetes Res Clin Pract. 2018;136:7–15.
Kahn HS, Imperatore G, Cheng YJ. A population-based comparison of BMI percentiles and waist-to-height ratio for identifying cardiovascular risk in youth. J Pediatr. 2005;146:482–8.
Freedman DS, Kahn HS, Mei Z, Grummer-Strawn LM, Dietz WH, Srinivasan SR, et al. Relation of body mass index and waist-to-height ratio to cardiovascular disease risk factors in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr. 2007;86:33–40.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010;23:247–69.
Katzmarzyk PT, Shen W, Baxter-Jones A, Bell JD, Butte NF, Demerath EW, et al. Adiposity in children and adolescents: correlates and clinical consequences of fat stored in specific body depots. Pediatr Obes. 2012;7:e42–61.
Sharma AK, Metzger DL, Daymont C, Hadjiyannakis S, Rodd CJ. LMS tables for waist-circumference and waist-height ratio Z-scores in children aged 5-19 y in NHANES III: association with cardio-metabolic risks. Pediatr Res. 2015;78:723–9.
Seo JY, Kim JH. Validation of surrogate markers for metabolic syndrome and cardiometabolic risk factor clustering in children and adolescents: a nationwide population-based study. PLOS One. 2017;12:e0186050.
Giannini DT, Kuschnir MCC, de Oliveira CL, Szklo M. Waist-to-Height Ratio as a Predictor of C-Reactive Protein Levels. J Am Coll Nutr. 2017;36:624–30.
Oliveira RG, Guedes DP. Performance of anthropometric indicators as predictors of metabolic syndrome in Brazilian adolescents. BMC Pediatr. 2018;18:33 .
Lin MS, Lin TH, Guo SE, Tsai MH, Chiang MS, Huang TJ, et al. Waist-to-height ratio is a useful index for nonalcoholic fatty liver disease in children and adolescents: a secondary data analysis. BMC Public Health. 2017;17:851. .
Garnett SP, Baur LA, Cowell CT. Waist-to-height ratio: a simple option for determining excess central adiposity in young people. Int J Obes (Lond). 2008;32:1028–30.
Taylor RW, Williams SM, Grant AM, Taylor BJ, Goulding A. Predictive ability of waist-to-height in relation to adiposity in children is not improved with age and sex-specific values. Obesity. 2011;19:1062–8.
Lo K, Wong M, Khalechelvam P, Tam W. Waist-to-height ratio, body mass index and waist circumference for screening paediatric cardio-metabolic risk factors: a meta-analysis. Obes Rev. 2016;17:1258–75.
Bosy-Westphal A, Booke CA, Blocker T, Kossel E, Goele K, Later W, et al. Measurement site for waist circumference affects its accuracy as an index of visceral and abdominal subcutaneous fat in a caucasian population. J Nutr. 2010;140:954–61.
Pettitt DJ, Talton JW, Liese AD, Liu LL, Crimmins N, West NA, et al. Comparison of two waist circumference measurement protocols: the SEARCH for Diabetes in Youth Study. Pediatr Obes. 2012;7:e81–e85.
Ma WY, Yang CY, Shih SR, Hsieh HJ, Hung CS, Chiu FC, et al. Measurement of waist circumference: Midabdominal or iliac crest? Diabetes Care. 2013;36:1660–6.
Hamman RF, Bell RA, Dabelea D, D’Agostino RB Jr., Dolan L, Imperatore G, et al. The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care. 2014;37:3336–44.
Taylor RW, Williams SM, Carter PJ, Goulding A, Gerrard DF, Taylor BJ. Changes in fat mass and fat-free mass during the adiposity rebound: FLAME study. Int J Pediatr Obes. 2011;6:e243–251.
National Center for Health Statistics. Anthropometry Procedures Manual–National Health and Nutrition Examination Survey (NHANES). NCHS, Hyattsville, MD, 2013 http://www.cdc.gov/nchs/data/nhanes/nhanes_13_14/2013_Anthropometry.pdf. Accessed 26 June 2018.
World Health Organization. Waist circumference and waist–hip ratio: Report of a WHO expert consultation, Geneva, 8–11 December, 2008. WHO, Geneva, Switzerland, 2011. http://apps.who.int/iris/bitstream/10665/44583/1/9789241501491_eng.pdf. Accessed 26 June 2018.
Arsenault BJ, Despres JP, Stroes ES, Wareham NJ, Kastelein JJ, Khaw KT, et al. Lipid assessment, metabolic syndrome and coronary heart disease risk. Eur J Clin Invest. 2010;40:1081–93.
Emerging Risk Factors Collaboration, Di Angelantonio E, Gao P, Pennells L, Kaptoge S, Caslake M, et al. LIpid-related markers and cardiovascular disease prediction. JAMA. 2012;307:2499–506.
Quispe R, Martin SS, Jones SR. Triglycerides to high-density lipoprotein-cholesterol ratio, glycemic control and cardiovascular risk in obese patients with type 2 diabetes. Curr Opin Endocrinol Diabetes Obes. 2016;23:150–6.
Ren X, Chen ZA, Zheng S, Han T, Li Y, Liu W.et al. Association between Triglyceride to HDL-C Ratio (TG/HDL-C) and Insulin Resistance in Chinese Patients with Newly Diagnosed Type 2 Diabetes Mellitus. PLOS One. 2016;11:e0154345 10.1371%2Fjournal.pone.0154345.
Salazar MR, Carbajal HA, Espeche WG, Aizpurua M, Marillet AG, Leiva Sisnieguez CE, et al. Use of the triglyceride/high-density lipoprotein cholesterol ratio to identify cardiometabolic risk: impact of obesity? J Investig Med. 2017;65:323–7.
Dabelea D, Pihoker C, Talton JW, D’Agostino RB Jr., Fujimoto W, Klingensmith GJ, et al. Etiological approach to characterization of diabetes type: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2011;34:1628–33.
Hastie TJ. Generalized additive models (Chapter 7). In: Chambers JM, Hastie T, editors. Statistical models in S. Grove, CA: Wadsworth & Brooks: Pacific; 1992.
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, et al. pROC: an open-source package for R and S + to analyze and compare ROC curves. BMC Bioinformatics. 2011;12:77
Davison AC, Hinkley DV. Bootstrap methods and their applications. Cambridge: Cambridge University Press; 1997.
Canty A. Ripley B Bootstrap R (S-Plus) Functions: boot: R package version 1.3-20, 2017.
Graves L, Garnett SP, Cowell CT, Baur LA, Ness A, Sattar N, et al. Waist-to-height ratio and cardiometabolic risk factors in adolescence: findings from a prospective birth cohort. Pediatr Obes. 2014;9:327–38.
Harding S, Silva MJ, Molaodi OR, Enayat ZE, Cassidy A, Karamanos A, et al. Longitudinal study of cardiometabolic risk from early adolescence to early adulthood in an ethnically diverse cohort. BMJ Open. 2016;6:e013221
Kondaki K, Grammatikaki E, Pavon DJ, Manios Y, Gonzalez-Gross M, Sjostrom M, et al. Comparison of several anthropometric indices with insulin resistance proxy measures among European adolescents: The Helena Study. Eur J Pediatr. 2011;170:731–9.
Liang J, Fu J, Jiang Y, Dong G, Wang X.Wu W, TriGlycerides and high-density lipoprotein cholesterol ratio compared with homeostasis model assessment insulin resistance indexes in screening for metabolic syndrome in the chinese obese children: a cross section study. BMC Pediatr. 2015;15:138.
Johnson ST, Kuk JL, Mackenzie KA, Huang TT, Rosychuk RJ, Ball GD. Metabolic risk varies according to waist circumference measurement site in overweight boys and girls. J Pediatr. 2010;156:247–52 e241.
Shen W, Punyanitya M, Chen J, Gallagher D, Albu J, Pi-Sunyer X, et al. Visceral adipose tissue: relationships between single slice areas at different locations and obesity-related health risks. Int J Obes (Lond). 2007;31:763–9. .
Demerath EW, Reed D, Rogers N, Sun SS, Lee M, Choh AC, et al. Visceral adiposity and its anatomical distribution as predictors of the metabolic syndrome and cardiometabolic risk factor levels. Am J Clin Nutr. 2008;88:1263–71.
Kvist H, Chowdhury B, Grangard U, Tylen U, Sjostrom L. Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: predictive equations. Am J Clin Nutr. 1988;48:1351–61.
O’Connor M, Ryan J, Foley S. Best single-slice location to measure visceral adipose tissue on paediatric CT scans and the relationship between anthropometric measurements, gender and VAT volume in children. Br J Radiol. 2015;88:20140711.
Huang TT, Johnson MS, Gower BA, Goran MI. Effect of changes in fat distribution on the rates of change of insulin response in children. Obes Res. 2002;10:978–84.
Ali O, Cerjak D, Kent JW Jr., James R, Blangero J, Zhang Y. Obesity, central adiposity and cardiometabolic risk factors in children and adolescents: a family-based study. Pediatr Obes [Internet]. 2014;9:e58–62.
Liu LL, Kahn HS, Pettitt DJ, Fino NF, Morgan T, Maahs DM, et al. Comparing two waist-to-height ratio measurements with cardiometabolic risk factors among youth with diabetes. Int J Child Health Nutr. 2016;5:87–94.
Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and risk of the adult metabolic syndrome: a systematic review. Int J Obes (Lond). 2012; 36:1–11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3255098/pdf/ijo2011186a.pdf; Accessed 26 June 2018.
Schmidt MD, Dwyer T, Magnussen CG, Venn AJ. Predictive associations between alternative measures of childhood adiposity and adult cardio-metabolic health. Int J Obes (Lond). 2011;35:38–45.
Ross R, Berentzen T, Bradshaw AJ, Janssen I, Kahn HS, Katzmarzyk PT, et al. Does the relationship between waist circumference, morbidity and mortality depend on measurement protocol for waist circumference? Obes Rev. 2008;9:312–25.
Mason C, Katzmarzyk PT. Effect of the site of measurement of waist circumference on the prevalence of the metabolic syndrome. Am J Cardiol. 2009;103:1716–20.
Owens S, Litaker M, Allison J, Riggs S, Ferguson M, Gutin B. Prediction of visceral adipose tissue from simple anthropometric measurements in youths with obesity. Obes Res. 1999;7:16–22.
Weber DR, Levitt Katz LE, Zemel BS, Gallagher PR, Murphy KM, Dumser SM, et al. Anthropometric measures of abdominal adiposity for the identification of cardiometabolic risk factors in adolescents. Diabetes Res Clin Pract. 2014;103:e14–17.
Labyak CA, Johnson TM. Sagittal abdominal diameter: a novel anthropometric measure for predicting visceral fat and associated cardiometabolic risk factors in children. Top Clin Nutr. 2015;30:153–8.
da Silva CC, Vasques ACJ, Zambon MP, Camilo DF, De Bernardi Rodrigues AM, Antonio M, et al. Sagittal abdominal diameter resembles waist circumference as a surrogate marker of insulin resistance in adolescents-Brazilian Metabolic Syndrome Study. Pediatr Diabetes. 2018;19:882–91.
Kahn HS, Bullard KM. Indicators of abdominal size relative to height associated with sex, age, socioeconomic position and ancestry among US adults. PLOS One. 2017;12:e0172245; https://doi.org/10.1371/journal.pone.0172245.
Acknowledgements
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families, and their health care providers, whose participation made this study possible. SEARCH 3/4: The authors wish to acknowledge the involvement of the Kaiser Permanente Southern California’s Clinical Research Center (funded by Kaiser Foundation Health Plan and supported in part by the Southern California Permanente Medical Group; the South Carolina Clinical & Translational Research Institute, at the Medical University of South Carolina, NIH/National Center for Advancing Translational Sciences (NCATS) grant number UL1 TR000062, UL1 Tr001450; Seattle Children’s Hospital and the University of Washington, NIH/NCATS grant number UL1 TR00423; University of Colorado Pediatric Clinical and Translational Research Center, NIH/NCATS grant Number UL1 TR000154; the Barbara Davis Center at the University of Colorado at Denver (DERC NIH grant number P30 DK57516); the University of Cincinnati, NIH/NCATS grant number UL1 TR000077, UL1 TR001425; and the Children with Medical Handicaps program managed by the Ohio Department of Health. This study includes data provided by the Ohio Department of Health, which should not be considered an endorsement of this study or its conclusions. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
Funding
Grant Support (SEARCH 3): SEARCH for Diabetes in Youth is funded by the Centers for Disease Control and Prevention (PA numbers 00097, DP-05-069, and DP-10-001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Grant Support (SEARCH 4): The SEARCH for Diabetes in Youth Cohort Study (1UC4DK108173) is funded by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases and supported by the Centers for Disease Control and Prevention. The Population Based Registry of Diabetes in Youth Study (1U18DP006131, U18DP006133, U18DP006134, U18DP006136, U18DP006138, U18DP006139) is funded by the Centers for Disease Control and Prevention and supported by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Sites (SEARCH 3/4): Kaiser Permanente Southern California (U18DP006133, U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U18DP006139, U48/CCU819241-3, U01 DP000247, and U18DP000247-06A1), Cincinnati’s Children’s Hospital Medical Center (U18DP006134, U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U18DP006138, U48/CCU419249, U01 DP000254, and U18DP002708), Seattle Children’s Hospital (U18DP006136, U58/CCU019235-4, U01 DP000244, and U18DP002710-01), Wake Forest University School of Medicine (U18DP006131, U48/CCU919219, U01 DP000250, and 200-2010-35171).
Author information
Authors and Affiliations
Contributions
HSK conceived this work and drafted the initial paper. JD contributed substantially to the research design and directed the statistical analyses. NFF organized data and assisted with analyses. All authors participated in the acquisition of data, interpretation of the results, and review of the final paper. HSK confirms he had full access to the data in the study and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kahn, H.S., Divers, J., Fino, N.F. et al. Alternative waist-to-height ratios associated with risk biomarkers in youth with diabetes: comparative models in the SEARCH for Diabetes in Youth Study. Int J Obes 43, 1940–1950 (2019). https://doi.org/10.1038/s41366-019-0354-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0354-8