Abstract
Background/objectives
Bariatric surgery leads to type 2 diabetes mellitus (T2DM) remission, but recurrence can ensue afterwards. However, literature provides heterogenous remission/recurrence criteria and there is no consensus on long-term T2DM management after surgery. We aim to assess T2DM remission/recurrence rates using standardized criteria and to identify relapse predictors. We also intend to analyze the management of residual T2DM and the impact of maintaining/withdrawing metformin in avoiding future relapse.
Subjects/methods
We investigated a cohort of 110 obese patients with T2DM who underwent bariatric surgery and were followed for 5 years (Y0–Y5). Patients who ever attained remission were accounted for cumulate remission, while prevalent remission was considered for individuals who were on remission in a specific visit.
Results
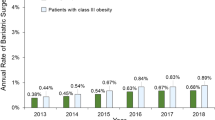
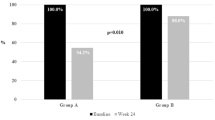
A complete prevalent remission of 47.3% was reached at Y1 and it remained stable till Y5 (46.4–48.2%). Complete cumulative rate was of 57.3% at Y5. Five-year T2DM recurrence rate was 15.9% and it was associated with higher pre-operative HbA1c levels (β = 1.06; p < 0.05) and a milder excess body weight loss (EBWL) (β = 0.49; p < 0.05). Glucose-lowering agents were fully stopped in 51.4% of the patients till Y1 and in 16.2% of them afterwards. Medication withdrawal was mainly attempted in patients with a lower baseline HbA1c (β = 0.54; p < 0.01) and higher first-year EBWL (β = 1.04; p < 0.01). Patients that kept metformin after reaching a HbA1c in the complete remission range (<6.0%) did not have greater odds of avoiding relapse in the next visit (OR = 0.33; p = 0.08).
Conclusions
Baseline HbA1c and EBWL were the main variables driving both T2DM relapse after bariatric surgery and the attempt to withdrawal anti-diabetic medication. In our population keeping metformin once an HbA1c < 6.0% is achieved did not seem to diminish relapse but further studies on this matter are needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Verma S, Hussain ME. Obesity and diabetes: an update. Diabetes Metab Syndr. 2017;11:73–9.
Souteiro P, Belo S, Neves JS, Magalhaes D, Silva RB, Oliveira SC, et al. Preoperative beta cell function is predictive of diabetes remission after bariatric surgery. Obes Surg. 2017;27:288–94.
American Diabetes Association Guidelines. Standards of medical care in diabetes—2017. Diabetes Care 40(Suppl 1):S1–S135.
Iacobellis G, Xu C, Campo RE, De La Cruz-Munoz NF. Predictors of short-term diabetes remission after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2015;25:782–7.
Schauer PR, Burguera B, Ikramuddin S, Cottam D, Gourash W, Hamad G, et al. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238:467–84. discussion84–5
Isaman DJ, Rothberg AE, Herman WH. Reconciliation of Type 2 diabetes remission rates in studies of Roux-en-Y gastric bypass. Diabetes Care. 2016;39:2247–53.
Brethauer SA, Aminian A, Romero-Talamas H, Batayyah E, Mackey J, Kennedy L, et al. Can diabetes be surgically cured? Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258:628–36. discussion36–7
Arterburn DE, Bogart A, Sherwood NE, Sidney S, Coleman KJ, Haneuse S, et al. A multisite study of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass. Obes Surg. 2013;23:93–102.
Still CD, Wood GC, Benotti P, Petrick AT, Gabrielsen J, Strodel WE, et al. Preoperative prediction of type 2 diabetes remission after Roux-en-Y gastric bypass surgery: a retrospective cohort study. Lancet Diabetes Endocrinol. 2014;2:38–45.
Robert M, Ferrand-Gaillard C, Disse E, Espalieu P, Simon C, Laville M, et al. Predictive factors of type 2 diabetes remission 1 year after bariatric surgery: impact of surgical techniques. Obes Surg. 2013;23:770–5.
Busetto L, Dicker D, Azran C, Batterham RL, Farpour-Lambert N, Fried M, et al. Practical recommendations of the obesity management task force of the European Association for the study of obesity for the post-bariatric surgery medical management. Obes Facts. 2017;10:597–632.
Heber D, Greenway FL, Kaplan LM, Livingston E, Salvador J, Still C. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:4823–43.
Dicker D, Yahalom R, Comaneshter DS, Vinker S. Long-term outcomes of three types of bariatric surgery on obesity and type 2 diabetes control and remission. Obes Surg. 2016;26:1814–20.
Halpern B, Cercato C, Mancini MC. Diabetes remission off medications is not a suitable endpoint for comparing bariatric/metabolic surgery with pharmacotherapy. Diabetologia. 2016;59:2040–1.
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11:489–506.
Yu J, Zhou X, Li L, Li S, Tan J, Li Y, et al. The long-term effects of bariatric surgery for type 2 diabetes: systematic review and meta-analysis of randomized and non-randomized evidence. Obes Surg. 2015;25:143–58.
Bojsen-Moller KN, Dirksen C, Jorgensen NB, Jacobsen SH, Serup AK, Albers PH, et al. Early enhancements of hepatic and later of peripheral insulin sensitivity combined with increased postprandial insulin secretion contribute to improved glycemic control after Roux-en-Y gastric bypass. Diabetes. 2014;63:1725–37.
Cho YM. A gut feeling to cure diabetes: potential mechanisms of diabetes remission after bariatric surgery. Diabetes Metab J. 2014;38:406–15.
Penney NC, Kinross J, Newton RC, Purkayastha S. The role of bile acids in reducing the metabolic complications of obesity after bariatric surgery: a systematic review. Int J Obes. 2015;39:1565–74.
DiGiorgi M, Rosen DJ, Choi JJ, Milone L, Schrope B, Olivero-Rivera L, et al. Re-emergence of diabetes after gastric bypass in patients with mid- to long-term follow-up. Surg Obes Relat Dis. 2010;6:249–53.
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Nanni G, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386:964–73.
de Oliveira VLP, Martins GP, Mottin CC, Rizzolli J, Friedman R. Predictors of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass in severely obese patients. Obes Surg. 2018;28:195–203.
Zhong MW, Liu SZ, Zhang GY, Zhang X, Liu T, Hu SY. Alterations in gut microbiota during remission and recurrence of diabetes after duodenal-jejunal bypass in rats. World J Gastroenterol. 2016;22:6706–15.
Vouri SM, Chen J, Sparkman J, Salles A, Micek ST. Antidiabetic medication de-escalation following bariatric surgery. J Diabetes. 2018;10:768–70.
Kashyap SR, Schauer P. Clinical considerations for the management of residual diabetes following bariatric surgery. Diabetes Obes Metab. 2012;14:773–79.
Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2019 Executive Summary. Endocr Pract. 2018;24:91–120.
Sjostrom L, Narbro K, Sjostrom CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Sjostrom L, Peltonen M, Jacobson P, Sjostrom CD, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65.
Heneghan HM, Cetin D, Navaneethan SD, Orzech N, Brethauer SA, Schauer PR. Effects of bariatric surgery on diabetic nephropathy after 5 years of follow-up. Surg Obes Relat Dis. 2013;9:7–14.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89.
Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular outcomes in type 1 diabetes: the DCCT/EDIC study 30-year follow-up. Diabetes Care. 2016;39:686–93.
Coleman KJ, Haneuse S, Johnson E, Bogart A, Fisher D, O’Connor PJ, et al. Long-term microvascular disease outcomes in patients with type 2 diabetes after bariatric surgery: evidence for the legacy effect of surgery. Diabetes Care. 2016;39:1400–7.
Aminian A, Brethauer SA, Andalib A, Nowacki AS, Jimenez A, Corcelles R, et al. Individualized metabolic surgery score: procedure selection based on diabetes severity. Ann Surg. 2017;266:650–7.
Larjani S, Spivak I, Hao Guo M, Aliarzadeh B, Wang W, Robinson S, et al. Preoperative predictors of adherence to multidisciplinary follow-up care postbariatric surgery. Surg Obes Relat Dis. 2016;12:350–6.
Souteiro P, Pedro J, Magalhães D, Neves J, Oliveira S, Belo S, et al. Patients’ follow-up adherence after bariatric surgery. Obes Facts. 2017;10(Suppl 1):1–259. T3P152
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Souteiro, P., Belo, S., Magalhães, D. et al. Long-term diabetes outcomes after bariatric surgery—managing medication withdrawl. Int J Obes 43, 2217–2224 (2019). https://doi.org/10.1038/s41366-019-0320-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0320-5
This article is cited by
-
Effect of Bariatric Surgery on Metabolic Syndrome in Chinese Patients with Low Body Mass Index: a Propensity Score Matching Study
Obesity Surgery (2023)
-
Predictors of normalized HbA1c after gastric bypass surgery in subjects with abnormal glucose levels, a 2-year follow-up study
Scientific Reports (2020)
-
Impact of Bariatric Surgery on Long-term Cardiovascular Risk: Comparative Effectiveness of Different Surgical Procedures
Obesity Surgery (2020)