Abstract
Background/objectives
Although weight change has been studied in relation to many individual chronic conditions, limited studies have focused on weight change and multimorbidity. This study examines the relationship between short-term weight change and the accumulation of multimorbidity in midlife.
Methods
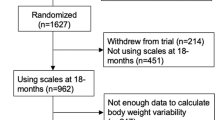
We used data from 7357 women aged 45–50 years without a history of any chronic conditions. The women were surveyed approximately every 3 years from 1996 to 2016. Associations between short-term weight change and accumulation of multimorbidity (two or more of nine chronic conditions) over each 3-year period, adjusting for baseline body mass index (BMI) or time-varying BMI (3-year period), were examined using repeated measures models. Short-term weight change was categorised into seven groups of annual weight change from high weight loss ( ≤ −5%) to high weight gain (> + 5%).
Results
Over 20 years, 60.4% (n = 4442) of women developed multimorbidity. Baseline BMI, time-varying BMI and short-term weight gain were all associated with the accumulation of multimorbidity. After controlling for sociodemographic, lifestyle factors and menopausal status, high weight gain was associated with a 25% increased odds of multimorbidity (odds ratio (OR) 1.25, 95% confidence interval (CI) 1.08–1.45) compared with maintaining a stable weight. The results were consistent among models adjusting for baseline BMI (OR 1.24, 95% CI 1.07–1.44) or time-varying BMI (OR 1.34, 95% CI 1.16–1.54). Weight loss was associated with increased odds of multimorbidity in women with normal BMI (baseline or time-varying).
Conclusions
Short-term weight gain is associated with significantly increased odds of multimorbidity in mid-aged women. This association is independent from baseline BMI (at 45–50 years) and time-varying BMI. These findings support a persistent weight management regime and prevention of weight gain throughout women’s midlife.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Gregg EW, Shaw JE. Global health effects of overweight and obesity. N Engl J Med. 2017;377:80–81.
Xu X, Mishra GD, Jones M. Evidence on multimorbidity from definition to intervention: an overview of systematic reviews. Ageing Res Rev. 2017;37:53–68.
Kingston A, Robinson L, Booth H, Knapp M, Jagger C, project M. Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing. 2018;47:374–80.
Mishra GD, Carrigan G, Brown WJ, Barnett AG, Dobson AJ. Short-term weight change and the incidence of diabetes in midlife: results from the Australian Longitudinal Study on Women’s Health. Diabetes Care. 2007;30:1418–24.
Keum N, Greenwood DC, Lee DH, Kim R, Aune D, Ju W et al. Adult weight gain and adiposity-related cancers: a dose-response meta-analysis of prospective observational studies. J Natl Cancer Inst. 2015;107:pii: djv088.
Stokes A, Preston SH. Revealing the burden of obesity using weight histories. Proc Natl Acad Sci USA. 2016;113:572–7.
Kivimaki M, Kuosma E, Ferrie JE, Luukkonen R, Nyberg ST, Alfredsson L, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. 2017;2:e277–e285.
Preston SH, Mehta NK, Stokes A. Modeling obesity histories in cohort analyses of health and mortality. Epidemiology. 2013;24:158–66.
Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364:2392–404.
Wang Z, Peng Y, Dong B. Is body mass index associated with lowest mortality increasing over time? Int J Obes (Lond). 2017;41:1171–5.
Dixon JB, Egger GJ, Finkelstein EA, Kral JG, Lambert GW. ‘Obesity paradox’ misunderstands the biology of optimal weight throughout the life cycle. Int J Obes (Lond). 2015;39:82–4.
Brown WJ, Williams L, Ford JH, Ball K, Dobson AJ. Identifying the energy gap: magnitude and determinants of 5-year weight gain in midage women. Obes Res. 2005;13:1431–41.
Byles J, Hockey R, McLaughlin D, Dobson A, Brown W, Loxton D et al. Chronic conditions, physical function and health care use: Findings from the Australian Longitudinal Study on Women’s Health. Report prepared for the Australian Government Department of Health. 2015.
Gomersall SR, Dobson AJ, Brown WJ. Weight gain, overweight, and obesity: determinants and health outcomes from the Australian Longitudinal Study on Women’s Health. Curr Obes Rep. 2014;3:46–53.
Smith SC, Bonow RO, Creager MA, Gibbons RJ, Hiratzka LF, Lloyd-Jones DM, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation (vol 124, pg 2458, 2011). Circulation. 2015;131:E408–E408.
Jackson CA, Dobson A, Tooth L, Mishra GD. Body mass index and socioeconomic position are associated with 9-year trajectories of multimorbidity: a population-based study. Prev Med. 2015;81:92–8.
Pack QR, Rodriguez-Escudero JP, Thomas RJ, Ades PA, West CP, Somers VK, et al. The prognostic importance of weight loss in coronary artery disease: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89:1368–77.
Moholdt T, Lavie CJ, Nauman J. Sustained physical activity, not weight loss, associated with improved survival in coronary heart disease. J Am Coll Cardiol. 2018;71:1094–101.
Academy of Medical Sciences. Multimorbidity: a priority for global health research. Academy of Medical Sciences: London, 2018.
Morris RL, Sanders C, Kennedy AP, Rogers A. Shifting priorities in multimorbidity: a longitudinal qualitative study of patient’s prioritization of multiple conditions. Chronic Illn. 2011;7:147–61.
Lee C, Dobson AJ, Brown WJ, Bryson L, Byles J, Warner-Smith P, et al. Cohort Profile: the Australian Longitudinal Study on Women’s Health. Int J Epidemiol. 2005;34:987–91.
Dobson AJ, Hockey R, Brown WJ, Byles JE, Loxton DJ, McLaughlin D, et al. Cohort profile update: Australian Longitudinal Study on Women’s Health. Int J Epidemiol. 2015;44:1547–1547f.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. World Health Organization: Geneva, 2000. Report no. 9241208945.
Australian Institute of Health and Welfare. The National Health Priority Areas. 2012.
Brown WJ, Trost SG, Bauman A, Mummery K, Owen N. Test-retest reliability of four physical activity measures used in population surveys. J Sci Med Sport. 2004;7:205–15.
Mishra GD, Dobson AJ. Using longitudinal profiles to characterize women’s symptoms through midlife: results from a large prospective study. Menopause. 2012;19:549–55.
Xu X, Mishra GD, Dobson AJ, Jones M. Progression of diabetes, heart disease, and stroke multimorbidity in middle-aged women: a 20-year cohort study. PLoS Med. 2018;15:18.
Canizares M, Hogg-Johnson S, Gignac MAM, Glazier RH, Badley EM. Increasing trajectories of multimorbidity over time: birth cohort differences and the role of changes in obesity and income. J Gerontol B Psychol Sci Soc Sci. 2018;73:1303–14.
Zheng Y, Manson JE, Yuan C, Liang MH, Grodstein F, Stampfer MJ, et al. Associations of weight gain from early to middle adulthood with major health outcomes later in life. JAMA. 2017;318:255–69.
Rueda-Clausen CF, Ogunleye AA, Sharma AM. Health benefits of long-term weight-loss maintenance. Annu Rev Nutr. 2015;35:475–516.
Oktay AA, Lavie CJ, Kokkinos PF, Parto P, Pandey A, Ventura HO. The interaction of cardiorespiratory fitness with obesity and the obesity paradox in cardiovascular disease. Prog Cardiovasc Dis. 2017;60:30–44.
Kennedy AB, Lavie CJ, Blair SN. Fitness or fatness: which is more important? JAMA. 2018;319:231–2.
Lam J, Lord SJ, Hunter KE, Simes RJ, Vu T, Askie LM. Australian clinical trial activity and burden of disease: an analysis of registered trials in National Health Priority Areas. Med J Aust. 2015;203:97–101.
Dhalwani NN, O’Donovan G, Zaccardi F, Hamer M, Yates T, Davies M, et al. Long terms trends of multimorbidity and association with physical activity in older English population. Int J Behav Nutr Phys Act. 2016;13:8.
Yang Y, Lee LC. Dynamics and heterogeneity in the process of human frailty and aging: evidence from the us older adult population. J Gerontol B Psychol Sci Soc Sci. 2010;65:246–55.
Holowko N, Jones M, Koupil I, Tooth L, Mishra G. Combined effect of education and reproductive history on weight trajectories of young Australian women: a longitudinal study. Obes (Silver Spring). 2016;24:2224–31.
Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–103.
Hansen H, Schafer I, Schon G, Riedel-Heller S, Gensichen J, Weyerer S, et al. Agreement between self-reported and general practitioner-reported chronic conditions among multimorbid patients in primary care–results of the MultiCare Cohort Study. BMC Fam Pract. 2014;15:1–14.
Burton NW, Brown W, Dobson A. Accuracy of body mass index estimated from self-reported height and weight in mid-aged Australian women. Aust N Z J Public Health. 2010;34:620–3.
Navin Cristina TJ, Stewart Williams JA, Parkinson L, Sibbritt DW, Byles JE. Identification of diabetes, heart disease, hypertension and stroke in mid- and older-aged women: Comparing self-report and administrative hospital data records. Geriatr Gerontol Int. 2015;16:95–102.
Stavrou E, Vajdic CM, Loxton D, Pearson SA. The validity of self-reported cancer diagnoses and factors associated with accurate reporting in a cohort of older Australian women. Cancer Epidemiol. 2011;35:e75–80.
Harber MP, Kaminsky LA, Arena R, Blair SN, Franklin BA, Myers J, et al. Impact of cardiorespiratory fitness on all-cause and disease-specific mortality: advances since 2009. Prog Cardiovasc Dis. 2017;60:11–20.
Nauman J, Tauschek LC, Kaminsky LA, Nes BM, Wisloff U. Global fitness levels: findings from a web-based surveillance report. Prog Cardiovasc Dis. 2017;60:78–88.
Xu X, Mishra GD, Jones M. Mapping the global research landscape and knowledge gaps on multimorbidity: a bibliometric study. J Glob Health. 2017;7:010414.
Katzmarzyk PT, Lee IM, Martin CK, Blair SN. Epidemiology of physical activity and exercise training in the United States. Prog Cardiovasc Dis. 2017;60:3–10.
Acknowledgements
This work was supported by the Australian Government Department of Health. XX holds an International Postgraduate Research Scholarship from the Australian government and a UQ Centennial Scholarship from The University of Queensland. GDM holds a National Health and Medical Research Council Principal Research Fellowship (APP1121844).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state that they have no conflicts of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Xu, X., Mishra, G.D., Dobson, A.J. et al. Short-term weight gain is associated with accumulation of multimorbidity in mid-aged women: a 20-year cohort study. Int J Obes 43, 1811–1821 (2019). https://doi.org/10.1038/s41366-018-0250-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0250-7