Abstract
Background and Objective
Intermittent energy restriction (IER) is an alternative to continuous energy restriction (CER) for weight loss. There are few long-term trials comparing efficacy of these methods. The objective was to compare the effects of CER to two forms of IER; a week-on-week-off energy restriction and a 5:2 program, during which participants restricted their energy intake severely for 2 days and ate as usual for 5 days, on weight loss, body composition, blood lipids, and glucose.
Subjects and Methods
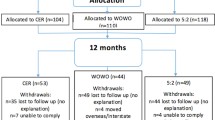
A one-year randomized parallel trial was conducted at the University of South Australia, Adelaide, Australia. Participants were 332 overweight and obese adults, ages 18–72 years, who were randomized to 1 of 3 groups: CER (4200 kJ/day for women and 5040 kJ/day for men), week-on-week-off energy restriction (alternating between the same energy restriction as the continuous group for one week and one week of habitual diet), or 5:2 (2100 kJ/day on modified fast days each week for women and 2520 kJ/day for men, the 2 days of energy restriction could be consecutive or non-consecutive). Primary outcome was weight loss, and secondary outcomes were changes in body composition, blood lipids, and glucose.
Results
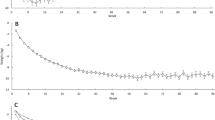
For the 146 individuals who completed the study (124 female, 22 male, mean BMI 33 kg/m2) mean weight loss, and body fat loss at 12 months was similar in the three intervention groups, −6.6 kg for CER, −5.1 kg for the week-on, week-off and −5.0 kg for 5:2 (p = 0.2 time by diet). Discontinuation rates were not different (p = 0.4). HDL-cholesterol rose (7%) and triglycerides decreased (13%) at 12 months with no differences between groups. No changes were seen for fasting glucose or LDL-cholesterol.
Discussion and Conclusion
The two forms of IER were not statistically different for weight loss, body composition, and cardiometabolic risk factors compared to CER.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
06 March 2019
Table 4 is still missing from both versions. It was labeled Table 3 in the first version but a reviewer wanted an extra table in the methods which became Table 1.
References
World Health Organization. Obesity and overweight World Health Organization. 2015. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 1 April 2015.
Scherer PE, Hill AJ. Obesity, diabetes, and cardiovascular diseases: a compendium. Circ Res. 2016;118:1703–5.
Wearing SC, Henning EM, Byrne NM, Steele JR, Hills AP. Musculoskeletal disorders associated with obesity: a biochemical perspective. Obes Rev. 2006;7:239–50.
Anderson JW, Kendall CW, Jenkins DJ. Importance of weight management in type 2 diabetes: review with meta-analysis of clinical studies. J Am Coll Nutr. 2003;22:331–9.
Aucott L, Poobalan A, Smith WCS, Avenell A, Jung R, Broom J, et al. Weight loss in obese diabetic and non-diabetic indviduals and long-term diabetes outcomes—a systematic review. Diabetes Obes Metab. 2004;6:85–94.
Barr ELM, Magliano DJ, Zimmet PZ, Polkinghorne KR, Atkins RC, Dunstan DW, et al. AusDiab 2005: The Australian Diabetes, Obesity and Lifestyle Study—tracking the accelerating epidemic: its causes and outcomes. Melbourne: Internationl Diabetes Institute; 2006.
Harvey AE, Lashinger LM, Hursting SD. The growing challenge of obesity and cancer: an inflammatory issue. Ann N Y Acad Sci. 2011;1229:45–52.
Vucenik I, Stains JP. Obesity and cancer risk: evidence, mechanisms, and recommendations. Ann N Y Acad Sci. 2012;1271:37–43.
Varady KA. Intermittent versus daily calorie restriction: which diet regimen is more effective for weight loss? Obes Rev. 2011;12:e593–601.
Wing RR, Jeffery RW. Prescribed “Breaks” as a means to disrupt weight control efforts. Obes Res. 2003;11:287–91.
Harvie M, Pegington M. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: a randomized trial in young overweight women. Int J Obes. 2011;35:714–27.
Harvie M, Wright C, Pegington M, McMullan D, Mitchell E, Martin B, et al. The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br J Nutr. 2013;110:1534–47.
Conley M, Le Fevre L, Haywood C, Proietto J. Is two days of intermittent energy restirction per week a feasible weight loss approach in obese males? A randomsied pilot study. Nutr Diet. 2017;75:65–72. Australia
Keogh JB, Pedersen E, Petersen KS, Clifton PM. Effects of intermittent compared to continuous energy restriction on short-term weight loss and long-term weight loss maintenance. Clin Obes. 2014;4:150–6.
Byrne NM, Sainsbury A, King NA, Hills AP, Wood RE. Intermittent energy restriction improves weight loss efficiency in obese men: the MATADOR study. Int J Obes. 2017;42:129–38.
Headland M, Clifton PM, Carter S, Keogh JB. Weight loss outcomes: a systematic review and meta-analysis of intermittent energy restriction trials lasting a minimum of 6 months. Nutrients. 2015;8:1–12.
Trepanowski JF, Kroeger CM, Barnosky AR, Klempel M, Bhutani S, Hoddy KK, et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults a randomized clinical trial. JAMA Intern Med. 2017;177:930–8.
Sundfor TM, Svendsen M, Tonstad S. Effect of intermittent versus continuous energy restriction on weight loss, maintenance and cardiometabolic risk: a randomized 1-year trial. Nutr Metab Cardiovasc Dis. 2018;28:698–706.
Noakes M, Keogh JB, Foster PR, Clifton PM. Effect of an energy-restricted, high-protein, low-fat diet relative to a conventional high-carbohydrate, low-fat diet on weight loss, body composition, nutritional status, and markers of cardiovascular health in obese women. Am J Clin Nutr. 2005;81:1298–306.
Seimon RV, Roekenes JA, Zibellini J, Zhu B, Gibson AA, Hills AP, et al. Do intermittent diets provide physiological benefits over continuous diets for weight loss? A systematic review of clinical trials. Mol Cell Endocrinol. 2015;418 Pt 2:153–72.
Bhutani S, Klempel M, Kroeger CM, Trepanowski JF, Varady KA. Alternate day fasting and endurance exercise combine to reduce body weight and favourably alter plasma lipids in obese humans. Obesity. 2013;21:1370–9.
Hoddy KK, Kroeger CM, Trepanowski JF, Barnosky A, Bhutani S, Varady KA. Meal timing during alternate day fasting: impact on body weight and cardiovascular disease risk in obese adults. [Erratum appears in Obesity. 2014;23:914]. Obesity. 2014;22:2524–31.
Klempel MC, Kroeger CM, Varady KA. Alternate day fasting (ADF) with a high-fat diet produces similar weight loss and cardio-protection as ADF with a low-fat diet. Metabolism. 2013;62:137–43.
Varady KA, Bhutani S, Church EC, Klempel MC. Short-term modified alternate-day fasting: a novel dietary strategy for weight loss and cardioprotection in obese adults. Am J Clin Nutr. 2009;90:1138–43.
Trepanowski JF, Kroeger CM, Barnosky A, Klempel MC, Bhutani S, Hoddy KK, et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern Med. 2017;177:930–8.
Byrne NM, Sainsbury A, King NA, Hills AP, Wood RE. Intermittent energy restriction improves weight loss efficiency in obese men: the MATADOR study. Int J Obes. 2017;42:129–38.
The National Health and Medical Research Council. National evidence based guideline for case detection and diagnosis of type 2 diabetes. Australia, 2009.
Acknowledgements
We thank Eva Pedersen for her assistance with study preparation and study participants. PMC is supported by an NHMRC Principal Research Fellowship. MLH was supported by a University of South Australia Postgraduate Award, funded jointly by the University of South Australia and the Research Training Program.
Author information
Authors and Affiliations
Contributions
PMC and JKB designed the research; MLH: conducted the research and had primary responsibility for the final content on the manuscript; MLH and PMC: analyzed data; and all authors: wrote the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Headland, M.L., Clifton, P.M. & Keogh, J.B. Effect of intermittent compared to continuous energy restriction on weight loss and weight maintenance after 12 months in healthy overweight or obese adults. Int J Obes 43, 2028–2036 (2019). https://doi.org/10.1038/s41366-018-0247-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0247-2
This article is cited by
-
Network meta-analysis of three different forms of intermittent energy restrictions for overweight or obese adults
International Journal of Obesity (2024)
-
Comparison of weight loss induced by daily caloric restriction versus intermittent fasting (DRIFT) in individuals with obesity: study protocol for a 52-week randomized clinical trial
Trials (2022)
-
Diet composition influences the metabolic benefits of short cycles of very low caloric intake
Nature Communications (2021)
-
Time-Restricted Eating, Intermittent Fasting, and Fasting-Mimicking Diets in Weight Loss
Current Obesity Reports (2021)
-
Effect of intermittent versus continuous calorie restriction on body weight and cardiometabolic risk markers in subjects with overweight or obesity and mild-to-moderate hypertriglyceridemia: a randomized trial
Lipids in Health and Disease (2020)