Abstract
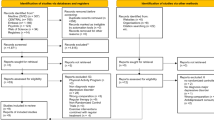
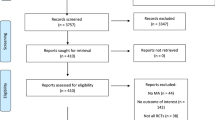
There are conflicting findings regarding the effect very low calorie diets (VLCDs) have on self-reported depressive symptoms and anxiety levels. Some studies have reported decreased subjective depressive symptoms and anxiety post-diet, whereas other studies have not. Further complicating matters, the protocol for VLCDs vary substantially across studies, which could account for the mixed findings. The primary goal of this meta-analysis and systematic review was to determine the effect VLCDs have on subjective depressive symptoms and anxiety pre- to post-diet. In addition, potential moderators (the presence/absence of behavioral therapy, duration of diet, inclusion/exclusion of low intensity exercise, and amount of weight lost) were examined to assess the effect of procedural deviations across VLCD studies on depressive symptoms and anxiety. A random-effects model was used for the meta-analysis and included nine studies with 16 independent samples. To further explain the results, study rigor was examined in the systematic review, which included 11 studies with 20 independent samples. Depressive symptoms significantly decreased pre- to post-diet when behavioral therapy was implemented during the diet, the duration of the diet was relatively long (8–16 weeks), low intensity exercise was included, and the dieters lost 14.1 kg or more post-diet. However, no difference in depressive symptoms were observed pre- to post-diet when behavioral therapy was not included, the diet was shorter (1–7 weeks), no exercise was implemented and dieters lost <14 kg of weight post-diet. There was no change in anxiety pre- to post-diet. Health care providers involved in supervising VLCDs should consider using a VLCD of at least 8 weeks that includes behavioral therapy and low intensity exercise in order to enhance the potential benefits of VLCDs on depressive symptoms. More research is required to examine the effect of VLCDs on anxiety.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References (*Studies included in the final sample of the meta-analysis and systematic review are marked with an asterisk.)
Chen S, Yan E. Very-low-calorie diet revisited. Obes Manag. 2006;2:31–32.
Tsai AG, Wadden TA. The evolution of very-low-calorie diets: an update and meta-analysis. Obesity. 2006;14:1283–93.
Saris WHM. Very-low-calorie diets and sustained weight loss. Obes Res. 2001;9:295S–301S.
Parretti HM, Jebb SA, Johns DJ, Lewis AL, Christian-Browng AM, Aveyard P. Clinical effectiveness of very-low-energy diets in the management of weight loss: a systematic review and meta-analysis of randomized controlled trails. Obes Rev. 2016;17:225–34.
Sumithran P, Proietto J. Very-low-calorie diets (VLCDs) for the treatment of obesity. In: Gill T(ed). Managing and preventing obesity. Cambridge: Woodhead Publishing; 2015. p. 231–42.
Henry RR, Wiest-Kent TA, Scheaffer L, Kolterman OG, Olefsky JM. Metabolic consequences of very-low-calorie diet therapy in obese non-insulin-dependent diabetic and nondiabetic subjects. Diabetes. 1986;35:155–64.
Lewis MC, Phillips ML, Slavotinek JP, Kow L, Thompson CH, Toouli J. Change in liver size and fat content after treatment with Optifast very low calorie diet. Obese Surg. 2006;16:697–701.
Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70:741–56.
Beck AT, Ward CM, Mendelson M, Mock JE, Erbaugh JK. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71.
Spielberger CD, Gorsuch RL. Manual for the state-trait anxiety inventory. Palo Alto: Consulting Psychologists Press; 1983.
Carey M, Small H, Yoong SL, Boyes A, Bisquera A, Sanson-Fisher R. Prevalence of comorbid depression and obesity in general practice: a cross-sectional survey. Br J General Pract. 2014;64:e122–e127.
Grundy A, Cotterchio M, Kirsh VA, Kreiger N. Associations between anxiety, depression, antidepressant medication, obesity and weight gain among Canadian women. PLoS ONE. 2014;9:e99780.
Pan A, Sun Q, Czernichow S, Kivimaki M, Okereke OI, Lucas M, et al. Bidirectional association between depression and obesity in middle-aged and older women. Int J Obes. 2012;36:595–602.
Wadden TA, Stunkard AJ. Social and psychological consequences of obesity. Ann Intern Med. 1985;103:1062–7.
Stunkard AJ, Wadden TA. Psychological aspects of severe obesity. Am J Clin Nutr. 1992;55:524S–532S.
Sysko R, Devlin MJ, Hildebrandt TB, Brewer SK, Zitsman JL, Walsh T. Psychological outcomes and predictors of initial weight loss outcomes among severely obese adolescents receiving laparoscopic adjustable gastric banding. J Clin Psychiatry. 2012;73:1351.
Ukkola A, Maki M, Kurppa K, Pekka C, Huhtala H, Kekkonen L, et al. Diet improves perception of health and well-being in symptomatic, but not asymptomatic, patients with celiac disease. Clin Gastroenterol Hepatol. 2011;9:118–23.
Lasikiewicz N, Myrissa K, Hoyland A, Lawton CL. Psychological benefits of weight loss following behavioural and/or dietary weight loss interventions. A systematic research review. Appetite. 2014;72:123–37.
*Wadden TA, Foster GD, Letizia KA. One-year behavioral treatment of obesity: comparison of moderate and severe caloric restriction and the effects of weight maintenance therapy. J Consult Clin Psychol. 1994;62:165–71.
*de Zwaan M, Mitchell JE, Crosby RD, Mussell MP, Raymond NC, Specker SM, et al. Short-term cognitive behavioral treatment does not improve outcome of a comprehensive very-low-calorie diet program in obese women with binge eating disorder. Behav Ther. 2005;36:89–99.
*Snel M, Sleddering MA, Peijl ID, Romijn JA, Pijl H, Meinders E, et al. Quality of life in type 2 diabetes mellitus after a very low calorie diet and exercise. Eur J Intern Med. 2012;23:143–9.
*Cheskin LJ, Hess JM, Henningfield J, Gorelick DA. Calorie restriction increases cigarette use in adult smokers. Psychopharmacol (Berl). 2005;179:430–6.
*Buffenstein R, Karklin A, Driver HS. Beneficial physiological and performance responses to a month of restricted energy intake in healthy overweight women. Physiol Behav. 2000;68:439–44.
Kitto GC. Predicting attrition and adherence in a very low calorie diet behaviorally based treatment program for obesity. PhD [dissertation]. Kansas: Kansas State University; 1992. Available from: ProQuest Dissertations Publishing.
*Wadden TA, Stunkard AJ. Controlled trial of very low calorie diet, behavior therapy, and their combination in the treatment of obesity. J Consult Clin Psychol. 1986;54:482–8.
Swencionis C, Wylie-Rosett J, Lent MR, Ginsberg M, Cimino C, Wassertheil-Smoller S, et al. Weight change, psychological well-being, and vitality in adults participating in a cognitive-behavioral weight loss program. Health Psychol. 2013;32:439–46.
Wadden TA, Foster GD, Wang J, Pierson RN, Yang MU, Moreland K, et al. Clinical correlates of short-and long-term weight loss. Am J Clin Nutr. 1992;56:271S–274S.
Atkinson RL, Fuchs A, Pastors JG, Saunders JT. Combination of very-low-calorie diet and behavior modification in the treatment of obesity. Am J Clin Nutr. 1992;56:199S–202S.
Wise TN, Mann LS, Cooper JN, Rustigi EB. Patient characteristics and treatment results in a protein-modified fasting diet. Int J Eat Disord. 1986;5:1089–94.
Palmeira AL, Branco TL, Martins SC, Minderico CS, Silva MN, Vieira PN, et al. Change in body image and psychological well-being during behavioral obesity treatment: Associations with weight loss and maintenance. Body Image. 2010;7:187–93.
National Institute of Diabetes and Digestive and Kidney Disease. Very low-calorie diets [internet]. National Institute of Diabetes and Digestive and Kidney Disease; 2012 Dec [cited 2018 May 21]. http://www.niddk.nih.gov/health-information/health-topics/weight-control/very-low-calorie-diets/Documents/verylowcaldietsbw.pdf
Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011;41:15–28.
Williamson DF, Serdula MK, Anda RF, Levy A, Byers T. Weight loss attempts in adults: goals, duration, and rate of weight loss. Am J Public Health. 1992;82:1251–7.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Comprehensive meta-analysis: a computer program from research synthesis (version 3). Englewood: Biostat Inc; 2014.
Fabricatore AN, Wadden TA, Higginbotham AJ, Faulconbridge LF, Nguyen AM, Heymfield SB, et al. Intentional weight loss and changes in symptoms of depression: A systematic review and meta-analysis. Int J Obes. 2011;35:1363–76.
Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: Realist synthesis. BioMed Cent Med. 2013;11:1–14.
Liu JJW, Ein N, Vickers K. Subjective and physiological responses to the 35% carbon dioxide challenge in healthy and non-clinical control populations: A meta-analysis and systematic review. 2018.
*LaPorte DL. A fatiguing effect in obese patients during partial fasting: Increase in vulnerability to emotion-related events and anxiety. Int J Eat Disord. 1990;9:345–55.
Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100:316–36.
Clark LA, Watson D. Theoretical and empirical issues in differentiating depression from anxiety. In: Becker J, Kleinman A, editors. Psychosocial aspects of depression. Hillsdale: Lawrence Erlbaum Associates, Inc; 1990. p. 39–65.
Starr LR, Davila J. Cognitive and interpersonal moderators of daily co-occurrence of anxious and depressed moods in generalized anxiety disorder. Cogn Ther Res. 2012;36:655–69.
Levin-Aspenson HF, Watson D. Mode of administration effects in psychopathology assessment: analyses of gender, age, and education differences in self-rated versus interview-based depression. Psychol Assess. 2018;30:287–95.
Beck AT, Steer RA, Brown GK. BDI-II: Beck Depression Inventory Manual, 2nd edn. San Antonio: Psychological Corporation; 1996.
Wang YP, Gorenstein C. Assessment of depression in medical patients: a systematic review of the utility of the Beck Depression Inventory-II. Clinics. 2013;68:1274–87.
Health Canada. Estimated energy requirements [internet]. Health Canada; 2014 [cited 2018 May 21]. http://www.hc-sc.gc.ca/fn-an/food-guide-aliment/basics-base/1_1_1-eng.php
U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans 2015–2020, 8th edition [internet]. U.S. Department of Health and Human Services and U.S. Department of Agriculture; 2015 Dec [cited 2018 May 21]. http://health.gov/dietaryguidelines/2015/guidelines/.
Stice E, Fairburn CG. Dietary and dietary-depressive subtypes of bulimia nervosa show differential symptom presentation, social impairment, comorbidity, and course of illness. J Consult Clin Psychol. 2003;71:1090–4.
National Institute for Clinical Excellence. Obesity: identification, assessment and management of overweight and obesity in children, young people and adults: Partial update of CG43. London: National Institute for Health and Care Excellence; 2014.
*Foster GD, Wadden TA, Peterson FJ, Letizia KA, Bartlett SJ, Conill AM. A controlled comparison of three very-low-calorie diets: effects on weight, body composition, and symptoms. Am J Clin Nutr. 1992;55:811–7.
*Wadden TA, Stunkard AL, Brownell KD, Day SC. A comparison of two very-low-calorie diets: protein-sparing-modified fast versus protein-formula-liquid diet. Am J Clin Nutr. 1985;41:533–9.
*Wadden TA, Stunkard AJ, Brownell KD, Day SC. Treatment of obesity by behavior therapy and very low calorie diet: a pilot investigation. J Consult Clin Psychol. 1984;52:692–4.
Sandoz Nutrition. The OPTIFAST CORE Program Group Leader Guide, vol I and II. Minneapolis: Sandoz Nutrition, 1987.
Sandoz Nutrition. The OPTIFAST CORE program patient manual. Minneapolis: Sandoz Nutrition, 1987
Brownell, KD. The LEARN program for weight control. American Health Publishing Co: Dallas; 1989.
Stunkard AJ, Berthold HC. What is behavior therapy? Am J Clin Nutr. 1985;41:821–3.
Lindner PG, Blackburn GL. Multidisciplinary approach to obesity utilizing fasting modified by protein-sparing therapy. Obes/Bariatr Med. 1976;5:198–216.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Ein, N., Armstrong, B. & Vickers, K. The effect of a very low calorie diet on subjective depressive symptoms and anxiety: meta-analysis and systematic review. Int J Obes 43, 1444–1455 (2019). https://doi.org/10.1038/s41366-018-0245-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0245-4
This article is cited by
-
Effect of exercise as adjuvant to energy-restricted diets on quality of life and depression outcomes: a meta-analysis of randomized controlled trials
Quality of Life Research (2022)
-
Role of dietary factors in the prevention and treatment for depression: an umbrella review of meta-analyses of prospective studies
Translational Psychiatry (2021)