Abstract
Background/Objectives
Individuals born small-for-gestational age (SGA), especially those who experience postnatal catch-up growth, are at increased risk for developing endocrine-metabolic abnormalities before puberty. In adults, brown adipose tissue (BAT) has been associated with protection against metabolic disorders, such as obesity, type 2 diabetes, and dyslipidaemia. Here, we assessed for the first time whether BAT activation differs between prepubertal children born SGA or appropriate-for-gestational age (AGA).
Subjects/methods
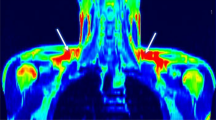
The study population consisted of 86 prepubertal children [41 AGA and 45 SGA; age (mean ± SEM), 8.5 ± 0.1 years], recruited into two prospective longitudinal studies assessing endocrine-metabolic status and body composition in infancy and childhood. The temperature at the supraclavicular region (SCR) before and after a cold stimulus was measured by infrared thermal imaging, and the area of thermally active SCR (increase after cold challenge, ΔAreaSCR) was calculated as a surrogate index of BAT activation. The results were correlated with clinical, endocrine-metabolic, and inflammation variables, and with visceral and hepatic adiposity (assessed by Magnetic Resonance Imaging).
Results
No differences in BAT activation index, as judged by ΔAreaSCR, were found between AGA and SGA children. However, girls showed higher baseline and post-cold induction AreaSCR than boys (both p ≤ 0.01). An interaction between gender and birth weight subgroup was observed for BAT activation; AGA girls increased significantly the ΔAreaSCR as compared to AGA boys; this increase did not occur in SGA girls vs SGA boys. Cold-induced ΔAreaSCR negatively correlated with HOMA-IR, us-CRP, liver volume, and liver fat.
Conclusions
Prepubertal AGA girls had significantly greater BAT activation index as compared to AGA boys; this difference was not observed in SGA subjects. Higher BAT activation associated with a lower amount of visceral fat and with a favorable metabolic profile. Long-term follow-up is needed to determine whether those differences relate to pubertal timing, and to the development of obesity and metabolic disorders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced foetal growth. Diabetologia. 1993;36:62–67.
Ibáñez L, Ong K, Dunger D, de Zegher F. Early development of adiposity and insulin resistance after catch-up weight gain in small-for-gestational age children. J Clin Endocrinol Metab. 2006;91:2153–8.
Ibáñez L, Suárez L, Lopez-Bermejo A, Díaz M, Valls C, de Zegher F. Early development of visceral fat excess after spontaneous catch-up growth in children with low birth weight. J Clin Endocrinol Metab. 2008;93:2079–83.
Sebastiani G, Díaz M, Bassols J, Aragonés G, López-Bermejo A, de Zegher F, et al. The sequence of prenatal growth restraint and post-natal catch-up growth leads to a thicker intima-media and more pre-peritoneal and hepatic fat by age 3-6 years. Pediatr Obes. 2016;11:251–7.
Ibáñez L, López-Bermejo A, Díaz M, Marcos MV, Casano P, de Zegher F. Abdominal fat partitioning and high-molecular-weight adiponectin in short children born small for gestational age. J Clin Endocrinol Metab. 2009;94:1049–52.
Malpique R, Bassols J, López-Bermejo A, Diaz M, Villarroya F, Pavia J, et al. Liver volume and hepatic adiposity in childhood: relations to body growth and visceral fat. Int J Obes (Lond). 2018;42:65–71.
Cypess AM, Lehman S, Williams G, Rodman D, Goldfine AB, Kuo FC, et al. Identification and importance of brown adipose tissue in adult humans. N Engl J Med. 2009;360:1509–17.
Rothwell NJ, Stock MJ. Effects of age on diet induced thermogenesis and brown adipose tissue metabolism in the rat. Int J Obes. 1983;7:583–9.
Chondronikola M, Volpi E, Børsheim E, Porter C, Annamalai P, Enerbäck S, et al. Brown adipose tissue improves whole-body glucose homeostasis and insulin sensitivity in humans. Diabetes. 2014;63:4089–99.
Bartelt A, Bruns OT, Reimer R, Hohenberg H, Ittrich H, Peldschus K, et al. Brown adipose tissue activity controls triglyceride clearance. Nat Med. 2011;17:200–5.
Enerback S. Human adipose tissue. Cell Metab. 2010;11:248–52.
Virtanen KA, Lidell ME, Orava J, Heglind M, Westergren R, Niemi T, et al. Functional brown adipose tissue in healthy adults. N Engl J Med. 2009;360:1518–25.
Drubach LA, Palmer EL 3rd, Connolly LP, Baker A, Zurakowski D, et al. Pediatric brown adipose tissue: detection, epidemiology, and differences from adults. J Pediatr. 2011;159:939–44.
Green AL, Bagci U, Hussein S, Kelly PV, Muzaffar R, Neuschwander-Tetri BA, et al. Brown adipose tissue detected by PET/CT imaging is associated with less central obesity. Nucl Med Commun. 2017;38:629–35.
Wijers SL, Saris WH, van Marken Lichtenbelt WD. Cold-induced adaptive thermogenesis in lean and obese. Obes (Silver Spring). 2010;18:1092–9.
Vijgen GH, Bouvy ND, Teule GJ, Brans B, Schrauwen P, van Marken Lichtenbelt WD. Brown adipose tissue in morbidly obese subjects. PLoS ONE. 2011;6:e17247.
Gilsanz V, Smith ML, Goodarzian F, Kim M, Wren TAL, Hu HH. Changes in brown adipose tissue in boys and girls during childhood and puberty. J Pediatr. 2012;169:604–9.
Robinson L, Ojha S, Symonds ME, Budge H. Body mass index as a determinant of brown adipose tissue function in healthy children. J Pediatr. 2014;164:318–22.
Symonds ME, Henderson K, Elvidge L, Bosman C, Sharkey, Perkins AC, et al. Thermal imaging to assess age-related changes of skin-temperature within supraclavicular region co-locating with brown adipose tissue in healthy children. J Pediatr. 2012;161:892–8.
Law JM, Morris DE, Engbeaya CI, Salem V, Coello C, Robinson L, et al. Thermal imaging is a non-invasive alternative to PET-CT for measurement of brown adipose tissue activity in humans. J Nucl Med. 2018;59:516–22.
Ong KK, Ahmed ML, Emmett PM, Preece MA, Dunger DB. Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ. 2000;320:967–71.
Jang C, Jalapu S, Thuzar M, Law PW, Susanne Jeavons S, Barclay JL, et al. Infrared thermography in the detection of brown adipose tissue in humans. Physiol Rep. 2014;2:e12167.
Ferrández-Longas A, Mayayo E, Labarta JI, Bagué L, Puga B, Rueda C, et al. Estudio longitudinal de crecimiento y desarrollo. Centro Andrea Prader. Zaragoza 1980-2002. In: Garcia- Dihinx A, Romo A, Ferrandez-Longas A (eds). Patrones de crecimiento y desarrollo en España. Ergon: Madrid, Spain; 2004. pp. 61–115.
Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51:170–9.
Ibáñez L, Lopez-Bermejo A, Díaz M, Suárez L, de Zegher F. Low-birth weight children develop lower sex hormone binding globulin and higher dehydroepiandrosterone sulfate levels and aggravate their visceral adiposity and hypoadiponectinemia between six and eight years of age. J Clin Endocrinol Metab.2009;94:3696–3699.
Gilsanz V, Chung SA, Jackson H, Dorey FJ, Hu HH. Functional brown adipose tissue is related to muscle volume in children and adolescents. J Pediatr. 2011;158:722–6.
Ponrartana S, Patricia C, Aggabao PC, Chavez TA, Dharmavaram NL, Gilsanz V. Changes in brown adipose tissue and muscle development during infancy. J Pediatr. 2016;173:116–21.
Saito M, Okamatsu-Ogura Y, Matsushita M, Watanabe K, Yoneshiro T, Nio-Kobayashi J, et al. High incidence of metabolically active brown adipose tissue in healthy adult humans: effects of cold exposure and adiposity. Diabetes. 2009;58:1526–31.
Cohade C, Osman M, Pannu HK, Wahl RL. Uptake in supraclavicular area fat (“USA-Fat”): description on 18F-FDG PET/CT. J Nucl Med. 2003;44:170–6.
Pfannenberg C, Werner MK, Ripkens S, Stef I, Deckert A, Schmadl M. Impact of age on the relationships of brown adipose tissue with sex and adiposity in humans. Diabetes. 2010;59:1789–93.
Claussnitzer M, Dankel SN, Kim KH, Quon G, Meuleman W, Haugen C, et al. FTO obesity variant circuitry and adipocyte browning in humans. N Engl J Med. 2015;373:895–907.
Dumortier O, Roger E, Pisani DF, Casamento V, Gautier N, Lebrun P, et al. Age-dependent control of energy homeostasis by brown adipose tissue in progeny subjected to maternal diet-induced fetal programming. Diabetes. 2017;66:627–39.
Bartelt A, Bruns OT, Reimer R, Hohenberg H, Ittrich H, Peldschus K. Brown adipose tissue activity controls triglyceride clearance. Nat Med. 2011;17:200–5.
Lee P, Bova R, Schofield L, Bryant W, Dieckmann W, Slattery A, et al. Brown adipose tissue exhibits a glucose-responsive thermogenic biorhythm in humans. Cell Metab. 2016;23:602–9.
Villarroya F, Gavaldà-Navarro A, Peyrou M, Villarroya J, Giralt M. The lives and times of brown adipokines. Trends Endocrinol Metab. 2017;28:855–67.
Wang GX, Zhao XY, Meng ZX, Kern M, Dietrich A, Chen Z, et al. The brown fat–enriched secreted factor Nrg4 preserves metabolic homeostasis through attenuation of hepatic lipogenesis. Nat Med. 2014;20:1436–43.
Ibáñez L, Ong KK, López-Bermejo A, Dunger DB, de Zegher F. Hyperinsulinaemic androgen excess in adolescent girls. Nat Rev Endocrinol. 2014;10:499–508.
de Zegher F, Reinehr T, Malpique R, Darendeliler F, López-Bermejo A, Ibáñez L. Reduced prenatal weight gain and/or augmented postnatal weight gain precedes polycystic ovary syndrome in adolescent girls. Obes (Silver Spring). 2017;25:1486–9.
Yuan X, Hu T, Zhao H, Huang Y, Ye R, Lin J, et al. Brown adipose tissue transplantation ameliorates polycystic ovary syndrome. Proc Natl Acad Sci USA. 2016;113:2708–13.
Hu T, Yuan X, Ye R, Zhou H, Lin J, Zhang C, et al. Brown adipose tissue activation by rutin ameliorates polycystic ovary syndrome in rat. J Nutr Biochem. 2017;47:21–28.
Ibáñez L, López-Bermejo A, Díaz M, de Zegher F. Catch-up growth in girls born small for gestational age precedes childhood progression to high adiposity. Fertil Steril. 2011;96:220–3.
Persson I, Ahlsson F, Ewald U, Tuvemo T, Qingyuan M, von Rosen D, et al. Influence of perinatal factors on the onset of puberty in boys and girls: implications for interpretation of link with risk of long term diseases. Am J Epidemiol. 1999;150:747–55.
Solorzano CMB, McCartney CR. Obesity and the pubertal transition in girls and boys. Reproduction. 2010;140:399–410.
Day FR, Elks CE, Murray A, Ong KK, Perry JRB. Puberty timing associated with diabetes, cardiovascular disease and also diverse health outcomes in men and women: the UK Biobank study. Sci Rep. 2015;5:11208.
Trnovská J, Šilhavý J, Kuda O, Landa V, Zídek V, Mlejnek P, et al. Salsalate ameliorates metabolic disturbances by reducing inflammation in spontaneously hypertensive rats expressing human C-reactive protein and by activating brown adipose tissue in nontransgenic controls. PLoS ONE. 2017;12:e0179063.
Lee J, Yoon K, Ryu S, Chang Y, Kim HR. High-normal levels of hs-CRP predict the development of non-alcoholic fatty liver in healthy men. PLoS ONE. 2017;12:e0172666.
Bian H, Hakkarainen A, Zhou Y, Lundbom N, Olkkonen VM, Yki-Järvinen H. Impact of non-alcoholic fatty liver disease on liver volume in humans. Hepatol Res. 2015;45:210–9.
Van der Poorten D, Milner KL, Hui J, Hodge A, Trenell MI, Kench JG, et al. Visceral fat: a key mediator of steatohepatitis in metabolic liver disease. Hepatology. 2008;48:449–57.
Ouellet V, Routhier-Labadie A, Bellemare W, Lakhal-Chaieb L, Turcotte E, Carpentier AC, et al. Outdoor temperature, age, sex, body mass index, and diabetic status determine the prevalence, mass, and glucose-uptake activity of 18F-FDG-detected BAT in humans. J Clin Endocrinol Metab. 2011;96:192–9.
Matsushita M, Yoneshiro T, Aita S, Kameya T, Sugie H, Saito M. Impact of brown adipose tissue on body fatness and glucose metabolism in healthy humans. Int J Obes (Lond). 2014;38:812–7.
Robinson LJ, Law JM, Symonds ME, Budge H. Brown adipose tissue activation as measured by infrared thermography by mild anticipatory psychological stress in lean healthy females. Exp Physiol. 2016;101:549–57.
Scotney H, Symonds ME, Law J, Budge H, Sharkey D, Manolopoulos KN. Glucocorticoids modulate human brown adipose tissue thermogenesis in vivo. Metabolism. 2017;70:125–32.
Acknowledgements
RM, GS, and LI are investigators of CIBERDEM (www.ciberdem.org). ALB is an investigator of the I3 Fund for Scientific research (Ministry of Education and Science, Spain). LI and RM had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. This study was supported by the Ministerio de Ciencia e Innovación, Instituto de Salud Carlos III, and by the Fondo Europeo de Desarrollo Regional (FEDER) (PI11/02403).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Malpique, R., Gallego-Escuredo, J.M., Sebastiani, G. et al. Brown adipose tissue in prepubertal children: associations with sex, birthweight, and metabolic profile. Int J Obes 43, 384–391 (2019). https://doi.org/10.1038/s41366-018-0198-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0198-7
This article is cited by
-
The relationship between famine exposure during early life and carotid plaque in adulthood
European Journal of Clinical Nutrition (2021)
-
Developmental Programming of Body Composition: Update on Evidence and Mechanisms
Current Diabetes Reports (2019)