Abstract
Background/Objectives
Physical activity (PA) and cardiorespiratory fitness (CRF) are independently associated with reduced cardiometabolic risk in children, and may affect risk through different pathways. This study aims to examine if CRF moderate the prospective association between PA, sedentary time, and cardiometabolic outcomes in 10-year-old children.
Subjects/Methods
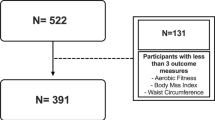
In total, 718 children of 1129 (drop out n = 7) had valid measures of PA (accelerometry), CRF (the Andersen running test), and a cardiometabolic risk profile measured at baseline and follow-up 7 months later. Cardiometabolic outcomes were systolic blood pressure, waist circumference (WC), total cholesterol, high-density lipoprotein, triglycerides, glucose, and insulin (HOMA-IR). The cardiometabolic risk factors were analysed individually, and as a clustered risk score (z score). A linear mixed model was used to examine the prospective associations between different PA exposures (overall PA, sedentary time, moderate-to-vigorous PA (MVPA), vigorous PA) and cardiometabolic outcomes, including the interaction term PA × CRF in the model to assess moderation by CRF.
Results
CRF modified the association for baseline overall PA (P < 0.039) and MVPA (min/day) with clustered cardiometabolic risk at follow-up (P < 0.023). Moreover, CRF modified the association between overall PA and MVPA with HOMA-IR independent of WC (P < 0.022). When stratified by CRF level (median split; high/low), MVPA predicted lower HOMA-IR [MVPA β −0.133 (95% CI: −0.223, −0.043); P = 0.004] and clustered cardiometabolic risk [MVPA β −0.094 (95% CI: −0.169, −0.019); P = 0.014] in children with low CRF, but not among their fitter peers (P > 0.232). There was neither direct association between sedentary time and cardiometabolic risk factors in any analyses, nor moderation by CRF.
Conclusion
CRF significantly moderated the prospective association between PA and the clustered cardiometabolic risk, but not for time spent sedentary. The magnitude of association between MVPA and clustered cardiometabolic risk was stronger in children with low CRF, and no associations appeared present in their high-fit peers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Berenson GS, Srinivasan SR, Nicklas TA. Atherosclerosis: a nutritional disease of childhood. Am J Cardiol. 1998;82:22T–9T.
Raitakari OT, Juonala M, Kahonen M, Taittonen L, Laitinen T, Maki-Torkko N, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–83.
Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, et al. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study). Lancet. 2006;368:299–304.
Brage S, Wedderkopp N, Ekelund U, Franks PW, Wareham NJ, Andersen LB, et al. Features of the metabolic syndrome are associated with objectively measured physical activity and fitness in Danish children: the European Youth Heart Study (EYHS). Diabetes Care. 2004;27:2141–8.
Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A, et al. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307:704–12.
Skrede T, Stavnsbo M, Aadland E, Aadland KN, Anderssen SA, Resaland GK, et al. Moderate-to-vigorous physical activity, but not sedentary time, predicts changes in cardiometabolic risk factors in 10-y-old children: the Active Smarter Kids Study. Am J Clin Nutr. 2017;105:1391–8.
Anderssen SA, Cooper AR, Riddoch C, Sardinha LB, Harro M, Brage S, et al. Low cardiorespiratory fitness is a strong predictor for clustering of cardiovascular disease risk factors in children independent of country, age and sex. Eur J Cardiovasc Prev Rehabil. 2007;14:526–31.
Ruiz JR, Ortega FB, Rizzo NS, Villa I, Hurtig-Wennlof A, Oja L, et al. High cardiovascular fitness is associated with low metabolic risk score in children: the European Youth Heart Study. Pediatr Res. 2007;61:350–5.
Ekelund U, Anderssen SA, Froberg K, Sardinha LB, Andersen LB, Brage S, et al. Independent associations of physical activity and cardiorespiratory fitness with metabolic risk factors in children: the European youth heart study. Diabetologia. 2007;50:1832–40.
Schutte NM, Nederend I, Hudziak JJ, Bartels M, de Geus EJ. Twin-sibling study and meta-analysis on the heritability of maximal oxygen consumption. Physiol Genom. 2016;48:210–9.
Ortega FB, Ruiz JR, Hurtig-Wennlof A, Vicente-Rodriguez G, Rizzo NS, Castillo MJ, et al. Cardiovascular fitness modifies the associations between physical activity and abdominal adiposity in children and adolescents: the European Youth Heart Study. Br J Sports Med. 2010;44:256–62.
Resaland GK, Moe VF, Aadland E, Steene-Johannessen J, Glosvik O, Andersen JR, et al. Active Smarter Kids (ASK): Rationale and design of a cluster-randomized controlled trial investigating the effects of daily physical activity on children’s academic performance and risk factors for non-communicable diseases. BMC Public Health. 2015;15:709.
Resaland GK, Aadland E, Moe VF, Aadland KN, Skrede T, Stavnsbo M, et al. Effects of physical activity on schoolchildren’s academic performance: the Active Smarter Kids (ASK) cluster-randomized controlled trial. Prev Med. 2016;91:322–8.
Andersen LB, Andersen TE, Andersen E, Anderssen SA. An intermittent running test to estimate maximal oxygen uptake: the Andersen test. J Sports Med Phys Fit. 2008;48:434–7.
Aadland E, Terum T, Mamen A, Andersen LB, Resaland GK. The Andersen aerobic fitness test: reliability and validity in 10-year-old children. PLoS ONE. 2014;9:e110492.
Esliger DW, Copeland JL, Barnes JD, Tremblay MS. Standardizing and optimizing the use of accelerometer data for free-living physical activity monitoring. J Phys Activity Health. 2005;2:366-83.
Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37:S531–43.
Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26:1557–65.
Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43:1360–8.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ . 2000;320:1240–3.
Tanner JM. Growth at Adolescence: with a general consideration of the effects of heredity and environmental factors upon growth and maturation from birth to maturity. 2nd edition ed. Oxford: Blackwell Scientific Publications; 1962.
Carel JC, Leger J. Clinical practice. Precocious puberty. N Engl J Med. 2008;358:2366–77.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370:1829–39.
Rickham PP. Human Experimentation. Code of Ethics of the World Medical Association. Declaration of Helsinki. Br Med J. 1964;2:177.
Aadland E, Andersen LB, Lerum O, Resaland GK. The Andersen aerobic fitness test: new peak oxygen consumption prediction equations in 10 and 16-year olds. Scand J Med Sci Sports. 2017.;28:862-72
Cesa CC, Sbruzzi G, Ribeiro RA, Barbiero SM, de Oliveira Petkowicz R, Eibel B, et al. Physical activity and cardiovascular risk factors in children: meta-analysis of randomized clinical trials. Prev Med. 2014;69:54–62.
Ferguson MA, Gutin B, Le NA, Karp W, Litaker M, Humphries M, et al. Effects of exercise training and its cessation on components of the insulin resistance syndrome in obese children. Int J Obes Relat Metab Disord. 1999;23:889–95.
Meyer U, Schindler C, Zahner L, Ernst D, Hebestreit H, van Mechelen W, et al. Long-term effect of a school-based physical activity program (KISS) on fitness and adiposity in children: a cluster-randomized controlled trial. PLoS ONE. 2014;9:e87929.
Tarp J, Brønd JC, Andersen LB, Møller NC, Froberg K, Grøntved A. Physical activity, sedentary behavior and long-term cardiovascular risk in young people: a review and discussion of methodology in prospective studies. J Sport Health Sci. 2016.;5:145-50
van Ekris E, Altenburg TM, Singh AS, Proper KI, Heymans MW, Chinapaw MJ. An evidence-update on the prospective relationship between childhood sedentary behaviour and biomedical health indicators: a systematic review and meta-analysis. Obes Rev. 2016;17:833–49.
Cliff DP, Hesketh KD, Vella SA, Hinkley T, Tsiros MD, Ridgers ND, et al. Objectively measured sedentary behaviour and health and development in children and adolescents: systematic review and meta-analysis. Obes Rev. 2016;17:330–44.
Chinapaw MJ, Altenburg T, Brug J. Sedentary behaviour and health in children - evaluating the evidence. Prev Med. 2015;70:1–2.
Berman LJ, Weigensberg MJ, Spruijt-Metz D. Physical activity is related to insulin sensitivity in children and adolescents, independent of adiposity: a review of the literature. Diabetes Metab Res Rev. 2012;28:395–408.
Bird SR, Hawley JA. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc Med. 2016;2:e000143.
DeFronzo RA, Ferrannini E, Sato Y, Felig P, Wahren J. Synergistic interaction between exercise and insulin on peripheral glucose uptake. J Clin Invest. 1981;68:1468–74.
Goodyear LJ, Kahn BB. Exercise, glucose transport, and insulin sensitivity. Annu Rev Med. 1998;49:235–61.
Richter EA, Hargreaves M. Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol Rev. 2013;93:993–1017.
Kraniou GN, Cameron-Smith D, Hargreaves M. Acute exercise and GLUT4 expression in human skeletal muscle: influence of exercise intensity. J Appl Physiol. 2006;101:934–7.
Lawlor DA, Benfield L, Logue J, Tilling K, Howe LD, Fraser A, et al. Association between general and central adiposity in childhood, and change in these, with cardiovascular risk factors in adolescence: prospective cohort study. BMJ . 2010;341:c6224.
Bouchard C, Rankinen T. Individual differences in response to regular physical activity. Med Sci Sports Exerc. 2001;33:S446–51. discussionS52-3
Kriemler S, Zahner L, Schindler C, Meyer U, Hartmann T, Hebestreit H, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ. 2010;340:c785.
Resaland GK, Anderssen SA, Holme IM, Mamen A, Andersen LB. Effects of a 2-year school-based daily physical activity intervention on cardiovascular disease risk factors: the Sogndal school-intervention study. Scand J Med Sci Sports. 2011;21:e122–31.
Aadland E, Andersen LB, Skrede T, Ekelund U, Anderssen SA, Resaland GK. Reproducibility of objectively measured physical activity and sedentary time over two seasons in children; comparing a day-by-day and a week-by-week approach. PLoS ONE. 2017;12:e0189304.
Mattocks C, Leary S, Ness A, Deere K, Saunders J, Kirkby J, et al. Intraindividual variation of objectively measured physical activity in children. Med Sci Sports Exerc. 2007;39:622–9.
Hutcheon JA, Chiolero A, Hanley JA. Random measurement error and regression dilution bias. BMJ . 2010;340:c2289.
Aadland E, Kvalheim OM, Rajalahti T, Skrede T, Resaland GK. Aerobic fitness and metabolic health in children: A clinical validation of directly measured maximal oxygen consumption versus performance measures as markers of health. Prev Med Rep. 2017;7:74–6.
Carter PJ, Taylor BJ, Williams SM, Taylor RW. Longitudinal analysis of sleep in relation to BMI and body fat in children: the FLAME study. BMJ . 2011;342:d2712.
Perneger TV. What’s wrong with Bonferroni adjustments. BMJ . 1998;316:1236–8.
Acknowledgements
The authors are grateful to the children and their parents/guardians from the 57 participating elementary schools for their time and effort. We would also like to acknowledge all colleagues and students who participated in data collection.
Funding:
The study was supported by grants from the Research Council of Norway (grant number 221047/F40 and 249932/F20), the Gjensidige Foundation (grant number 1042294), and the Western Norway University of Applied Sciences (formerly credited as the Sogn og Fjordane University College).
Authors Contribution
The authors’ responsibilities were as follows—G.K.R., S.A.A., L.B.A., E.Aa., and U.E. designed the Active Smarter Kids Study. T.S., E.Aa., M.S., S.A.A., and G.K.R. conducted the research. T.S., E.Aa., and U.E. analysed the data. T.S., E.Aa., G.K.R., and U.E. wrote the manuscript. T.S., E.Aa., G.K.R., and U.E. had primary responsibility for the final content. All authors have read, provided feedback, and approved submission of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Skrede, T., Aadland, E., Andersen, L.B. et al. Does cardiorespiratory fitness moderate the prospective association between physical activity and cardiometabolic risk factors in children?. Int J Obes 42, 1029–1038 (2018). https://doi.org/10.1038/s41366-018-0108-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0108-z