Abstract
Background/objectives
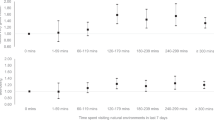
Examine the prospective relationship of total volume versus bouts of sedentary behaviour (SB) and moderate-to-vigorous physical activity (MVPA) with cardiometabolic risk in children. In addition, the moderating effects of weight status and MVPA were explored.
Subjects/methods
Longitudinal study including 454 primary school children (mean age 10.3 years). Total volume and bouts (i.e. ≥10 min consecutive minutes) of MVPA and SB were assessed by accelerometry in Nov 2009/Jan 2010 (T1) and Aug/Oct 2010 (T2). Triglycerides, total cholesterol/HDL cholesterol ratio (TC:HDLC ratio), homoeostatic model assessment of insulin resistance, systolic blood pressure and waist circumference were assessed at T2 (Sept/Oct 2010) and combined in a composite cardiometabolic risk score. Associations of total time and uninterrupted MVPA and SB were examined using multilevel mixed linear models, with or without mutual adjustments between MVPA and SB. The moderating effects of weight status and MVPA (for SB only) were examined by adding interaction terms.
Results
Children engaged daily in about 60 min of total MVPA and 0–15 min/week in MVPA bouts. Mean total sedentary time was around 7 h/day with over 3 h/day accumulated in bouts. Higher mean levels of MVPA were significantly associated with a lower waist circumference, triglycerides, insulin resistance, TC:HDLC ratio and composite cardiometabolic risk, with non-significant associations for uninterrupted MVPA. Associations with sedentary time were much smaller and inconsistent: higher total sedentary time was associated with higher insulin resistance; after adjusting for MVPA, higher mean total and bouts of sedentary time were associated with lower waist circumference, and sedentary bouts with lower composite cardiometabolic risk.
Conclusions
Children accumulated MVPA intermittently and rarely in bouts, and about half their total sedentary time in bouts. Total MVPA is important for lowering cardiometabolic risk in children, whereas both total and uninterrupted sedentary time seem of less importance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Steele RM, Brage S, Corder K, Wareham N, Ekelund U. Physical activity, cardiorespiratory fitness, and the metabolic syndrome in youth. J Appl Physiol. 2008;105:342–51.
Chinapaw M, Altenburg T, Brug J. Sedentary behaviour and health in children - evaluating the evidence. Prev Med. 2015;70:1–2.
Chinapaw MJ, Proper KI, Brug J, van Mechelen W, Singh AS. Relationship between young peoples’ sedentary behaviour and biomedical health indicators: a systematic review of prospective studies. Obes Rev. 2011;12:e621–32.
van Ekris E, Altenburg TM, Singh A, Proper K, Heymans MW, Chinapaw M. An evidence-update on the prospective relationship between childhood sedentary behaviour and biomedical health indicators: a systematic review and meta-analysis. Obes Rev. 2016;17:833–49.
Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307:704–12.
Brug J, van Stralen MM, Te Velde SJ, Chinapaw MJ, De Bourdeaudhuij I, Lien N, et al. Differences in weight status and energy-balance related behaviors among school children across Europe: the ENERGY-Project. PLoS ONE. 2012;7:e34742.
Verloigne M, Van Lippevelde W, Maes L, Yildirim M, Chinapaw M, Manios Y, et al. Self-reported TV and computer time do not represent accelerometer-derived total sedentary time in 10 to 12-year-olds. Eur J Public Health. 2013;23:30–2.
Tremblay MS, Barnes JD, Gonzalez SA, Katzmarzyk PT, Onywera VO, Reilly JJ. et al. GlobalMatrix 2.0: report card grades on the physical activity of children and youth comparing 38 countries. J Phys Act Health. 2016;13(11Suppl 2):S343–66.
Jago R, Baranowski T, Baranowski JC, Thompson D, Greaves KA. BMI from 3-6 y of age is predicted by TV viewing and physical activity, not diet. Int J Obes. 2005;29:557–64.
Basterfield L, Pearce MS, Adamson AJ, Frary JK, Parkinson KN, Wright CM, et al. Physical activity, sedentary behavior, and adiposity in English children. Am J Prev Med. 2012;42:445–51.
Altenburg TM, Rotteveel J, Dunstan DW, Salmon J, Chinapaw MJ. The effect of interrupting prolonged sitting time with short, hourly, moderate-intensity cycling bouts on cardiometabolic risk factors in healthy, young adults. J Appl Physiol. 2013;115:1751–6.
Healy G, Dunstan D, Salmon J, Cerin E, Shaw J, Zimmet P, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31:661–6.
Peddie MC, Bone JL, Rehrer NJ, Skeaff CM, Gray AR, Perry TL. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. Am J Clin Nutr. 2013;98:358–66.
Saunders TJ, Chaput JP, Goldfield GS, Colley RC, Kenny GP, Doucet E, et al. Prolonged sitting and markers of cardiometabolic disease risk in children and youth: a randomized crossover study. Metabolism. 2013;62:1423–8.
Belcher BR, Berrigan D, Papachristopoulou A, Brady SM, Bernstein SB, Brychta RJ, et al. Effects of interrupting children’s sedentary behaviors with activity on metabolic function: a randomized trial. J Clin Endocrinol Metab. 2015;100:3735–43.
Fletcher EA, Salmon J, McNaughton SA, Orellana L, Wadley GD, Bruce C, et al. Effects of breaking up sitting on adolescents’ postprandial glucose after consuming meals varying in energy: a cross-over randomised trial. J Sci Med Sport. 2017;21:280–5.
Carson V, Janssen I. Volume, patterns, and types of sedentary behavior and cardiometabolic health in children and adolescents: a cross-sectional study. BMC Public Health. 2011;11:274.
Carson V, Stone M, Faulkner G. Patterns of sedentary behavior and weight status among children. Pediatr Exerc Sci. 2014;26:95–102.
Altenburg TM, de Niet M, Verloigne M, De Bourdeaudhuij I, Androutsos O, Manios Y, et al. Occurrence and duration of various operational definitions of sedentary bouts and cross-sectional associations with cardiometabolic health indicators: the ENERGY-project. Prev Med. 2015;71:101–6.
Andersen LB, Wedderkopp N, Hansen HS, Cooper AR, Froberg K. Biological cardiovascular risk factors cluster in Danish children and adolescents: the European Youth Heart Study. Prev Med. 2003;37:363–7.
Andersen LB, Lauersen JB, Brond JC, Anderssen SA, Sardinha LB, Steene-Johannessen J, et al. A new approach to define and diagnose cardiometabolic disorder in children. J Diabetes Res. 2015;2015:539835.
Andersen LB, Haraldsdottir J. Tracking of cardiovascular disease risk factors including maximal oxygen uptake and physical activity from late teenage to adulthood. An 8-year follow-up study. J Intern Med. 1993;234:309–15.
Wirix AJ, Nauta J, Groothoff JW, Rabelink TJ, Hirasing RA, Chinapaw MJ, et al. Is the prevalence of hypertension in overweight children overestimated? Arch Dis Child. 2016;101:998–1003.
Reinehr T, Andler W, Denzer C, Siegried W, Mayer H, Wabitsch M. Cardiovascular risk factors in overweight German children and adolescents: relation to gender, age and degree of overweight. Nutr Metab Cardiovasc Dis. 2005;15:181–7.
Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012.
Wedderkopp N, Jespersen E, Franz C, Klakk H, Heidemann M, Christiansen C, et al. Study protocol. The Childhood Health, Activity, and Motor Performance School Study Denmark (The CHAMPS-study DK). BMC Pediatr. 2012;12:128.
Kinosian B, Glick H, Garland G. Cholesterol and coronary heart disease: predicting risks by levels and ratios. Ann Intern Med. 1994;121:641–7.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Chinapaw MJM, de Niet M, Verloigne M, de Bourdeauhuij I, Brug J, Altenburg TM. From sedentary time to sedentary patterns: accelerometer data reduction decision in youth. PLoS ONE. 2014;9:e111205.
Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43:1360–8.
Fischer C, Yildirim M, Salmon J, Chinapaw M. Comparing different accelerometer cut points for sedentary time in children. Pediatr Exerc Sci. 2012;24:220–8.
Altenburg TM, Chinapaw MJ. Bouts and breaks in children’s sedentary time: currently used operational definitions and recommendations for future research. Prev Med. 2015;77:1–3.
Hamilton MT, Hamilton DG, Zderic TW. Exercise physiology versus inactivity physiology: an essential concept for understanding lipoprotein lipase regulation. Exerc Sport Sci Rev. 2004;32:161–6.
Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26:1557–65.
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–93.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3.
Tanner JM. Growth at Adolescence. 2nd edn. Oxford: Blackwell Scientific; 1962.
Duke PM, Litt IF, Gross RT. Adolescents’ self-assessment of sexual maturation. Pediatrics. 1980;66:918–20.
Ragland DR. Dichotomizing continuous outcome variables: dependence of the magnitude of association and statistical power on the cutpoint. Epidemiology. 1992;3:434–40.
Ried-Larsen M, Grontved A, Moller NC, Larsen KT, Froberg K, Andersen LB. Associations between objectively measured physical activity intensity in childhood and measures of subclinical cardiovascular disease in adolescence: prospective observations from the European Youth Heart Study. Br J Sports Med. 2014;48:1502–7.
Jago R, Wedderkopp N, Kristensen PL, Moller NC, Andersen LB, Cooper AR, et al. Six-year change in youth physical activity and effect on fasting insulin and HOMA-IR. Am J Prev Med. 2008;35:554–60.
Hjorth MF, Chaput JP, Damsgaard CT, Dalskov SM, Andersen R, Astrup A, et al. Low physical activity level and short sleep duration are associated with an increased cardiometabolic risk profile: a longitudinal study in 8–11 year old Danish children. PLoS ONE. 2014;9:e104677.
Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:1302–10.
Andersen L, Hasselstrøm H, Grønfeldt V, Hansen S, Froberg K. The relationship between physical fitness and clustered risk, and tracking of clustered risk from adolescence to young adulthood: eight years follow-up in the Danish Youth and Sport Study. Int J Behav Nutr Phys Act. 2004;1:6.
Acknowledgements
The CHAMPS-study was funded by: The TRYG Foundation, University College Lillebaelt, University of Southern Denmark, The Nordea Foundation, The IMK foundation, The Region of Southern Denmark, The Egmont Foundation, The A.J. Andersen Foundation, The Danish Rheumatism Association, Østifternes Foundation, Brd. Hartmann’s Foundation, TEAM Denmark, The Danish Chiropractor Foundation, The Nordic Institute of Chiropractic and Clinical Biomechanics.
Author contributions
MC had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: MC and TA. Acquisition of data: HK, NCM. Drafting of the manuscript: MC and TA. Critical revision of the manuscript for important intellectual content: All authors. Statistical analyses: MC. Obtained funding: NW and LBA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The contributions of Altenburg and Chinapaw were funded by the Netherlands Organization for Health Research and Development (ZonMw; Project No. 91211057). The remaining authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chinapaw, M., Klakk, H., Møller, N.C. et al. Total volume versus bouts: prospective relationship of physical activity and sedentary time with cardiometabolic risk in children. Int J Obes 42, 1733–1742 (2018). https://doi.org/10.1038/s41366-018-0063-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0063-8
This article is cited by
-
Determination of cut-off points for the Move4 accelerometer in children aged 8–13 years
BMC Sports Science, Medicine and Rehabilitation (2023)
-
Sedentary patterns and cardiometabolic risk factors in Mexican children and adolescents: analysis of longitudinal data
International Journal of Behavioral Nutrition and Physical Activity (2022)
-
A collaborative approach to adopting/adapting guidelines. The Australian 24-hour movement guidelines for children (5-12 years) and young people (13-17 years): An integration of physical activity, sedentary behaviour, and sleep
International Journal of Behavioral Nutrition and Physical Activity (2022)
-
The multivariate physical activity signature associated with metabolic health in children
International Journal of Behavioral Nutrition and Physical Activity (2018)