Abstract
Introduction
Obesity is a major risk factor for mortality from a range of causes. We investigated whether skinfold measurements were associated with mortality independently of variation in body mass index (BMI).
Methods
A prospective analysis of mortality in 870 apparently healthy adult Caucasian men participating in an occupational health cohort was undertaken. At baseline, skinfold measurements were taken at biceps, triceps, iliac and subscapular sites. Derived measurements included the sum of all four skinfolds and subscapular to triceps, subscapular to iliac and BMI to iliac ratios. All-cause mortality was analysed by Cox proportional hazards modelling and death in specific mortality subcategories by competing risks analysis.
Results
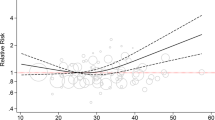
During a mean of 27.7 years follow up, there were 303 deaths (119 cancer, 101 arteriovascular, 40 infection, 43 other). In univariable analysis, BMI was associated with all-cause, cancer, arteriovascular and other mortality and subscapular skinfold with all-cause and arteriovascular mortality. On bivariable analysis, with inclusion of BMI, subscapular skinfold ceased to be a associated with mortality but iliac skinfold emerged as strongly, negatively associated with all-cause and arteriovascular mortality. In multivariable analysis, with inclusion of age, BMI, smoking, alcohol and exercise, iliac skinfold was negatively associated with all-cause (Hazard ratio HR 0.77, 95% confidence interval CI 0.66–0.90, p = 0.002), arteriovascular (HR 0.75, 95%CI 0.58,0.97, p = 0.02) and infection (HR 0.63, 95%CI 0.42,0.94, p = 0.02) death. Among obese participants (BMI ≥ 30 kg/m2), iliac skinfold of ≤9.7 mm was associated with a six-fold increase in all-cause mortality risk.
Conclusion
Low iliac skinfold thickness is an independent risk factor for all-cause mortality in adult white males with risk apparently concentrated among people who are obese.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156.
Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
He Y, Lam TH, Jiang B, Li LS, Sun DL, Wu L, et al. Changes in BMI before and during economic development and subsequent risk of cardiovascular disease and total mortality: a 35-year follow-up study in China. Diabetes Care. 2014;37:2540–7.
Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Prac. 2010;89:309–19.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–78.
Aune D, Norat T, Vatten LJ. Body mass index, abdominal fatness and the risk of gallbladder disease. Eur J Epidemiol. 2015;30:1009–19.
Aune D, Norat T, Vatten LJ. Body mass index and the risk of gout: a systematic review and dose-response meta-analysis of prospective studies. Eur J Nutr. 2014;53:1591–601.
Kip KE, Marroquin OC, Kelley DE, Johnson BD, Kelsey SF, Shaw LJ, et al. Clinical importance of obesity versus the metabolic syndrome in cardiovascular risk in women: a report from the Women’s Ischemia Syndrome Evaluation (WISE) study. Circulation. 2004;109:706–13.
Kaur A, Johnston DG, Godsland IF. Does metabolic health in overweight and obesity persist?—Individual variation and cardiovascular mortality over two decades. Eur J Endocrinol. 2016;175:133–43.
Bradshaw PT, Reynolds KR, Wagenknecht LE, Ndumele CE, Stevens J. Incidence of components of metabolic syndrome in the metabolically healthy obese over 9 years follow-up: the atherosclerosis risk in communities study. Int J Obes. 2017.
Espinosa De Ycaza AE, Donegan D, Jensen MD. Long-term metabolic risk for the metabolically healthy overweight/obese phenotype. Int J Obes. 2017.
Kramer CK, Zinman B, Retnakaran R. Are metabolically healthy overweight and obesity benign conditions?: A systematic review and meta-analysis. Ann Intern Med. 2013;159:758–69.
Lassale C, Tzoulaki I, Moons KGM, Sweeting M, Boer J, Johnson L, et al. Separate and combined associations of obesity and metabolic health with coronary heart disease: a pan-European case-cohort analysis. Eur Heart J. 2017;39(5):397–406.
Cornier MA, Despres JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124:1996–2019.
Karelis AD, Faraj M, Bastard JP, St-Pierre DH, Brochu M, Prud’homme D, et al. The metabolically healthy but obese individual presents a favorable inflammation profile. J Clin Endocrinol Metab. 2005;90:4145–50.
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med. 2008;168:1617–24.
Neeland IJ, Ayers CR, Rohatgi AK, Turer AT, Berry JD, Das SR, et al. Associations of visceral and abdominal subcutaneous adipose tissue with markers of cardiac and metabolic risk in obese adults. Obesity . 2013;21:E439–47.
Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012;97:2482–8.
Shimabukuro M, Kozuka C, Taira S, Yabiku K, Dagvasumberel M, Ishida M, et al. Ectopic fat deposition and global cardiometabolic risk: new paradigm in cardiovascular medicine. J Med Invest. 2013;60:1–14.
Fujimoto WY, Bergstrom RW, Boyko EJ, Chen KW, Leonetti DL, Newell-Morris L, et al. Visceral adiposity and incident coronary heart disease in Japanese-American men. The 10-year follow-up results of the Seattle Japanese-American Community Diabetes Study. Diabetes Care. 1999;22:1808–12.
Graffy PM, Pickhardt PJ. Quantification of hepatic and visceral fat by CT and MR imaging: relevance to the obesity epidemic, metabolic syndrome and NAFLD. Br J Radiol. 2016;89:20151024.
Menotti A, Lanti M, Maiani G, Kromhout D. Forty-year mortality from cardiovascular diseases and their risk factors in men of the Italian rural areas of the Seven Countries Study. Acta Cardiol. 2005;60:521–31.
Donahue RP, Abbott RD. Central obesity and coronary heart disease in men. Lancet. 1987;2:1215.
Yarnell JW, Patterson CC, Thomas HF, Sweetnam PM. Central obesity: predictive value of skinfold measurements for subsequent ischaemic heart disease at 14 years follow-up in the Caerphilly Study. Int J Obes Relat Metab Disord. 2001;25:1546–9.
Imeson JD, Haines AP, Meade TW. Skinfold thickness, body mass index and ischaemic heart disease. J Epidemiol Community Health. 1989;43:223–7.
Oppert JM, Charles MA, Thibult N, Guy-Grand B, Eschwege E, Ducimetiere P. Anthropometric estimates of muscle and fat mass in relation to cardiac and cancer mortality in men: the Paris Prospective Study. Am J Clin Nutr. 2002;75:1107–13.
Tanne D, Medalie JH, Goldbourt U. Body fat distribution and long-term risk of stroke mortality. Stroke. 2005;36:1021–5.
Freedman DS, Williamson DF, Croft JB, Ballew C, Byers T. Relation of body fat distribution to ischemic heart disease. The National Health and Nutrition Examination Survey I (NHANES I) Epidemiologic Follow-up Study. Am J Epidemiol. 1995;142:53–63.
van Lenthe FJ, van Mechelen W, Kemper HC, Twisk JW. Association of a central pattern of body fat with blood pressure and lipoproteins from adolescence into adulthood. The Amsterdam Growth and Health Study. Am J Epidemiol. 1998;147:686–93.
Hariri AA, Oliver NS, Johnston DG, Stevenson JC, Godsland IF. Adiposity measurements by BMI, skinfolds and dual energy X-ray absorptiometry in relation to risk markers for cardiovascular disease and diabetes in adult males. Dis Markers. 2013;35:753–64.
Durnin JV, Womersley J. Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr. 1974;32:77–97.
Kim J, Meade T, Haines A. Skinfold thickness, body mass index, and fatal coronary heart disease: 30 year follow up of the Northwick Park heart study. J Epidemiol Community Health. 2006;60:275–9.
Willett W. Anthropometric measures and body composition. In: Willett W, Hu F (eds.) Nutritional epidemiology. 3rd ed. Oxford: Oxford University Press; 2013. p. 529 Chapter 9.
Ludescher B, Machann J, Eschweiler GW, Vanhofen S, Maenz C, Thamer C, et al. Correlation of fat distribution in whole body MRI with generally used anthropometric data. Invest Radiol. 2009;44:712–9.
Bouchi R, Takeuchi T, Akihisa M, Ohara N, Nakano Y, Nishitani R, et al. High visceral fat with low subcutaneous fat accumulation as a determinant of atherosclerosis in patients with type 2 diabetes. Cardiovasc Diabetol. 2015;14:136.
Demura S, Sato S. Suprailiac or abdominal skinfold thickness measured with a skinfold caliper as a predictor of body density in Japanese adults. Tohoku J Exp Med. 2007;213:51–61.
Acknowledgements
The HDDRISC study was initiated the late Professor Victor Wynn, who directed it for much of its course. Data acquisition was sustained by many clinical, scientific, technical, nursing and administrative staff, to each of whom we extend our thanks.
Funding
Data acquisition for the HDDRISC study was funded by the Heart Disease and Diabetes Research Trust and the Rosen Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Loh, W.J., Johnston, D.G., Oliver, N. et al. Skinfold thickness measurements and mortality in white males during 27.7 years of follow-up. Int J Obes 42, 1939–1945 (2018). https://doi.org/10.1038/s41366-018-0034-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0034-0