Abstract
Background
Studies conducted during the 2009 influenza A (H1N1) pandemic found that obesity increases the risk of severe influenza including hospitalization and death. In this study, we examined the relationship of BMI with having laboratory-confirmed seasonal influenza and influenza-related respiratory hospitalization.
Methods
We linked a cohort of 246,494 adults aged ≥45 years with data on BMI to subsequent laboratory-confirmed influenza notifications and cause-specific hospitalizations from 2006 to 2015. Cox-proportional hazard models were used to estimate the risk of incident laboratory-confirmed influenza and influenza-related respiratory hospitalizations according to BMI, adjusting for age, sex and other covariates.
Results
After 1,840,408 person-years of follow-up, 1891 participants had laboratory-confirmed influenza notifications (crude rate 10.3/10,000 person-years) of whom 623 were hospitalized for a respiratory illness. Compared to those with healthy BMI (22.5 to <25.0 kg/m2), influenza incidence was respectively 27% (adjusted HR [aHR]: 1.27, 95% CI: 1.10–1.46) and 69% (aHR: 1.69, 1.24–2.29) greater among obese (BMI: 30 to <40 kg/m2) and very obese adults (40 to <50 kg/m2). The equivalent aHRs for hospitalization were 1.57 (95% CI: 1.22–2.01) and 4.81 (95% CI: 3.23–7.17). For every 5-unit BMI increase above 22.5 kg/m2, there was a 15% (aHR: 1.15, 95% CI: 1.09–1.22) increase in risk of having a diagnosis of influenza and 42% increase in hospitalization (aHR: 1.42, 95% CI: 1.30–1.60). These trends did not differ between the pandemic year (2009) and other years.
Conclusions
Our results suggest that obese adults have a similar risk of hospitalization for seasonal influenza as adults with cardiovascular disease and diabetes, and should therefore be equally prioritized for funded interventions such as targeted immunization programs.
Similar content being viewed by others
Introduction
Influenza causes significant morbidity, mortality, and economic loss with recent global estimates suggesting 3–5 million cases of severe illness and 250,000–500,000 deaths each year [1, 2]. Although moderately effective vaccines are available to prevent influenza, vaccine coverage is still suboptimal even in at-risk populations [3, 4].
In 2014, worldwide about 600 million adults were identified as obese (Body Mass Index (BMI) ≥ 30 kg/m2) [5]. The burden of obesity is even greater in industrialized countries such as Australia and the United States where recent studies suggest that, respectively, 30% and 36% of the adult population is obese [6, 7]. Currently in Australia, obese adults are strongly recommended for immunization against influenza, although unlike adults with diabetes, and pre-existing cardiac and respiratory diseases, they are not currently eligible for free vaccination under Australia’s National Immunization Program if they are under 65 years of age [8].
Following the 2009 pandemic of Influenza A (H1N1), several studies found that obesity increases the severity of influenza caused by the pandemic strain, including hospitalization and death [9,10,11,12,13]. However, less is known about the relationship between obesity and seasonal (non-pandemic) influenza. A systematic review examining risk factors for severe outcomes in patients with seasonal and pandemic influenza that searched available literature until March 2011 found only a single study quantifying the relationship between obesity and seasonal influenza [14]. Several studies conducted thereafter using data from non-pandemic influenza seasons have suggested that obesity increases the risk of severe influenza identified by hospitalization [15,16,17], admission to intensive care units (ICU) [18], and respiratory mortality [19] among influenza patients, however this has not been consistently reported [20, 21]. Also there is uncertainty about the relationship between obesity and the risk of having a diagnosis of laboratory-confirmed influenza or influenza-like illness (ILI) in non-pandemic influenza seasons [22,23,24].
In this study, we used prospective data from 246,000 adults aged ≥45 years, followed up over 10 influenza seasons (2006–2015) for laboratory-confirmed influenza, and influenza-related respiratory hospitalizations. Primarily, we examined the relationship of BMI with the risk of having laboratory-confirmed seasonal influenza and influenza-related respiratory hospitalization.
Methods
Setting, participants, and data sources
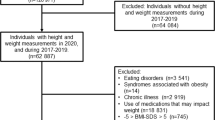
We used a cohort of 265,951 adults aged ≥45 years, living in New South Wales, Australia, and recruited into the Sax Institute’s 45 and Up Study between 2006 and 2009. The cohort profile has been published elsewhere [25]. In brief, adults ≥45 years were randomly sampled from the National health insurance enrolment database (formerly known as Medicare Australia), and invited to participate. Those who agreed completed a baseline questionnaire at recruitment, providing information on socio-demographics, health, lifestyle, and self-reported height and body-weight. Participants consented for long-term follow-up and record linkage of their information to a wide range of healthcare-related administrative databases [25].
Cohort data from the baseline were linked to the Notifiable Conditions Information Management System (NCIMS), the NSW Admitted Patient Data Collection (APDC), and the NSW Registry of Births, Deaths and Marriages (RBDM). The NSW Centre for Health Record Linkage (CHeReL) conducted the linkages to the NCIMS, APDC, and RBDM using a probabilistic matching method [26].
Under the NSW Public Health Act 2010, laboratories are required to notify confirmed influenza. These notifications are compiled by NSW Health into the NCIMS [27]. Data compiled in the NCIMS include the condition notified, estimated date of onset, details of laboratory confirmation, and type of specimen [27]. For influenza, the date of onset is usually estimated by the date the specimen was taken from the patient. The APDC database records all hospitalizations occurring in NSW and includes data on the date of admission and discharge, the primary diagnosis for hospitalization, and up to 49 secondary diagnoses that affected the treatment or length of stay. Diagnoses are coded using the International Classification of Disease 10th revision, Australian Modification (ICD-10-AM) [28]. The RBDM records the date of all births, deaths and marriages of NSW residents. For this study, the NCIMS, APDC, and RBDM databases were complete up to 31 December 2015.
Study variables
The primary outcome was laboratory-confirmed influenza diagnosis recorded in the NCIMS that linked to the 45 and Up Study participants. The secondary outcome was influenza-related respiratory hospitalization, which was ascertained when a participant had an influenza notification and a linked respiratory disease-coded hospitalization (ICD10 J-codes) in the APDC records that occurred within a week before and up to 2 weeks after the onset of influenza.
BMI was calculated using self-reported body weight and height at the time of enrolment, as a ratio of weight in kilograms to square of height in metres. BMI was categorized using the following cut-points (corresponding WHO BMI classification shown in brackets): 15.0 to <18.5 (underweight), 18.5 to <22.5 (normal weight), 22.5 to <25.0 (normal weight), 25.0 to <30.0 (overweight), 30.0 to <40.0 (obese class I and II), 40.0 to <50.0 (obese class III) [29].
Covariates
The information on covariates used in the analyses was obtained from data provided in the baseline questionnaire. The covariates included age, sex, annual household income (<$AUD70,000/year, ≥$AUD70,000/year), area of residence (major city, inner regional, outer regional/remote/very-remote) [30], education (no formal education, school/diploma, university), private health insurance (yes, no), alcohol consumption (≤1 drink/day, >1 drink/day), smoking (never, current, past).
Statistical methods
Participants with extreme levels of BMI (≤15.0 and ≥50.0 kg/m2) and where BMI could not be calculated due to missing information were excluded from the analyses. Follow-up time was estimated from the date of recruitment to the date of first influenza event, date of death or last date for which we had follow-up records (31 December 2015), whichever came first. We calculated laboratory-confirmed influenza notification rates for each BMI category. We then modelled the relationship between BMI and influenza using Cox proportional hazard models adjusting for important covariates with BMI 22.5 to <25.0 kg/m2 as the reference category. Age at baseline was the underlying time variable; sex, area of residence, income and smoking were selected a priori to be included in the model. Education, alcohol consumption, and private health insurance were added to the model if their inclusion changed the point estimate of the relationship between BMI and influenza by at least 10%. Missing values for each covariate were assigned as a separate category in analyses. Further, we tested for trend of notified influenza and respiratory hospitalization per 5-unit increase in BMI in adults with BMI ≥ 22.5 kg/m2. Test for trend was performed by modelling the median BMI value in each BMI category as a continuous variable. We then stratified the trend analyses according to various sociodemographic, lifestyle factors, and co-morbidity status. Co-morbidity was defined as the presence of at least one of the following conditions: self-reported diabetes, heart disease hospitalization (ICD 10 codes: I20-I25) in the 5 years prior to enrolment, self-reported asthma, and respiratory hospitalization for chronic respiratory disease (ICD10 codes: J40-J45) in the 5 years prior to enrolment. We also examined risks for notified influenza that occurred in the year of the last pandemic (2009), and all other years excluding 2009. Similar analyses were conducted to examine the relationship between BMI and influenza-related respiratory hospitalization.
All analyses were conducted in STATA 14 software. The conduct of the 45 and Up Study was approved by the University of New South Wales Human Research Ethics Committee (HREC). This specific study was approved by the NSW Population Health Research Ethics Committee, and the University of New South Wales Human Research Ethics Committee (2010/12/292).
Results
Of the 265,951 participants, we included 246,494 (92.7%) in the main analysis who had valid BMI data. The mean age of the participants at baseline was 62.6 years (standard deviation (SD)—11.1 years) and 53% were female. Detailed distribution of characteristics according to BMI categories is shown in Table 1. In brief, 21.8% of participants were obese, 39.6% were overweight, 36.9% were healthy weight, and 1.3% were underweight. The average age of healthy weight and obese participant was 63.1 years (SD: 11.9) and 61.1 years (SD: 9.8), respectively. The proportion of current smokers among obese participants (BMI: 30.0 to <50.0 kg/m2) was 6.8% compared to 7.9% in healthy weight participants (BMI: 18.5 to <25.0 kg/m2).
The 246,494 participants were followed up for 1,840,408 person-years and 1919 laboratory-confirmed notifications of influenza were recorded in 1891 participants; 185 in 2009 and 1706 in other years. All subsequent analyses included only the first influenza notification.
The crude influenza notification rate was 10.3/10,000 person-years (95% CI: 9.8–10.7). When adjusted for covariates in the final model (age, sex, income, area of residence, and smoking) compared to BMI 22.5 to <25.0 kg/m2, the risk of notified influenza was 27% (adjusted Hazard Ratio (aHR): 1.27 (95% CI: (1.10–1.46)) and 69% (aHR: 1.69 (95% CI: 1.24–2.29) higher in those with BMI 30.0 to <40.0 kg/m2 and 40.0 to <50.0 kg/m2, respectively (Fig. 1 and Appendix I).
Association between body mass index (BMI) and all notified influenza infection. Adjusted for: age, sex, income, area of residence, smoking (the squares represent the point estimates, and the vertical lines represent the 95% CI. Size of squares are proportional to the number of events. The HR are plotted at median BMI values for categories: 15.0 to <18.5, 18.5 to <22.5, 22.5 to <25.0, 25.0 to <30.0, 30.0 to <40.0, 40.0 to <50.0 kg/m2)
Figure 2 shows the trend in the hazard ratio of having notified influenza per 5-unit increase in BMI among people with BMI ≥ 22.5 kg/m2 overall and stratified by age, sex, lifestyle factors, and co-morbidity, adjusted for all other covariates. Overall, we observed a 15% increase in the risk of having notified influenza per 5-unit increase in BMI (aHR: 1.15, 95% CI: 1.09–1.22) (p < 0.001). This risk did not differ significantly when examined in subgroups of age (45–64 or ≥65 years), sex, smoking status, or other sociodemographic and health-related factors. It was also similar for influenza diagnosed in 2009 as it was for influenza diagnosed in other years (Fig. 2).
Trend in influenza notification per 5-unit increase in body mass index (BMI) according to sociodemographic, and life-style factors and co-morbidities in those with BMI ≥ 22.5 kg/m2. Co-morbidities include self-reported diabetes, self-reported asthma or respiratory hospitalization within 5 years prior to enrolment, and hospitalization for heart disease within 5 years prior to enrolment (see Methods). Participants (N = 40161) with BMI < 22.5 kg/m2 were excluded from the analyses. The solid vertical line represents the null, and vertical dotted line represents the overall HR per 5-unit increase in BMI
Of those participants with laboratory-confirmed influenza, 36% (682/1891) had at least one hospitalization event within a week prior and up to 2 weeks after the date of influenza notification (total of 950 hospital separations in 682 participants). Of the 950 hospital separations, 38.1% (N = 362/950) had a primary diagnosis specifically coded as influenza or pneumonia (ICD-10 J09-J18), a further 26.5% (n = 252) were coded as another respiratory illness (ICD-10 J-codes other than J09-J18) and the remaining 35.4% (n = 336) had non-respiratory-related primary diagnosis codes (see Appendices II and III). Of those hospital separations without a primary diagnosis of a respiratory illness, 29.2% (98/336) had at least one secondary diagnosis code for influenza or pneumonia, and 10.4% (35/336) had at least one secondary diagnosis code for a respiratory illness other than influenza or pneumonia. Overall 32.9% of participants with an influenza notification (623/1891) had a hospitalization where either the primary or secondary diagnosis codes indicated a respiratory disease and were included as cases in analyses of influenza-related respiratory hospitalizations.
Figure 3 shows the relationship between BMI and influenza-related respiratory hospitalizations. Compared to those with BMI 22.5 to <25.0 kg/m2, the aHR for an influenza-related respiratory hospitalization was 1.57 (95% CI: 1.22–2.01) for those with BMI 30.0 to <40.0 kg/m2 and 4.81 (95% CI: 3.23–7.17) for those with BMI 40.0 to <50.0 kg/m2. It was also significantly higher for underweight participants (aHR: 2.23, 95% CI: 1.37–3.64) (Appendix IV). The overall trend for an increase in risk of influenza-related respiratory hospitalization in those with BMI ≥ 22.5 kg/m2 was substantially greater than that for notified influenza (aHR: 1.42, 95% CI: 1.30–1.60 per 5-unit increase in BMI). The trend for increase in risk of influenza-related respiratory hospitalization per 5-unit increase in BMI during the pandemic influenza year (2009) did not differ from other seasonal influenza years (aHR: 1.67, 95% CI: 1.28–2.17, and aHR :1.40, 95% CI: 1.26–1.54).
Association between body mass index (BMI) and notified influenza infection according to influenza-related respiratory hospitalization. Adjusted for age, sex, income, area of residence, and smoking (the squares represent the point estimates, and the vertical lines represent the 95% CI. The HRs of two groups are plotted at the same median values of BMI categories: 15.0 to <18.5, 18.5 to <22.5, 22.5 to <25.0, 25.0 to <30.0, 30.0 to <40.0, 40.0 to <50.0 kg/m2, but for the purpose of clear visualization one is slightly shifted to the right)
When the outcome was defined as notified influenza not requiring hospitalization, we did not observe any significant association with obesity or underweight (Fig. 3 and Appendix V). The overall trend of increase in risk of notified but not hospitalized influenza per 5-unit increase in BMI was aHR: 1.02 (95% CI: 0.95–1.10).
Discussion
In this study, we observed an increased risk of laboratory-confirmed notified influenza and influenza-related respiratory hospitalizations in obese middle-aged and older adults. In those with BMI ≥ 22.5 kg/m2, for every 5 kg/m2 increase in BMI, the risk of notified influenza increased by 15%, and the risk of influenza-related hospitalization by 42%. We found the risk of influenza in relation to BMI was similar for 2009 (Influenza A (H1N1) pandemic year) as for other seasonal influenza years. It was also similar comparing adults of different ages (45–64 and ≥65 years), and between smokers and non-smokers. Our results add to the growing evidence of a role of BMI in increasing the risk of diagnosed influenza and respiratory hospitalization not only in the pandemic year but also in seasonal influenza years, particularly after 2009. To our knowledge, this is also the first prospective study to examine and report the association of laboratory-confirmed seasonal influenza in relation to BMI.
There is increasing evidence regarding the immunopathological relationship between higher BMI and influenza. Obesity impairs the immunological response to influenza infection as well as influenza vaccination by altering the normal cellular immune system [31]. Several immunopathological mechanisms related to obesity such as defects in CD4+ and CD8+ T-cells, delay in expression of proinflammatory cytokines in humans [32,33,34,35] or other immune responses that may increase the risk of severe disease due to infection with Influenza A (H1N1) have been described in mice models [34, 36]. A recent study also suggests that the risk of having a diagnosis of influenza or ILI is twice in immunized obese adults compared to immunized healthy weight adults despite comparable serological response to the immunization [24].
The relationship between obesity and influenza gained prominence with the 2009 pandemic of Influenza A (H1N1) with initial reports suggesting a higher risk of hospitalization, intensive care admission and death in obese adults [9, 12, 13, 37, 38]. A systematic review found that among individuals hospitalized for influenza, the risk of intensive care unit (ICU) admission or death due to Influenza A (H1N1) was two times greater in severely obese (BMI ≥ 40.0 kg/m2) compared to healthy weight individuals [12]. Also, studies of community-based adults have reported that the risk of hospitalization due to Influenza A (H1N1) is greater in obese compared to healthy weight individuals [9, 37].
There have been fewer studies examining the association between obesity and laboratory-confirmed influenza or influenza-like illness in non-pandemic seasons [22,23,24]. A study conducted between 2007 and 2009 with laboratory-confirmed influenza cases (n = 705) and test negative controls (with non-influenza respiratory illness) found no significant association between obesity and the risk of medically attended laboratory diagnosed influenza in a community dwelling US population for Influenza A (H1N1) as well as infection due to other strains [23]. Another case–control study suggested a modest but significant association between obesity (BMI: ≥30.0 kg/m2) and influenza-like illness in outpatients both in 2009 and the years 2004–2005, but the same study also reported no significant association between obesity and hospitalized influenza-like illness [22]. A recent study also suggested an increased risk of influenza and influenza-like illness in vaccinated obese adults compared to vaccinated healthy weight adults, but this difference may be due to the relative inefficacy of vaccine to protect the obese adults [24]. Reasons for the lack of agreement between studies may be smaller sample sizes leading to non-significant results [22], and the use of test-negative controls that had non-influenza-related respiratory illnesses (as obese people may also be at higher risk of respiratory infections other than influenza) [23, 39].
In this study, we observed a higher risk of seasonal influenza-related hospitalization in obese adults. Consistent with our findings, some earlier studies have also described a higher risk of hospitalization and other severe outcomes due to seasonal influenza among obese individuals [15,16,17,18,19]. For example, Kwong et al. [17] reported increased odds ratios for respiratory hospitalization of 1.45 and 2.12 for individuals with BMI 30.0 to <40.0 kg/m2 and BMI 40.0 to <50.0 kg/m2 compared to healthy weight people in the influenza seasons of 1996/97 through to 2007/08 in Ontario, Canada. Whereas, Charland et al. [16] reported a 12% increase in influenza-related hospitalization per 5% increase in prevalence of obesity in the years 2002–2008 in the United States.
We also observed an increased risk of seasonal influenza-related respiratory hospitalization in underweight participants (aHR = 2.23) compared to healthy weight participants. A recent systematic review also concluded that there is a higher risk of influenza-related pneumonia in underweight participants [40], and the authors argue that such a relationship may be due to malnutrition and undiagnosed comorbid conditions that may increase the risk of infection [40].
The results of our study should be interpreted carefully. We used influenza notifications to identify those infected. As up to 80% of those with influenza may not visit a healthcare facility, and only a fraction of those who do are likely to be tested, our rates of influenza notifications will underestimate the true rates [41, 42]. It is possible that if clinical presentation and testing for influenza differs according to BMI then our hazard ratio estimates may be biased although this type of ascertainment bias is less likely to occur with hospitalizations. We also lacked information on annual influenza vaccination and could not adjust for this in our analyses. However, when we examined the risks by subgroups known to have significantly higher vaccination uptake such as those ≥ 65 years and those with co-morbidities [43], we found our results were generally consistent. We also know from a separate survey on a subset of our cohort conducted between 2012–2015 that overweight/obese people are more likely to have received influenza vaccination [3]. Therefore, it is likely our inability to adjust for influenza vaccination status would lead to an underestimation of the effect of obesity on influenza risk. Data on BMI were based on self-reported height and weight data collected at study entry but evidence indicates that self-reported data for BMI show excellent validity [44], and the change in BMI in older adults is not great over the 7-year average follow-up period for this analysis [45]. While we found obesity effects were similar in 2009 as in other years, we had relatively few cases of influenza in 2009 compared to all other years and, as only 30% of influenza notifications were subtyped, we were unable to examine the effects of BMI on different influenza types. Given that national surveillance data for the years 2010–2015 report 23.6% of total laboratory-confirmed influenza in Australian influenza surveillance sites were influenza A (H1N1) [46], and the majority of our influenza notifications and hospitalizations occurred in the years following 2009, it is possible that the increase in risk in relation to BMI that we observed in seasons other than 2009 may be due to circulating Influenza A (H1N1) in the years following 2009.
Current immunization guidelines in Australia recognize the elevated risk of influenza associated with obesity and strongly recommend influenza vaccine for obese adults but unlike people with cardiac disease and diabetes, influenza vaccination for obese people aged <65 years is not funded under the National Immunisation Program [8]. This means obese adults without the other risk factors need to pay for the vaccine. However, the risk ratios for hospitalization for seasonal influenza in obese adults that we observed were comparable to or higher than that reported for adults with cardiovascular diseases and diabetes in other studies [14, 17, 47].
In conclusion, we observed that during both the pandemic (2009) and recent seasonal influenza years, obesity was independently associated with having laboratory-confirmed influenza but the association was primarily driven by severe influenza requiring hospitalization with about a 40% increase for every 5 kg/m2 increase in BMI above 22.5 kg/m2. This increase in risk is comparable to that reported among adults with cardiac disease and diabetes [14, 17, 47], suggesting that obese adults should be equally prioritized for funding for targeted immunization programs to prevent severe influenza.
Data availability
The Sax Institute’s 45 and Up study baseline data linked with MBS and PBS data were obtained from the Sax Institute and are available upon request to the Sax Institute (Level 13, Building 10, 235 Jones Street, Ultimo NSW 2007, Australia (+61) 02 9188 9500; 45andUp.research@saxinstitute.org.au). Linked NCIMS, APDC, EDDC, and RBDM data were obtained from the NSW Ministry of Health and are available upon request to the Centre for Health Record Linkage (CHeReL) (Level 7, 73 Miller Street, North Sydney NSW 2015, Australia; cherel.mail@moh.health.nsw.gov.au).
Disclaimer
The funders had no role in study design, data collection, management, analyses, interpretation of study results and no influence in preparation, review and approval of manuscript.
References
World Health Organization. Influenza (seasonal), Fact sheet. 2016. http://www.who.int/mediacentre/factsheets/fs211/en/. Accessed 15 May 2017.
Nicholson KG, Wood JM, Zambon M. Influenza. Lancet. 2003;362:1733–45.
Dyda A, Karki S, Hayen A, MacIntyre CR, Menzies R, Banks E, et al. Influenza and pneumococcal vaccination in Australian adults: a systematic review of coverage and factors associated with uptake. BMC Infect Dis. 2016;16:515.
Blank PR, Szucs TD. Increasing influenza vaccination coverage in recommended population groups in Europe. Expert Rev Vaccin. 2009;8:425–33.
World Health Organization. Obesity and Overweight, Fact sheet. 2016. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 15 May 2017.
Australian Bureau of Statistics. National Health Survey, First Results, Australia 2014-2015. http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0012014-15?OpenDocument. Accessed 15 May 2017.
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among us adults, 1999-2010. JAMA. 2012;307:491–7.
Australian Government, Department of Health. The Australian Immunisation Handbook, 10th Edition. http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/7B28E87511E08905CA257D4D001DB1F8/$File/Aus-Imm-Handbook.pdf. Accessed 15 May 2017.
Martin V, Castilla J, Godoy P, Delgado-Rodriguez M, Soldevila N, Fernandez-Villa T, et al. High body mass index as a risk factor for hospitalization due to influenza: a case-control study. Arch Bronconeumol. 2016;52:299–307.
Centers for Disease C, Prevention. Intensive-care patients with severe novel influenza A (H1N1) virus infection - Michigan, June 2009. MMWR Morb Mortal Wkly Rep. 2009;58:749–52.
Sun Y, Wang Q, Yang G, Lin C, Zhang Y, Yang P. Weight and prognosis for influenza A(H1N1)pdm09 infection during the pandemic period between 2009 and 2011: a systematic review of observational studies with meta-analysis. Infect Dis. 2016;48:813–22.
Fezeu L, Julia C, Henegar A, Bitu J, Hu FB, Grobbee DE, et al. Obesity is associated with higher risk of intensive care unit admission and death in influenza A (H1N1) patients: a systematic review and meta-analysis. Obes Rev. 2011;12:653–9.
Louie JK, Acosta M, Samuel MC, Schechter R, Vugia DJ, Harriman K, et al. A novel risk factor for a novel virus: obesity and 2009 pandemic influenza A (H1N1). Clin Infect Dis. 2011;52:301–12.
Mertz D, Kim TH, Johnstone J, Lam PP, Science M, Kuster SP, et al. Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ. 2013;347:f5061.
Tempia S, Walaza S, Moyes J, Cohen AL, von Mollendorf C, Treurnicht FK, et al. Risk factors for influenza-associated severe acute respiratory illness hospitalization in South Africa, 2012-2015. Open Forum Infect Dis. 2017;4:ofw262.
Charland KM, Buckeridge DL, Hoen AG, Berry JG, Elixhauser A, Melton F, et al. Relationship between community prevalence of obesity and associated behavioral factors and community rates of influenza-related hospitalizations in the United States. Influenza Other Respir Virus. 2013;7:718–28.
Kwong JC, Campitelli MA, Rosella LC. Obesity and respiratory hospitalizations during influenza seasons in Ontario, Canada: a cohort study. Clin Infect Dis. 2011;53:413–21.
Dimitrijevic D, Ilic D, Rakic Adrovic S, Suljagic V, Pelemis M, Stevanovic G, et al. Predictors of hospitalization and admission to intensive care units of influenza patients in serbia through four influenza seasons from 2010/2011 to 2013/2014. Jpn J Infect Dis. 2017;70:275–83.
Zhou Y, Cowling BJ, Wu P, Chan WM, Lee SY, Lau EH, et al. Adiposity and influenza-associated respiratory mortality: a cohort study. Clin Infect Dis. 2015;60:e49–57.
Braun ES, Crawford FW, Desai MM, Meek J, Kirley PD, Miller L, et al. Obesity not associated with severity among hospitalized adults with seasonal influenza virus infection. Infection. 2015;43:569–75.
Blumentals WA, Nevitt A, Peng MM, Toovey S. Body mass index and the incidence of influenza-associated pneumonia in a UK primary care cohort. Influenza Other Respir Virus. 2012;6:28–36.
Cocoros NM, Lash TL, DeMaria A Jr, Klompas M. Obesity as a risk factor for severe influenza-like illness. Influenza Other Respir Virus. 2014;8:25–32.
Coleman LA, Waring SC, Irving SA, Vandermause M, Shay DK, Belongia EA. Evaluation of obesity as an independent risk factor for medically attended laboratory-confirmed influenza. Influenza Other Respir Virus. 2013;7:160–7.
Neidich SD, Green WD, Rebeles J, Karlsson EA, Schultz-Cherry S, Noah TL, et al. Increased risk of influenza among vaccinated adults who are obese. Int J Obes. 2017;41:1324–30.
45 and Up Study Collaborators, Banks E, Redman S, Jorm L, Armstrong B, Bauman A, et al. Cohort profile: the 45 up study. Int J Epidemiol. 2008;37:941–7.
Centre for Health Record Linkage (CHeReL): Quality assurance. http://www.cherel.org.au/media/24160/qa_report_2012.pdf. Accessed 14 May 2017.
Center for Health Record Linkage. Data dictionaries- Notifiable Conditions Information Management System (NCIMS). http://www.cherel.org.au/media/29612/ncims_data_dictionary_feb_2014-a.docx. Accessed 17 May 2017.
Center for Health Record Linkage. Data dictionaries- NSW Admitted Patient Data Collection (APDC). http://www.cherel.org.au/data-dictionaries#section1. Accessed 17 May 2017.
World Health Organization. Body Mass Index—BMI. 2017. http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Accessed 18 May 2017.
Australian Institute of Health and Welfare. Rural, Regional and Remote Health: A Guide to Remoteness Classifications. Rural Health Series No. 4. AIHW Cat. No. PHE 53. AIHW, Canberra. 2004. http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=6442459567. Accessed 7 Aug 2017.
Green WD, Beck MA. Obesity impairs the adaptive immune response to influenza virus. Ann Am Thorac Soc. 2017;14:S406–S409.
Paich HA, Sheridan PA, Handy J, Karlsson EA, Schultz-Cherry S, Hudgens MG, et al. Overweight and obese adult humans have a defective cellular immune response to pandemic H1N1 influenza A virus. Obesity. 2013;21:2377–86.
Karlsson EA, Sheridan PA, Beck MA. Diet-induced obesity in mice reduces the maintenance of influenza-specific CD8+ memory T cells. J Nutr. 2010;140:1691–7.
Smith AG, Sheridan PA, Harp JB, Beck MA. Diet-induced obese mice have increased mortality and altered immune responses when infected with influenza virus. J Nutr. 2007;137:1236–43.
Painter SD, Ovsyannikova IG, Poland GA. The weight of obesity on the human immune response to vaccination. Vaccine. 2015;33:4422–9.
Peiris JS, Hui KP, Yen HL. Host response to influenza virus: protection versus immunopathology. Curr Opin Immunol. 2010;22:475–81.
Morgan OW, Bramley A, Fowlkes A, Freedman DS, Taylor TH, Gargiullo P, et al. Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease. PLoS ONE. 2010;5:e9694.
Van Kerkhove MD, Vandemaele KA, Shinde V, Jaramillo-Gutierrez G, Koukounari A, Donnelly CA, et al. Risk factors for severe outcomes following 2009 influenza A (H1N1) infection: a global pooled analysis. PLoS Med. 2011;8:e1001053.
Campitelli MA, Rosella LC, Kwong JC. The association between obesity and outpatient visits for acute respiratory infections in Ontario, Canada. Int J Obes. 2014;38:113–9.
Phung DT, Wang Z, Rutherford S, Huang C, Chu C. Body mass index and risk of pneumonia: a systematic review and meta-analysis. Obes Rev. 2013;14:839–57.
Flahault A, de Lamballerie X, Hanslik T. Symptomatic infections less frequent with H1N1pdm than with seasonal strains: Antoine Flahault, Xavier de Lamballerie, Camille Pelat, Nicolas Salez, Thomas Hanslik. PLoS Curr. 2009;1:RRN1140.
Leung NH, Xu C, Ip DK, Cowling BJ. Review article: the fraction of influenza virus infections that are asymptomatic: a systematic review and meta-analysis. Epidemiology. 2015;26:862–72.
Dyda A, MacIntyre CR, McIntyre P, Newall AT, Banks E, Kaldor J, et al. Factors associated with influenza vaccination in middle and older aged Australian adults according to eligibility for the national vaccination program. Vaccine. 2015;33:3299–305.
Ng SP, Korda R, Clements M, Latz I, Bauman A, Bambrick H, et al. Validity of self-reported height and weight and derived body mass index in middle-aged and elderly individuals in Australia. Aust N Z J Public Health. 2011;35:557–63.
Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
World Health Organization, 2017. Influenza, FluNet. http://apps.who.int/flumart/Default?ReportNo=12. Accessed 24 Jul 2017.
Lau D, Eurich DT, Majumdar SR, Katz A, Johnson JA. Working-age adults with diabetes experience greater susceptibility to seasonal influenza: a population-based cohort study. Diabetologia. 2014;57:690–8.
Acknowledgements
This research was completed using data collected through the 45 and Up Study (www.saxinstitute.org.au). The 45 and Up Study is managed by the Sax Institute in collaboration with major partner Cancer Council NSW; and partners: the National Heart Foundation of Australia (NSW Division); NSW Ministry of Health; NSW Government Family & Community Services—Ageing, Carers and the Disability Council NSW; and the Australian Red Cross Blood Service. We thank the many thousands of people participating in the 45 and Up Study.
Funding
This work was supported by National Health and Medical Research Council (NHMRC) grant (Grant number: 1048180). EB, AN, and BL are supported by NHMRC Fellowships.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
PM sits on the Australian Government expert advisory committee for immunization. EB chairs the Australian Government Advisory Committee on the Safety of Vaccines. CRM had received funding and/or laboratory testing support for investigator driven research from CSL Biotherapies, Pfizer and Merck but not related to this research. She has participated in advisory boards for Pfizer, Merck and GSK. All other authors declare no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Karki, S., Muscatello, D.J., Banks, E. et al. Association between body mass index and laboratory-confirmed influenza in middle aged and older adults: a prospective cohort study. Int J Obes 42, 1480–1488 (2018). https://doi.org/10.1038/s41366-018-0029-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0029-x
This article is cited by
-
The TIGIT+ T regulatory cells subset associates with nosocomial infection and fatal outcome in COVID-19 patients under mechanical ventilation
Scientific Reports (2023)
-
Association between obesity and COVID-19 mortality and length of stay in intensive care unit patients in Brazil: a retrospective cohort study
Scientific Reports (2022)