Abstract
Prior studies in predominantly European (Caucasian) populations have discovered common genetic variants (single nucleotide polymorphisms, SNPs) associated with leukocyte telomere length (LTL), but whether these same variants affect LTL in non-Caucasian populations are largely unknown. We investigated whether six genetic variants previously associated with LTL (TERC (rs10936599), TERT (rs2736100), NAF1 (7675998), OBFC1 (rs9420907), ZNF208 (rs8105767), and RTEL1 (rs755017)) are correlated with telomere length (TL) in peripheral blood mononuclear cells (PBMCs) in a cohort of Africans living with and without HIV and undergoing evaluation for tuberculosis (TB). We found OBFC1 and the genetic sum score of the effect alleles across all six loci to be associated with shorter TL (adjusted for age, gender, HIV status, and smoking pack-years (p < 0.02 for both OBFC1 and the genetic sum score). In an analysis stratified by HIV status, the genetic sum score is associated with LTL in both groups with and without HIV. On the contrary, a stratified analysis according to TB status revealed that in the TB-positive subgroup, the genetic sum score is not associated with LTL, whereas the relationship remains in the TB-negative subgroup. The different impacts of HIV and TB on the association between the genetic sum score and LTL indicate different modes of modification and suggest that the results found in this cohort with HIV and TB participants may not be applied to the African general population. Future studies need to carefully consider these confounding factors.
Similar content being viewed by others
Introduction
Telomeres are nucleotide sequences that cap the ends of linear chromosomes to protect them from degradation over cycles of replication [1]. Typically, they contain tandem repeats of TTAGGG sequence, which is maintained by the enzyme telomerase [2]. These 10–15 kb telomeric sequences gradually shorten over time, leading to cell senescence and apoptosis [3]. Shorter mean leukocyte telomere length (LTL) is associated with a high risk of several major age-associated diseases [4,5,6] and has been advanced as a marker of biological aging. Chronic infections, such as HIV, accelerate the replicative aging of the peripheral immune system [7] and have been associated with many of the same diseases associated with shorter LTL, despite successful antiviral treatment [8,9,10].
Genetic inheritance plays a major role in telomere length (TL) determination with a reported heritability of up to 82% [11]. However, only a handful of common genetic variants (single nucleotide polymorphisms, SNPs) have been found to contribute to the interpersonal variations in LTL [4]. Genetic sum scores that combined these TL associated SNPs as the instrument variable in Mendelian randomization studies have shown that TL is causally associated with aging-related diseases, such as cardiovascular disease, some types of cancer, and lung diseases [12,13,14,15,16,17]. The use of these TL associated SNPs, as opposed to TL measured from leukocytes, allows unbiased estimates of the effect of TL as a biomarker for disease risk, without the potential impact of reverse causation and confounders.
These prior SNP studies were conducted in predominantly European (Caucasian) populations, with only a limited number of studies in Asian populations. As the frequencies of these TL SNPs are different for different world populations [18], studies conducted in the European and Asian populations may not apply to other populations, such as Africans [19]. In fact, two previous papers reported that the association of TL and SNPs is either weakened [20] or not found in other racial groups [21]. Determining how TL SNPs contribute to observed TL is important to understanding the underlying mechanisms of how TL contributes to diseases in these different populations. In an African (Ugandan) cohort of persons living with and without HIV and undergoing evaluation for tuberculosis (TB) [22], we measured TL from peripheral blood mononuclear cells (PBMCs) and investigated the associations between measured TL and the top six previously reported TL SNPs (in TERC, TERT, NAF1, OBFC1, ZNF208, and RTEL1, respectively) and their genetic sum score. Our goals are twofold: (1) To examine whether the associations between these SNPs, the sum score and the measured TL also exist in this Uganda cohort, and (2) To examine if HIV or TB infection modifies these associations. To our knowledge, this is the first report of an African population with TL SNP data.
Materials and methods
IHOP and I AM OLD study participants
This study is a substudy of the International HIV-associated Opportunistic Pneumonias (IHOP) Study (May 2013 to December 2014) and the Inflammation, Aging, Microbes, and Obstructive Lung Disease (I AM OLD) Study (January 2015 to May 2016) and examined a single cohort comprised of persons living with HIV (PLHIV) and persons without HIV. In brief, both these studies enrolled consecutive adults (>18 years) who were admitted to Mulago National Referral Hospital in Kampala, Uganda with cough and suspected TB. We administered a standardized questionnaire and reviewed hospital records to obtain demographic and clinical information and to assess cardiopulmonary comorbidities, cigarette smoke exposure, and alcohol consumption. Rapid HIV serological testing was performed on participants unless prior HIV infection was confirmed previously. Patients with a prior positive HIV diagnosis were asked about their use of antiretroviral therapy (ART). CD4+ T-cell counts were measured on all PLHIV at the time of study enrollment. All patients underwent a standardized evaluation for TB that included expectorated sputum sent for acid-fast bacilli (AFB) smear and mycobacterial culture using both Lowenstein–Jensen and Mycobacterial Growth Indicator Tube (MGIT). Those patients who had a negative sputum AFB smear examination provided an additional expectorated sputum sent for Xpert® MTB/RIF (Cepheid). Patients who had both negative sputum AFB smear examination and negative Xpert® MTB/RIF underwent bronchoscopy with bronchoalveolar lavage, which was sent for AFB smear and Lowenstein–Jensen and MGIT cultures. Patients were considered to be TB positive if they had any positive result (AFB smear, Xpert, and/or culture) or were empirically treated for TB based on a high clinical suspicion. Patients with no positive results, two negative Lowenstein–Jensen mycobacterial cultures, and no empiric TB therapy were considered to be TB negative. Of this study that enrolled patients undergoing evaluation for TB from May 2013 to May 2016, 439 total participants underwent genotyping for the six TL SNPs. TL (expressed as the ratio of telomere vs. single-copy gene ratio T/S) was determined for these participants, 434 of which were valid. The IHOP and I AM OLD studies were approved by UCSF’s Institutional Review Board/Committee on Human Research, as well as the Mulago Hospital Research and Ethics Committee, the Makerere University School of Medicine Research and Ethics Committee, and the Uganda National Council for Science and Technology. Written informed consent was obtained from all participants and the work was conducted in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki).
DNA extraction and telomere length measurement
“PBMCs” were obtained from venous blood draw using CPT tubes according to manufacturer’s instructions (BD Vacutainer® CPT™ Mononuclear Cell Preparation Tube—Sodium Heparin, BD Biosciences, San Jose, CA, USA). Total genomic DNA was extracted from PBMCs using the QIAamp DNA Blood Mini extraction kit (QIAGEN, Hilden, Germany). DNA concentration was measured using the NanoDrop 2000 (Thermo Fisher Scientific, Waltham, MA, USA). The acceptance criteria for genomic DNA were OD260/OD280 between 1.7 and 2.0.
Mean PBMC TL was measured using quantitative PCR as described previously [23], using a modified version of Cawthon’s method [24]. TL was expressed as a ratio of the telomere repeat length (T) to copy number for a single-copy gene (S) in each sample. Laboratory personnel who performed the assays were blinded to all other demographic and clinical data, as well the SNP data.
SNP selection and genotyping
In this study, the top six SNPs associated with TL reported by previous studies were selected for analysis, with the lower-frequency alleles set as the minor allele. The effect allele is set as the short TL allele as has been previously reported [12]. Genotypes of TERC, TERT, NAF1, OBFC1, ZNF208, and RTEL1 were determined using 10 ng of DNA in 5 μL reactions on a 384-well plate using TaqMan SNP assay primers (Thermo Fisher Scientific, Waltham, MA, USA) and LightCycler® 480 Probes Master Mix (Roche Diagnostics Corporation, Indianapolis, IN, USA). Reactions took place in a LightCycler® 480 (Roche Diagnostics Corporation) using the Endpoint Genotyping Dual Color Hydrolysis Probe Analysis program. Genotypes were called by the program and confirmed by inspecting cluster plots. Assays were validated by duplicates in initial runs using 14 samples.
Calculation of unweighted genetic sum score, weighted score for each individual SNP and the weighted genetic sum score
The unweighted genetic sum scores for each sample were determined by summing the number of effect alleles (short TL allele is defined as the effect allele as described in Codd et al. [12]) that the sample contained across all six TL-associated variants, with the long/long, short/long, and short/short phenotypes receiving a score of 0, 1, and 2, respectively.
Linear regressions for TL vs. number of effect alleles for each SNP (unadjusted), or multiple regressions controlling for demographic and clinical variables (age, gender, HIV, and smoking pack-years) were performed to obtain adjusted beta coefficients for each SNP. The weighted score of any specific SNP for each sample was determined by multiplying the number of effect alleles (0, 1, or 2) that the sample contained for a given SNP by beta coefficients. The weighted genetic sum scores were determined using the equation below, as described previously [14].
Weighted genetic sum score = ∑i = nβiSNPi,
where n is the number of effect allele and βi is the beta efficiency for the specific SNPi.
Statistical analysis
For the unweighted analyses for each individual SNP, linear regressions for TL vs. number of effect alleles for each SNP (unadjusted) and linear regressions for each SNP, controlling for demographic and clinical variables (age, gender, HIV, and smoking pack-years) (adjusted) were performed. This procedure was repeated with the unweighted genetic sum score in a patient.
For the weighted analyses, linear regressions for TL vs. weighted score for each SNP (unadjusted) and linear regressions for weighted score for each SNP, controlling for demographic and clinical variables (age, gender, HIV, and smoking pack-years) (adjusted) were performed. This procedure was repeated with the weighted genetic sum score in a patient.
Multivariable linear regression analyses, adjusting for age, gender, and smoking pack-years, with TL vs. weighted score for each SNP and the genetic sum score, stratified by HIV or TB status, were also performed.
Results
Study participants
In total, 439 adults with cough who were evaluated for suspected TB at Mulago Hospital in Kampala, Uganda were genotyped for the six SNPs, and 434 (99%) had sufficient genomic DNA for TL measurements. The cohort consisted of 222 (51.2%) PLHIV and 212 (48.8%) persons who were HIV negative (Table 1). The median CD4+ T-cell count of the PLHIV was 118 cells/μL and 87 (39.2%) of these HIV-positive participants were receiving ART at the time of enrollment. All subjects were of African ancestry. Overall, demographic and clinical characteristics were similar between HIV-positive and HIV-negative participants except for a greater proportion of HIV-negative participants were men compared with HIV-positive participants (Table 1).
Out of the total cohort, 181 (41.7%) are TB positive and 253 (58.3%) participants are TB negative. One hundred (45.0%) of the HIV-positive participants are TB positive and 81 (38.2%) of the HIV-negative participants are TB positive. The percentages of TB-positive participants are not different between PLHIV vs. HIV-negative participants (p = 0.17).
Phenotypically measured telomere length is shorter in HIV+ patients
TL measured in leukocytes was reported to be shorter in HIV+ patients [25, 26]. We previously showed that in Ugandan with suspected TB, TL is shorter in HIV+ patients compared with HIV− participants and shortened telomeres are not associated with TB [22]. In this cohort, we confirmed our previous finding that TB is not associated with a difference in TL in univariate analysis and HIV+ is independently associated with shorter TL in multivariate analysis after adjusting for age, current smoking, pack-years, and asthma (Supplemental Table 1).
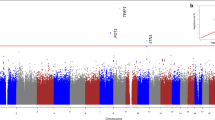
Prevalence rates of SNP genotypes
Duplicate samples matched in genotype consistency and all genotypes adhered to Hardy–Weinberg equilibrium (TERC p = 0.90, TERT p = 0.76, NAF1 p = 0.56, OBFC1 p = 0.32, ZNF208 p = 0.61, and RTEL1 p = 0.92) (Table 2). Comparing the frequencies of the alleles associated with longer TL with those found in the European population from the 1000 Genomes Project (http://www.internationalgenome.org/), we observed that for all but one locus, TERT (rs2736100), alleles associated with longer LTL are at higher frequency in our African population (Fig. 1). The frequency shifts in this cohort support prior findings comparing the allele frequencies between Europeans and Africans and are consistent with the findings that measured TL in Africans is longer than Europeans [18].
OBFC1 and total genetic sum scores are associated with LTL in the Ugandan population
We first analyzed the association between measured TL and each of the genetic variants, first on its own (i.e., unadjusted), then adjusted for age, gender, HIV status, and smoking pack-years as these demographic and clinical factors affect TL. Examined individually, only one SNP was associated with a significant effect on LTL, with the allele A of OBFC1 (rs9420907) variant associated with shorter LTL in unadjusted (β = −0.04, p = 0.024) and adjusted (β = −0.04, p = 0.017) analyses (Table 3).
The relative small cohort size suggests that it is possible that the study is underpowered to detect a statistically significant difference between different genotypes of each individual SNP. Genetic sum scores that combined the SNPs have been used as instrument variables in Mendelian randomization studies to examine the potential causal relationship between TL and disease risks [12, 17, 27, 28], we therefore constructed a genetic sum score that combined the effects of all six (below).
Since the effect size of each SNP on TL is different, we constructed a weighted genetic sum score, taking into consideration the different effect sizes as shown in Table 3, using an approach previously described by Machiela et al. [14]. As we did for the analyses of the individual SNPs, we examined the weighted genetic sum score both unadjusted (on its own) and adjusted for age, gender, HIV, and smoking pack-years. The weighted genetic sum score is associated with shorter TL in both the unadjusted (β = −0.004, p = 0.008) and adjusted (β = −0.004, p = 0.002) models (Table 4).
Effect of HIV and TB on the association between allele score with LTL
Since HIV is associated with shorter TL, as secondary analyses, we performed demographically adjusted analyses stratified by HIV status (HIV positive or negative) (Table 5). The total weighted genetic sum score showed a significant association in both PLHIV (β = −0.005, p = 0.01) and participants without HIV (β = −0.004, p = 0.047) in multivariable analysis adjusting for age, gender, and smoking pack-years (Table 5).
As a significant proportion of the 434 participants (41.7%) are TB positive, we further analyzed the data based on the TB status of the participants. In TB-negative participants, we found that weighted genetic sum score was significantly associated with LTL (β = −0.006, p = 0.001 adjusted for age, gender, and smoking pack-years) (Table 6). However, we did not observe these associations in TB-positive participants (Table 6).
Discussion
The discovery of a panel of SNPs associated with LTL [12] and the Mendelian randomization studies that established a direct cause-effect relationship between LTL and many common diseases [17] suggest that TL and its genetic determinants are important biomarkers, as well as drivers of human diseases. Current knowledge of these associations is limited to the European populations, with only a handful reported in the Chinese population [14, 29]. In this study, we found that individuals with the A allele of the telomere-related SNP OBFC1, as well as the total score of six SNPs previously reported in the European population, have significantly shorter TL (both unadjusted and adjusted for age, sex, HIV status, and smoking pack-years) in a Ugandan cohort. Ours is the first study that investigated the relationship between the previously established panel of SNPs and LTL in African populations.
A recent study examining European, African, and African American LTLs found that LTL is significantly longer in Africans than in both Europeans and African Americans [18]. These shifts in allele frequency between Europe and Africa do not fit the pattern expected by neutral genetic drift, which suggest that differences in LTL within Europeans and Africans might explain ethnic differences in risks for diseases that are associated to LTL. It is implied that shorter LTL is selected for in Europeans to decrease risk of melanoma in light-skinned individuals [18] because many of the SNPs were found previously to be associated with increased melanoma risk among Europeans [30]. We compared our allele frequency with those of the European descent from the 1000 Genomes database and observed that for all but one locus, allele frequencies associated with a longer LTL are at higher frequency in Africans compared with European populations. Our findings are consistent with the results in the above study.
Previous studies, including a prior study from this cohort, have demonstrated an association between HIV infection and shortened TL in leukocytes [7, 22, 31, 32]. Despite the impact of HIV, when we stratified by HIV status, we still found that the weighted genetic sum score is associated with measured TL in both PLHIV and HIV-negative subgroups. The analysis stratified by TB status paints a different picture. Little is known about whether TB is associated with a change in TL. Our previous study on 184 adults admitted to Mulago Hospital in Kampala, Uganda with suspected TB did not find an association with TB status and TL [7, 22, 31, 32]. Univariable analysis of TB status and measured TL in this cohort also did not show an association (Supplemental Table 1). In the current analysis, the genetic sum score is associated with TL in the TB-negative group, but not in the TB-positive group, suggesting that TB infection modifies the relationship such that the effects of these SNPs are masked in the TB-positive participants. The role and mechanism of how TB affects genetically determined telomere and phenotypically measured LTL need to be further explored. One potential mechanism could be the altered cell compositions in the PBMCs from TB-negative vs. TB-positive participants. TB is known to impact both T and B cells, major cell types in total PBMCs [33, 34]. As TL is different in these cell types and with varying differentiation stages [23, 35], differences in PBMC cell compositions between the TB-negative vs. TB-positive participants can potentially contribute to differences in phenotypically measured TL, which might cofound the relationship between TL SNP and measured PBMC TL. Prior studies that examined the associations of TL SNPs and LTL have also used diseased populations [5, 36,37,38], but have adjusted for the status of the disease in their statistical analysis model. Our finding that the association of the genetic sum score for TL and measured LTL remains in PLHIV participants, but not in TB-positive participants suggest that these two diseases impact this association differently. Measurement of TL in individual cell types, instead of PBMCs, in both PLHIV and TB-positive participants, may help clarify this issue. Future studies that utilize TL SNPs as instrument variables for LTL need to assess the impact of specific disease on this association and the potential confounding effect from the disease.
Our study has several limitations. First, this study has a relatively small sample size, given the small effect size of each SNP. Other reported studies have cohorts of much larger size than ours [5, 12, 14, 29]. We therefore performed the analysis without correcting for multiple analysis, as was done in a previous study [39]. The goal here is to look for promising trends rather than draw final conclusions. Further, about 50% of the participants are PLHIV and about 40% of them are TB positive. Although OBFC1 and the genetic sum score are associated with TL in the total cohort, stratified analysis showed that while this relationship remains in both the PLHIV and HIV-negative subgroups, and the TB-negative subgroup, the genetic sum score is not associated with LTL in the TB-positive subgroup. Although we adjusted for TB status in the analysis, it is that possible residual confounding effects of TB infection still exist. Therefore, the results from this specific cohort cannot be applied to the general African population without further investigation. Finally, our study does not have information on the prevalence of malaria in these participants, with is often associated with HIV infection. Future studies with a larger sample size, in a population without the confounding factors from HIV and TB infections are needed to further validate the findings.
In summary, this study found that the OBFC1 (rs9420907) SNP as well as the genetic sum score of six TL associated SNPs previously reported in Caucasians to be also associated with shorter TL in this Ugandan (African) cohort. This novel finding will facilitate future studies using TL as a biomarker for disease risk in African populations.
References
Pfeiffer V, Lingner J. Replication of telomeres and the regulation of telomerase. Cold Spring Harb Perspect Biol. 2013;5:a010405.
Blackburn EH. Telomeres and telomerase. Keio J Med. 2000;49:59–65.
Blackburn EH. Telomeres and telomerase: their mechanisms of action and the effects of altering their functions. FEBS Lett. 2005;579:859–62.
Sethi I, Bhat GR, Singh V, Kumar R, Bhanwer AJ, Bamezai RN, et al. Role of telomeres and associated maintenance genes in type 2 diabetes mellitus: a review. Diabetes Res Clin Pract. 2016;122:92–100.
Maubaret CG, Salpea KD, Romanoski CE, Folkersen L, Cooper JA, Stephanou C, et al. Association of TERC and OBFC1 haplotypes with mean leukocyte telomere length and risk for coronary heart disease. PLoS ONE. 2013;8:e83122.
Cordoba-Lanus E, Cazorla-Rivero S, Espinoza-Jimenez A, de-Torres JP, Pajares MJ, Aguirre-Jaime A, et al. Telomere shortening and accelerated aging in COPD: findings from the BODE cohort. Respir Res. 2017;18:59.
Wolthers KC, Bea G, Wisman A, Otto SA, de Roda Husman AM, Schaft N, et al. T cell telomere length in HIV-1 infection: no evidence for increased CD4+ T cell turnover. Science. 1996;274:1543–7.
Sokalski KM, Chu J, Mai AY, Qiu AQ, Albert AY, Zanet DL, et al. Endocrine abnormalities in HIV-infected women are associated with peak viral load - the children and women: antiretrovirals and markers of aging (CARMA) cohort. Clin Endocrinol. 2016;84:452–62.
Haldane V, Legido-Quigley H, Chuah FLH, Sigfrid L, Murphy G, Ong SE, et al. Integrating cardiovascular diseases, hypertension, and diabetes with HIV services: a systematic review. AIDS Care. 2017;30:1–13.
Presti RM, Flores SC, Palmer BE, Atkinson JJ, Lesko CR, Lau B, et al. Mechanisms underlying HIV associated non-infectious lung disease. Chest. 2017;152:1053–60
Broer L, Codd V, Nyholt DR, Deelen J, Mangino M, Willemsen G, et al. Meta-analysis of telomere length in 19,713 subjects reveals high heritability, stronger maternal inheritance and a paternal age effect. Eur J Hum Genet. 2013;21:1163–8.
Codd V, Nelson CP, Albrecht E, Mangino M, Deelen J, Buxton JL, et al. Identification of seven loci affecting mean telomere length and their association with disease. Nat Genet. 2013;45:422–7, 27e1-2.
Ellehoj H, Bendix L, Osler M. Leucocyte telomere length and risk of cardiovascular disease in a cohort of 1,397 danish men and women. Cardiology. 2016;133:173–7.
Machiela MJ, Hsiung CA, Shu XO, Seow WJ, Wang Z, Matsuo K, et al. Genetic variants associated with longer telomere length are associated with increased lung cancer risk among never-smoking women in Asia: a report from the female lung cancer consortium in Asia. Int J Cancer. 2015;137:311–9.
Rode L, Bojesen SE, Weischer M, Vestbo J, Nordestgaard BG. Short telomere length, lung function and chronic obstructive pulmonary disease in 46,396 individuals. Thorax. 2013;68:429–35.
Rode L, Nordestgaard BG, Bojesen SE. Peripheral blood leukocyte telomere length and mortality among 64,637 individuals from the general population. J Natl Cancer Inst. 2015;107:djv074.
Telomeres Mendelian Randomization C, Haycock PC, Burgess S, Nounu A, Zheng J, Okoli GN, et al. Association between telomere length and risk of cancer and non-neoplastic diseases: a mendelian randomization study. JAMA Oncol. 2017;3:636–51.
Hansen ME, Hunt SC, Stone RC, Horvath K, Herbig U, Ranciaro A, et al. Shorter telomere length in Europeans than in Africans due to polygenetic adaptation. Hum Mol Genet. 2016;25:2324–30.
Li CY, Yu Q, Ye ZQ, Sun Y, He Q, Li XM, et al. A nonsynonymous SNP in human cytosolic sialidase in a small Asian population results in reduced enzyme activity: potential link with severe adverse reactions to oseltamivir. Cell Res. 2007;17:357–62.
Hamad R, Tuljapurkar S, Rehkopf DH. Racial and socioeconomic variation in genetic markers of telomere length: a cross-sectional study of U.S. older adults. EBioMedicine. 2016;11:296–301.
Njajou OT, Blackburn EH, Pawlikowska L, Mangino M, Damcott CM, Kwok PY, et al. A common variant in the telomerase RNA component is associated with short telomere length. PLoS ONE. 2010;5:e13048.
Auld E, Lin J, Chang E, Byanyima P, Ayakaka I, Musisi E, et al. HIV infection is associated with shortened telomere length in ugandans with suspected tuberculosis. PLoS ONE. 2016;11:e0163153.
Lin J, Epel E, Cheon J, Kroenke C, Sinclair E, Bigos M, et al. Analyses and comparisons of telomerase activity and telomere length in human T and B cells: insights for epidemiology of telomere maintenance. J Immunol Methods. 2010;352:71–80.
Cawthon RM. Telomere measurement by quantitative PCR. Nucleic Acids Res. 2002;30:e47.
Pathai S, Lawn SD, Gilbert CE, McGuinness D, McGlynn L, Weiss HA, et al. Accelerated biological ageing in HIV-infected individuals in South Africa: a case-control study. AIDS. 2013;27:2375–84.
Zanet DL, Thorne A, Singer J, Maan EJ, Sattha B, Le Campion A, et al. Association between short leukocyte telomere length and HIV infection in a cohort study: no evidence of a relationship with antiretroviral therapy. Clin Infect Dis 2014;58:1322–32.
Zhang C, Doherty JA, Burgess S, Hung RJ, Lindstrom S, Kraft P, et al. Genetic determinants of telomere length and risk of common cancers: a Mendelian randomization study. Hum Mol Genet. 2015;24:5356–66.
Zhan Y, Hagg S. Telomere length shortening in Alzheimer’s disease: procedures for a causal investigation using single nucleotide polymorphisms in a mendelian randomization study. Methods Mol Biol. 2018;1750:293–306.
Luu HN, Long J, Wen W, Zheng Y, Cai Q, Gao YT, et al. Association between genetic risk score for telomere length and risk of breast cancer. Cancer Causes Control. 2016;27:1219–28.
Iles MM, Bishop DT, Taylor JC, Hayward NK, Brossard M, Cust AE, et al. The effect on melanoma risk of genes previously associated with telomere length. J Natl Cancer Inst. 2014;106:dju267.
Effros RB, Allsopp R, Chiu CP, Hausner MA, Hirji K, Wang L, et al. Shortened telomeres in the expanded CD28-CD8+ cell subset in HIV disease implicate replicative senescence in HIV pathogenesis. AIDS. 1996;10:F17–22.
Bestilny LJ, Gill MJ, Mody CH, Riabowol KT. Accelerated replicative senescence of the peripheral immune system induced by HIV infection. AIDS. 2000;14:771–80.
Chan J, Mehta S, Bharrhan S, Chen Y, Achkar JM, Casadevall A, et al. The role of B cells and humoral immunity in Mycobacterium tuberculosis infection. Semin Immunol. 2014;26:588–600.
Jasenosky LD, Scriba TJ, Hanekom WA, Goldfeld AE. T cells and adaptive immunity to mycobacterium tuberculosis in humans. Immunol Rev. 2015;264:74–87.
Hodes RJ, Hathcock KS, Weng NP. Telomeres in T and B cells. Nat Rev Immunol. 2002;2:699–706.
Shen Q, Zhang Z, Yu L, Cao L, Zhou D, Kan M, et al. Common variants near TERC are associated with leukocyte telomere length in the Chinese Han population. Eur J Hum Genet. 2011;19:721–3.
Liu Y, Cao L, Li Z, Zhou D, Liu W, Shen Q, et al. A genome-wide association study identifies a locus on TERT for mean telomere length in Han Chinese. PLoS One. 2014;9:e85043.
Bojesen SE, Pooley KA, Johnatty SE, Beesley J, Michailidou K, Tyrer JP, et al. Multiple independent variants at the TERT locus are associated with telomere length and risks of breast and ovarian cancer. Nat Genet. 2013;45:371–84. 84e1-2
Zeiger AM, White MJ, Eng C, Oh SS, Witonsky J, Goddard PC, et al. Genetic determinants of telomere length in African American youth. Sci Rep. 2018;8:13265.
Acknowledgements
This work was supported by the National Institutes of Health (grant numbers R01 HL128156, R01 HL090335, K24 HL087713, and D43 TW009607). The funding sources played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. We wish to acknowledge the participants of this study, the hospital staff at Mulago National Referral Hospital in Kampala, Uganda, and the following individuals: Alfred Andama, Catherine Nabakiibi, Sylvia Kaswabuli, Robert Ssebunya, Dr. Irene Ayakaka, Dr. Wallen Tumwine, Priscilla Bbosa, Yusef Magezi, Josephine Zawedde, Dr. Elizabeth Blackburn, Colin Huang, Serena Fong, Stephen Stone, Elizabeth Auld, Alisa Malki, Marlena Hartman-Filson, Maggie McGing, and Mathew Sommers.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
JL is a co-founder and scientific advisor to Telomere Diagnostic Inc. The company played no role in this study. Other authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, S., Chang, E., Byanyima, P. et al. Association between common telomere length genetic variants and telomere length in an African population and impacts of HIV and TB. J Hum Genet 64, 1033–1040 (2019). https://doi.org/10.1038/s10038-019-0646-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s10038-019-0646-9
This article is cited by
-
TERT single nucleotide polymorphism rs2736098 but not rs2736100 is associated with telomere length in HIV-infected patients on cART
Molecular Biology Reports (2024)
-
Telomere length and outcome of treatment for pulmonary tuberculosis in a gold mining community
Scientific Reports (2021)



