Abstract
ORAI1 encodes a calcium channel essential in the store-operated calcium entry mechanism. A previous genetic association study identified a rare in-frame insertion variant of ORAI1 conferring Kawasaki disease (KD). To deepen our understanding of the involvement of rare variants of ORAI1 in KD pathogenesis, we investigated 3812 patients with KD and 2644 healthy individuals for variations in the protein-coding region of ORAI1. By re-sequencing the study participants’ DNA, 27 variants with minor allele frequencies (MAFs) < 0.01 that had not been examined in the previous study were identified. Although no significant association with KD was observed either in single-variant analyses or in a collapsing method analysis of the 27 variants, stratification by MAFs, variant types, and predicted deleteriousness revealed that six rare, deleterious, missense variants (MAF < 0.001, CADD C-score ≥ 20) were exclusively present in KD patients, including three refractory cases (OR = ∞, P = 0.046). The six missense variants include p.Gly98Asp, which has been demonstrated to result in gain of function leading to constitutive Ca2+ entry. Conversely, five types of frameshift variants, all identified near the N terminus and assumed to disrupt ORAI1 function, showed an opposite trend of association (OR = 0.35, P = 0.24). These findings support our hypothesis that genetic variations causing the upregulation of the Ca2+/NFAT pathway confer susceptibility to KD. Our findings also provide insights into the usefulness of stratifying the variants based on their MAFs and on the direction of the effects on protein function when conducting association studies using the gene-based collapsing method.
Similar content being viewed by others
Introduction
Kawasaki disease (KD, MIM#611775) is an acute systemic vasculitis syndrome which mainly affects children younger than 5 years of age. Due to the cardiac complication represented by coronary artery aneurysms, KD has become the leading cause of acquired heart diseases during childhood in developed countries [1, 2]. Genome-wide studies have identified several common variants associated with KD susceptibility [3,4,5]. However, the involvement of rare genetic variants, which has been recognized as one of the explanations for the “missing heritability” problem in common diseases, in KD pathogenesis has been largely uninvestigated. In 2016, we reported associations of a common single-nucleotide variant (SNV) and a rare in-frame insertion variant of the ORAI1 gene with susceptibility to KD [6]. ORAI1 is a gene that encodes a plasma membrane calcium channel essential to the store-operated calcium entry (SOCE) mechanism in immune cells [7,8,9] and skeletal muscle cells [10, 11], and is the first gene in which both common and rare variants have been associated with KD. Owing to the design of our previous study, where we identified variants by re-sequencing 94 patients with KD and evaluating their association in a larger case and control panel, it was assumed that there remained other rare variants of ORAI1 that were not examined. In this study, to deepen the understanding of the involvement of rare genetic variants in KD susceptibility and to obtain insight into the role of ORAI1 in KD pathogenesis, a large-scale genetic association study was conducted.
Materials and methods
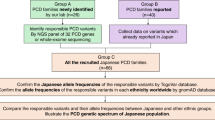
The flow of this study is demonstrated in Fig. 1.
Samples
First, 2434 KD samples were collected at several cooperating medical institutes in Japan, and 1378 KD samples were obtained from the Japan Kawasaki Disease Genome Consortium, which comprises 49 participating medical institutes/hospitals.
The control samples were all from adult individuals without a history of KD and were collected at Keio University (n = 374) or obtained from the Midosuji Rotary Club (n = 940) and Health Science Research Resources Bank, Osaka (n = 1330).
Ethics
The ethical committees or institutional review boards at RIKEN, Chiba University, and all medical institutes that contributed to the patient samples approved the study. Written informed consent was given by all participants. Since KD is a childhood disease and the patients were infants or children at the time of enrollment, in most cases, written informed consent was obtained from the patients’ parents. When the patients were 16 to 20 years old, we received written informed consent from both the patients themselves and their parents.
Direct sequencing
Protein-coding regions of the ORAI1 gene distributed in exons 1 (303 bp) and 2 (600 bp) were re-sequenced by a PCR direct sequencing method. For exon 1, PCR primers were also used for direct sequencing, while for exon 2, primers for sequencing were additionally designed. The sequencing reactions were performed using the BigDyeTM Terminator v3.1 Cycle Sequencing Kit (Thermo Fisher Scientific), and sequencing was carried out by an ABI 3770xL or ABI 3130xL sequencer (Applied Biosystems). Variants were identified on the SEQUENCHER V4 software (HITACHI). Primer sequences for PCR and direct sequencing were demonstrated, and PCR conditions are summarized in Supplementary Figure 1.
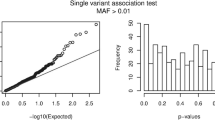
Association analyses
Lack of statistical power is a major obstacle in performing association studies of rare variants when the number of subjects is not sufficiently large. Combining information of multiple rare variants to evaluate the effect as a single variant is one method to overcome this problem [12]. We applied the collapsing method to variants for which ≥0.75 of statistical power was not expected to detect association with P < 0.05 under the assumption of the odds ratio of 3.0. Association of the individual, as well as collapsed multiple variants with KD, were assessed by Fisher’s exact test using the R 3.4.0 statistical computing environment. P values < 0.05 were considered significant.
In silico prediction of deleteriousness of the identified variants
Predictions of the deleteriousness of the ORAI1 variants identified in this study were carried out using the Combined Annotation Dependent Depletion (CADD) tool [13]. The prediction score (C-score) of 20 corresponded to the top 1% of harmfulness when evaluating all known single-base substitutions, and was set as the threshold for creating a stratified variants subgroup for collapsing.
Results
Chromosomal locations, nucleotide and protein changes, the allele frequencies in cases of KD and controls, and the protein domains together with the CADD C-scores of the identified 34 variants, including 11 novel ones, are summarized in Table 1. These include all of the known five common variants (rs3741595, rs3741596, rs3741597, rs3825174, and rs3825175) as well as two rare variants (rs141919534 and c.59G>C) that have already been identified in our previous study [6]. The 27 variants that have never been evaluated for their association with KD include 12 missense (44%), 9 synonymous (33%), 5 frameshift (19%), and 1 in-frame insertion (4%) variant, and all of them had minor allele frequencies (MAFs) < 0.01 in the subjects in this study (Table 1). The position of these rare variants on the ORAI1 protein domains and the number of subjects presenting each variant are shown in Fig. 2. All of the alternative alleles of insertion or deletion variants were determined by sequencing of the PCR amplicons cloned into plasmids (data not shown).
ORAI1 protein domains and variants identified in this study. Positions and amino acid substitutions of the 27 ORAI1 variants identified in this study on the protein domains are shown. Two previously identified rare variants (p.Pro45_Pro46insProPro4 and p.Gly20Ala) are also shown. For each modification, the number of individuals with the variant in the 3812 cases of Kawasaki disease and 2644 controls is provided between parentheses. The black, red, and purple letters indicate synonymous, missense, and deletion/insertion variants, respectively. Variants with a Combined Annotation Dependent Depletion (CADD) C-score ≥ 20 (5 frameshift and 8 missense variants) are indicated in boldface (color figure online)
Of the 27 variants, 4 (c.12G>T, c.264C>G, c.397G>A, and c.889G>A) had relatively high allele frequencies (MAF > 0.001) in the controls, and the others were so rare that only up to three minor alleles were observed in the entire sample sets. None of the four relatively common variants showed significant association with KD (data not shown). When all 27 variants and the variants stratified based on their MAFs (>0.001 or <0.001) were evaluated as a single variant by the collapsing method, none of them had a significant association (Table 2).
Next, the variants were further stratified based on their deleteriousness using the CADD prediction score (C-score). Of the 23 variants with MAFs < 0.001, 11 had higher C-scores ≥ 20 and included 6 missense and 5 frameshift variants. The six deleterious missense variants were exclusively identified in patients with KD (odds ratio (OR) = ∞, P = 0.046). The clinical features of the six KD patients is summarized in Table 3. Three of the six were refractory cases who did not respond to at least two rounds of the standard intravenous immunoglobulin (IVIG) treatment (2 g/kg) and required additional therapies. The three included two patients who had medium-sized to giant coronary artery aneurysms as cardiac complications. Although not significant, the five frameshift variants showed a negative trend of association (OR = 0.35, P = 0.24).
Discussion
ORAI1, as part of the SOCE mechanism, plays an essential role in T-cell activity. Homozygous loss of functional ORAI1 alleles causes an autosomal recessive immune deficiency syndrome [9]. ORAI1 is also expressed in hematopoietic cells including B cells [14], dendritic cells [15], neutrophils [16], natural killer cells [17], platelets [18], and mast cells [19]. In our recent study, one common non-synonymous variant (rs3741596) and a rare 6-bp insertion/deletion variant (rs141919534) were associated with KD [6]. Based on previous studies on Ca2+/nuclear factor of activated T-cells (NFAT) pathway upregulation by susceptibility variants of ITPKC and CASP3, in addition to successful clinical studies on cyclosporine A, which is an immunosuppressant targeting this pathway for KD [4, 5, 20,21,22], the two above-mentioned variants were hypothesized to upregulate ORAI1 channel function. In this study, by selecting variants for collapsing according to their MAFs, types, and predicted deleteriousness, we observed a significant association in six rare deleterious missense SNVs with KD. Although conclusions should be carefully drawn because of a lack of exact information on the directions and sizes of the effects due to individual variants, the results in this study further support our hypothesis that genetic variants leading to Ca2+/NFAT pathway upregulation may confer susceptibility to KD. The idea was based on the following two studies. First, we obtained the information showing that one of the six rare and deleterious missense variants has a significant gain-of-function effect [23]. The p.Gly98Asp mutation was located within the first transmembrane region of the protein, where amino acids were well conserved throughout the species (Supplementary Figure 2). The Gly98 of ORAI1 is a key amino acid that acts as a gating hinge for channel opening and closing, and the change from glycine (neutral and hydrophobic) to aspartate (acidic and hydrophilic) is known to result in constitutive Ca2+ permeability independently of STIM1 [23, 24]. Second, the five frameshift variants, which tended to be negatively associated with KD, were collectively identified in the N-terminal cytoplasmic region (Supplementary Figure 3). None of the four transmembrane regions of ORAI1, all located downstream of the frameshift-initiating points on the variant proteins, would be properly translated because of the incorrect reading frames. Thus, the truncated ORAI1 proteins, which had the correct amino acid sequence of ORAI1 only in the N-terminal cytoplasmic region and lacked the membrane protein properties, would not be expressed on the plasma membrane (Supplementary Figure 4), and could not engage in ion conduction. Therefore, the two types of variants, which were supposed to have at least partly different functional effects on ORAI1 protein function, had the opposite directions of association with KD, and thereby provided an insight into the role of ORAI1 variants in KD pathogenesis. Of the six KD patients with the rare deleterious missense variants, three were refractory cases requiring repeated IVIG administration and other treatment options. In particular, an early-onset case, who was affected at 2 months of age, suffered from extremely severe KD. The patient developed giant coronary aneurysms in three coronary artery branches and had an acute myocardial infarction by occlusion of the right coronary artery on day 34 of illness (Table 3). Considering the low frequencies of the deleterious alleles, the usefulness of sequencing the ORAI1 gene at the bedside of acute KD patients seems to be limited. However, the accumulation of knowledge about the functional significance of the rare variants, their association with KD, as well as the severer manifestations and the degrees of genetic penetrance will pave the way for genetic counseling or testing of the relatives of the variant carriers.
In contrast to the six rare and deleterious missense variants exclusively observed in patients with KD, frameshift variants were observed in patients with KD as well as in controls. Loss-of-function mutations of ORAI1 have been known to cause an autosomal recessive congenital immune deficiency syndrome (IMD9; MIM #61782) [9]. In the familial case of IMD9, both parents of the patients, who were heterozygous for the causal mutation and in whose T cells SOCE was partially impaired, were immunologically normal. Furthermore, it is also known that some gain-of-function mutations of ORAI1 cause an autosomal dominant tubular aggregate myopathy (TAM2; MIM #615883) [25]. Three independent patients with TAM2 due to a p.Gly98Ser of ORAI1 have been reported [26, 27]. In in vitro experiments using exogenously expressed ORAI1 mutant proteins, both p.Gly98Ser and p.Gly98Asp similarly lead to a constitutive activation of the channel [23, 27]. Given that five other rare deleterious missense variants also have a gain-of-function effect on ORAI1 function, and some dominant effects, it was reasonable for the control population to lack these types of variants. The different distribution patterns of these stratified variants in the study populations might reflect the difference in impact of the variants on the cellular activity as well as on the phenotype that individuals with the variants would have. It has been reported that ORAI1 has two isoforms, ORAI1α with 303 amino acids translated from the first methionine, and ORAI1β, a shorter isoform that uses the second (64th position) or the third (71st position) methionine residue as a translation initiation codon [28]. The impact of the five frameshift variants in this study might be milder than expected, because the shorter isoform that also supports SOCE can be translated from all alternative alleles of these variants.
Collapsing the rare variants has been recognized to be effective in assessing the association of rare genetic variants [29]. Usually, common variants are not included in the collapsing analysis because their high allele frequencies in cases or controls, whether they are associated with the trait of interest or not, may interfere with the detection of the association of other rare variants. In this study, we found it useful to further stratify the rare variants by their MAFs. The MAFs of the rare variants in the controls in this study vary from 0.00617 for c.12G>T, with 53 and 32 alternative alleles seen in the cases of KD and controls, respectively, to 0.0 for multiple variants observed only in a single or few patients with KD. There is a well-recognized model of the relationship between the risk allele frequencies and the strength of the genetic effect, in which the smaller allele frequencies of the risk-associated variants result in a larger effect size [30, 31]. In this context, it seemed reasonable to evaluate the association of rare variants by the collapsing method after stratifying them by their MAFs. In contrast to the lack of difference in the alternative allele frequencies when the 27 rare variants were collapsed without stratification (OR = 0.98, P = 0.87), 23 variants with MAFs < 0.001 showed a positive trend of association (OR = 1.84, P = 0.19).
The opposite trends of association in both missense and frameshift variants were indicative of the potential importance of stratifying rare variants in association studies, according to their magnitude and the direction of their effects on the protein function. Currently, there are a number of computer tools to predict the deleteriousness of genetic variants. The results of stratifying the nine rare (MAF < 0.001) missense variants were inconsistent among the commonly used prediction tools, including Polyphen-2, SIFT, and Mutation Taster [32] (Supplementary Table 1). In this study, we used CADD, recognizing an advantage of the tool in performing the prediction by integrating multiple prediction results and scores, including those from SIFT and PolyPhen-2. The option to evaluate synonymous SNVs and deletion/insertion variants was another reason for selecting CADD. However, the items utilized to calculate the C-scores during deleteriousness evaluations of known causal variants of TAM2 (gain of function) [26, 27, 33, 34] and IMD9 (loss of function) [35,36,37,38] with CADD did not seem to be suited to discriminating the two variant categories. This resulted in difficulty in precisely inferring the direction of the variant effects by in silico tools (Supplementary Table 2). At present, determining the true functional effect of each variant by functional assays with Ca2+ imaging or patch-clamp techniques using the variant carriers’ lymphocytes, or cultured cell lines transduced with the variant channels, is the most suitable and reliable method of stratifying the variants for efficient association studies.
In this study, six insertion/deletion variants were newly identified. Because all of them were located within the N-terminal cytoplasmic region, this domain might be a hot spot for these types of variants (Supplementary Figure 3). One of these variants was a novel insertion of 37 bases (c.125_126ins), which was identical to the upstream sequence from the inserted position. In ClinVar, two other insertion variants of 37 bases in similar positions of ORAI1 (c.126_127insCCGCCGCCGCAGCGGGGACGGGGAGCCCCCGGGGGCC; Variation ID: 594718, and c.141_142insCCGCCGCCGCAGCGGGGACGGGGAGCCCCCGGGGGCC; Variation ID: 470188) had been registered. Although these three variants were not identical, the high similarity of the inserted sequences (Supplementary Figure 5) suggests some common mechanism in the generation of the variants.
Previously, we reported a positive association of a six-base insertion variant of ORAI1 (rs141919534; p.Pro45_Pro46insProPro) with KD. Interestingly, another novel in-frame insertion variant (p.Arg32_Arg33insSerArgArg), identified within the same cytoplasmic region, was observed in three patients with KD but not in controls. Within the cytoplasmic region, there is a domain for interactions with STIM1 (Supplementary Figure 3). The similar association trend observed for these two in-frame insertion variants within the N-terminal cytoplasmic region may reflect the modulated interaction between ORAI1 and STIM1 due to the elongation of this domain and the subsequent increase in Ca2+ influx or the duration of the channel opening.
There are several limitations to this study. First, the exact impacts of the rare and deleterious missense variants were not evaluated by biological assays and the prediction of deleteriousness was carried out with a single tool. Second, the frequencies of the deleterious missense variants identified in this study were so low that the findings cannot be immediately applied in clinical diagnosis, even when the gain-of-function effect was proven for all six variants. Finally, a correction of multiple testing was not conducted.
In conclusion, we observed that ORAI1 deleterious missense variants with MAFs < 0.001, including one known gain-of-function mutation in the first transmembrane region, had a positive association with KD in a collapsing method analysis. Although it was not significant, an in-frame insertion variant in the N-terminal cytoplasmic region showed the same association trend as the other in-frame insertion variant within the same protein domain that had been identified in our previous study [6]. Conversely, five frameshift variants causing N-terminal protein truncation showed the opposite trend of association. These observations support our hypothesis that genetic variants leading to upregulation of the Ca2+/NFAT pathway confer susceptibility to KD. The usefulness of the collapsing method in evaluating the association of mutations and rare variations with diseases may be enhanced when MAFs and variant types are taken into account. Currently, there is no in silico tool that can predict the direction of the variants’ effect on the protein function. Future advances in the precise prediction of the functional impact of the identified variants (i.e., neutral, gain of function, or loss of function) may facilitate the assessment of their association with diseases.
Change history
31 July 2019
An amendment to this paper has been published and can be accessed via a link at the top of the paper
References
Kawasaki T. Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Arerugi. 1967;16:178–222.
Burns JC. Commentary: translation of Dr. Tomisaku Kawasaki’s original report of fifty patients in 1967. Pediatr Infect Dis J. 2002;21:993–5.
Onouchi Y, Tamari M, Takahashi A, Tsunoda T, Yashiro M, Nakamura Y, et al. A genome-wide linkage analysis of Kawasaki disease: evidence for linkage to chromosome 12. J Hum Genet. 2007;52:179–90.
Onouchi Y, Gunji T, Burns JC, Shimizu C, Newburger JW, Yashiro M, et al. ITPKC functional polymorphism associated with Kawasaki disease susceptibility and formation of coronary artery aneurysms. Nat Genet. 2008;40:35–42.
Onouchi Y, Ozaki K, Burns JC, Shimizu C, Hamada H, Honda T, et al. Common variants in CASP3 confer susceptibility to Kawasaki disease. Hum Mol Genet. 2010;19:2898–906.
Onouchi Y, Fukazawa R, Yamamura K, Suzuki H, Kakimoto N, Suenaga T, et al. Variations in ORAI1 gene associated with Kawasaki disease. PLoS One. 2016;11:e0145486.
Prakriya M, Feske S, Gwack Y, Srikanth S, Rao A, Hogan PG. ORAI1 is an essential pore subunit of the CRAC channel. Nature. 2006;443:230–3.
Vig M, Peinelt C, Beck A, Koomoa DL, Rabah D, Koblan-Huberson M, et al. CRACM1 is a plasma membrane protein essential for store-operated Ca2+ entry. Science. 2006;312:1220–3.
Feske S, Gwack Y, Prakriya M, Srikanth S, Puppel SH, Tanasa B, et al. A mutation in Orai1 causes immune deficiency by abrogating CRAC channel function. Nature. 2006;441:179–85.
Trebak M, Zhang W, Ruhle B, Henkel MM, González-Cobos JC, Motiani RK, et al. What role for store-operated Ca2+ entry in muscle? Microcirculation. 2013;20:330–6.
Kurebayashi N, Ogawa Y. Depletion of Ca2+ in the sarcoplasmic reticulum stimulates Ca2+ entry into mouse skeletal muscle fibres. J Physiol. 2001;533:185–99.
Sung YJ, Korthauer KD, Swartz MD, Engleman CD. Methods for collapsing multiple rare variants in whole-genome sequence data. Genet Epidemiol. 2014;38:13–20.
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet. 2014;46:310–5.
Baba Y, Kurosaki T. Impact of Ca2+ signaling on B cell function. Trends Immunol. 2011;32:589–94.
Félix R, Crottès D, Delalande A, Fauconnier J, Lebranchu Y, Le Guennec JY, et al. The Orai-1 and STIM-1 complex controls human dendritic cell maturation. PLoS One. 2013;8:e61595.
Steinckwich N, Schenten V, Melchior C, Bréchard S, Tschirhart EJ. An essential role of STIM1, Orai1, and S100A8-A9 proteins for Ca2+ signaling and FcγR-mediated phagosomal oxidative activity. J Immunol. 2011;186:2182–91.
Maul-Pavicic A, Chiang SC, Rensing-Ehl A, Jessen B, Fauriat C, Wood SM, et al. ORAI1-mediated calcium influx is required for human cytotoxic lymphocyte degranulation and target cell lysis. Proc Natl Acad Sci USA. 2011;108:3324–9.
Tolhurst G, Carter RN, Amisten S, Holdich JP, Erlinge D, Mahaut-Smith MP. Expression profiling and electrophysiological studies suggest a major role for Orai1 in the store-operated Ca2+ influx pathway of platelets and megakaryocytes. Platelets. 2008;19:308–13.
Baba Y, Nishida K, Fujii Y, Hirano T, Hikida M, Kurosaki T. Essential function for the calcium sensor STIM1 in mast cell activation and anaphylactic responses. Nat Immunol. 2008;9:81–8.
Onouchi Y, Suzuki Y, Suzuki H, Terai M, Yasukawa K, Hamada H, et al. ITPKC and CASP3 polymorphisms and risks for IVIG unresponsiveness and coronary artery lesion formation in Kawasaki disease. Pharm J. 2013;13:52–9.
Suzuki H, Terai M, Hamada H, Honda T, Suenaga T, Takeuchi T, et al. Cyclosporin A treatment for Kawasaki disease refractory to initial and additional intravenous immunoglobulin. Pediatr Infect Dis J. 2011;10:871–6.
Aoyagi R, Hamada H, Sato Y, Suzuki H, Onouchi Y, Ebata R, et al. Study protocol for a phase III multicentre, randomised, open-label, blinded-end point trial to evaluate the efficacy and safety of immunoglobulin plus cyclosporin A in patients with severe Kawasaki disease (KAICA Trial). BMJ Open. 2015;5:e009562.
Zhang SL, Yeromin AV, Hu J, Amcheslavsky A, Zheng H, Cahalan MD. Mutations in Orai1 transmembrane segment 1 cause STIM1-independent activation of Orai1 channels at glycine98 and channel closure at arginine91. Proc Natl Acad Sci USA. 2011;108:17838–43.
Zheng H, Zhou M-H, Hu C, Kuo E, Peng X, Hu J, et al. Differential roles of the C and N termini of Orai1 protein in interacting with stromal interaction molecule 1 (STIM1) for Ca2+ release-activated Ca2+ (CRAC) channel activation. J Biol Chem. 2013;288:11263–72.
Shahrizaila N, Lowe J, Wills A. Familial myopathy with tubular aggregates associated with abnormal pupils. Neurology. 2004;63:1111–3.
Endo Y, Noguchi S, Hara Y, Hayashi YK, Motomura K, Miyatake S, et al. Dominant mutations in ORAI1 cause tubular aggregate myopathy with hypocalcemia via constitutive activation of store-operated Ca2+ channels. Hum Mol Genet. 2015;24:637–48.
Boehm J, Bulla M, Urquhart JE, Malfatti E, Williams SG, Sullivan JO, et al. ORAI1 mutations with distinct channel gating defects in tubular aggregate myopathy. Hum Mutat. 2017;38:426–38.
Fukushima M, Tomita T, Janoshazi A, Putney JW. Alternative translation initiation gives rise to two isoforms of Orai1 with distinct plasma membrane mobilities. J Cell Sci. 2012;125:4354–61.
Li B, Leal SM. Methods for detecting associations with rare variants for common diseases: application to analysis of sequence data. Am J Hum Genet. 2008;83:311–21.
McCarthy MI, Abecasis GR, Cardon LR, Goldstein DB, Little J, Ioannidis JP, et al. Genome-wide association studies for complex traits: consensus, uncertainty and challenges. Nat Rev Genet. 2008;9:356–69.
Manolio TA, Collins FS, Cox NJ, Goldstein DB, Hindorff LA, Hunter DJ, et al. Finding the missing heritability of complex diseases. Nature. 2009;461:747–53.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Garibaldi M, Fattori F, Riva B, Labasse C, Brochier G, Ottaviani P, et al. A novel gain-of-function mutation in ORAI1 causes late-onset tubular aggregate myopathy and congenital miosis. Clin Genet. 2017;91:780–86.
Nesin V, Wiley G, Kousi M, Ong EC, Lehmann T, Nicholl DJ, et al. Activating mutations in STIM1 and ORAI1 cause overlapping syndromes of tubular myopathy and congenital miosis. Proc Natl Acad Sci USA. 2014;111:4197–202.
McCarl CA, Picard C, Khalil S, Kawasaki T, Rother J, Papolos A, et al. ORAI1 deficiency and lack of store-operated Ca2+ entry cause immunodeficiency, myopathy, and ectodermal dysplasia. J Allergy Clin Immunol. 2009;124:1311–8.
Chou J, Badran YR, Yee CSK, Bainter W, Ohsumi TK, Al-Hammadi S, et al. A novel mutation in ORAI1 presenting with combined immunodeficiency and residual T-cell function. J Allergy Clin Immunol. 2015;136:479–82.
Badran YR, Massaad MJ, Bainter W, Cangemi B, Naseem SU, Javad H, et al. Combined immunodeficiency due to a homozygous mutation in ORAI1 that deletes the C-terminus that interacts with STIM1. Clin Immunol. 2016;166–7:100–2.
Lian J, Cuk M, Kahlfuss S, Kozhaya L, Vaeth M, Rieux-Laucat F, et al. ORAI1 mutations abolishing store-operated Ca2+ entry cause anhidrotic ectodermal dysplasia with immunodeficiency. J Allergy Clin Immunol. 2018;142:1297–310.
den Dunnen JT, Antonarakis SE. Mutation nomenclature extensions and suggestions to describe complex mutations: a discussion. Hum Mutat. 2000;15:7–12.
Acknowledgements
This study was supported by grants from the Millennium Project, Japan Kawasaki Disease Research Center (2009 to YO), the Ministry of Education, Culture, Sports, and Technology (25293139 to YO), the Ministry of Health, Labour and Welfare (0401040 to AH), and the Japan Agency for Medical Research and Development (JP17ek0410039 to TH). We are grateful to the participants in this study and the medical staff caring for the patients. We also thank Ms. Yoshie Kikuchi for her technical assistance.
Japan Kawasaki Disease Genome Consortium
Hiroshi Masuda7, Tohru Kobayashi7, Toshiaki Jibiki8, Taro Yamazaki9, Yoshiaki Ohkuma10, Maya Fujiwara11, Tomio Kobayashi12, Harumitsu Takeuchi13, Kazunobu Ouchi14, Yumi Mizuno15, Shigeto Fuse16, Nobuhiro Fukazawa17, Tsutomu Saji18, Shinichi Takatsuki18, Kenichiro Nishimura19, Hiromichi Hamada20, Ryuji Fukazawa21, Hideko Nishumura22, Kentaro Aso23, Tomoyo Matsubara24, Takahisa Mizuno25, Satoru Iwashima26, Mamoru Ayusawa27, Kazuyuki Ikeda28, Takashi Kosuda29, Kunio Hashimoto30, Kunio Hirasawa31, Masaru Miura32, Junpei Somura33, Emi Toba34, Keiichi Hirono35, Yuichi Nomura36, Hirokazu Arakawa37, Shouhei Ogata38, Hiroki Kajino39, Seiji Kawamura40, Hayato Aoyagi41, Hiroshi Suzuki42, Kouta Ichinose43, Ayako Shimozono44, Yoshiaki Kato45, Masamune Higashikawa46, Youichi Kawamura47, Masahiro Misawa48, Noriko Nagai49, Taichi Kato50, Dan Nagata51, Akiko Okamoto52, Hiroyuki Suzuki53, Masahiko Kishiro54, Junko Shiono55, Kouji Higashi56, Naoki Yokoyama57, Ryota Ebata58, Yoshihiro Onouchi59.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Japan Kawasaki Disease Genome Consortium are listed in Acknowledgements.
Rights and permissions
About this article
Cite this article
Thiha, K., Mashimo, Y., Suzuki, H. et al. Investigation of novel variations of ORAI1 gene and their association with Kawasaki disease. J Hum Genet 64, 511–519 (2019). https://doi.org/10.1038/s10038-019-0588-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s10038-019-0588-2
This article is cited by
-
Circulating CD3+HLA-DR+ Extracellular Vesicles Are Not Increased in the Acute Phase of Kawasaki Disease
SN Comprehensive Clinical Medicine (2020)
-
Immunogenetics of Kawasaki disease
Clinical Reviews in Allergy & Immunology (2020)