Abstract
Aminoglycosides are potent antibiotics which are used to treat severe gram-negative infections, neonatal sepsis, and multidrug-resistant tuberculosis. Ototoxicity is a well-known side effect of aminoglycosides, and a rapid, profound, and irreversible hearing loss can occur in predisposed individuals. MT-RNR1 gene encoding the mitochondrial ribosomal 12S subunit is a hot spot for aminoglycoside-induced hearing loss mutations, however, a variability in the nature and frequency of genetic changes in different populations exists. The objective of this study was to analyze MT-RNR1 gene mutations in a Baltic-speaking Latvian population, and to estimate the prevalence of such genetic changes in the population-specific mitochondrial haplogroups. In the cohort of 191 ethnic non-related Latvians, the presence of two deafness-associated mutations, m.1555A>G and m.827A>G, three potentially pathogenic variations, m.961insC(n), m.961T>G and m.951G>A, and one unknown substitution, m961T>A was detected, and the aggregate frequency of all variants was 7.3%. All genetic changes were detected in samples belonged to the haplogroups H, U, T, and J. The presence of several aminoglycoside ototoxicity-related MT-RNR1 gene mutations in Baltic-speaking Latvian population indicates the necessity to include ototoxicity-related mutation analysis in the future studies in order to determine the feasibility of DNA screening for patients before administration of aminoglycoside therapy.
Similar content being viewed by others
Introduction
Hearing ability is one of the key human senses which is important for the satisfactory quality of life. 360 million people worldwide have disabling hearing loss, and 32 million of those are children [1]. The causality of the hearing loss is multifactorial. Hereditary hearing loss can be conductive or sensorineural; it can be a part of a syndrome or a sole clinical symptom [2]. Acquired hearing causes include infectious diseases, chronic ear infections, otitis media, head or ear injury, excessive noise, physically blocked the ear canal, ageing, and use of certain medicines [1]. More than 150 drugs are currently known to be ototoxic; while the ototoxicity of many medicines, such as loop diuretics, macrolide antibiotics, and quinine resolves after treatment discontinuation, the use of platinum derivatives and aminoglycosides is associated with permanent hearing loss (reviewed in Lanvers-Kaminsky and Ciarimboli, 2017) [3].
Despite known nephro side effects and ototoxic side effects, aminoglycosides are still commonly prescribed antibiotics in clinical practice used to treat severe or hospital-acquired gram-negative infections, neonatal sepsis, and multidrug-resistant tuberculosis [4, 5]. Ototoxic side effects occur within days or weeks after systemic application of any amount (including a single dose) of the antibiotic, and could manifest as either cochlea damage with permanent hearing loss or vestibular damage with dizziness, ataxia and/or, nystagmus [6, 7]. Streptomycin and gentamicin are primarily vestibulotoxic, whereas amikacin, neomycin, dihydrosterptomycin, and kanamicin are primarily cochleotoxic [8]. The main etiology of the sensory deficit is death of inner ear sensory hair cells selectively triggered by aminoglycosides, and known mechanisms include drug trafficking across endothelial and epithelial barrier layers, sensory cell uptake of these drugs, and disruption of intracellular physiological pathways (reviewed in Jiang et al., 2017) [9].
Patients’ individual susceptibility to aminoglycoside-induced hearing loss (AIHL [MIM: 580000] [10]) varies considerably, and several risk factors have been identified including high doses, high plasma concentrations, frequent applications, long treatment periods, renal dysfunction, older age, noise exposure, preexisting hearing impairment, and co-administration of other ototoxic or nephrotoxic drugs [3]. AIHL also reflects environmental-genetic interactions, as it occurs more likely in persons with specific variants in the mitochondrial genome (mtDNA) and is transmitted by maternal inheritance. A mitochondrion is a very essential organelle of a eukaryotic cell that provides cellular energy, and large deletions in the mitochondrial genome and definite mitochondrial point mutations usually lead to syndromic deafness [11]. MtDNA abnormality as a possible basis of the maternal inheritance of the aminoglycoside ototoxicity was firstly noted by Higashi in 1989 [12]. Later, several mutations, such as m.1555A>G, m.1494C>T, m.961_962delTinsC(n), m.1095T>C and m.827A>G were discovered in the mitochondrial ribosomal 12S subunit gene (MT-RNR1) and associated with both AIHL and nonsyndromic hearing loss (NSHL) [13,14,15,16,17,18].
The pooled prevalence of the AIHL-related MT-RNR1 gene mutations in general global population was shown to be 2%; however, in different populations it seems to be variable [19]. Comprehensive worldwide data are still lacking, making it difficult to estimate the risk of AIHL in general, and to differentiate pathological mtDNA mutations from nonpathogenic polymorphisms. Moreover, variation in the degree of hearing loss in patients with mtDNA mutations indicates the involvement of additional environmental factors or genetic modifiers, many of which still have to be deciphered [20].
In Latvia, aminoglycosides are commonly prescribed as a second-line anti-tuberculosis drugs used for multidrug-resistant tuberculosis treatment [21]. In addition, the use of aminoglycoside antibiotics in the treatment of infections in babies in neonatal intensive care units has been considered as an important risk factor of sensorineural hearing loss among children and, especially, preterm infants [22]. The goal of this study was to cognize the frequency of AIHL-related MT-RNR1 gene mutations in Baltic-speaking ethnic Latvian population, and to estimate the prevalence of such mutations in the population-specific mitochondrial haplogroups (mtDNA hgs).
Materials and methods
Subjects
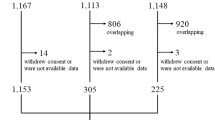
DNA samples of 191 ethnic non-related Latvians (European population, the Baltic region), i.e., individuals who are considered themselves as Latvians for three generations, were used in this study. Among them, 107 were females (56%), 84 males (44%); mean age was 53 years (16–88 years).
The samples and information were obtained from the Genome Database of the Latvian Population (VIGDB). The project was conducted in accordance with the Helsinki Declaration; the study protocol was approved by the Central Medical Committee of Ethics in Latvia.
mtDNA MT-RNR1 gene analysis
For the detection of mtDNA MT-RNR1 gene mutations which were associated with AIHL, a polymerase chain reaction (PCR) amplification of the partial mtDNA sequence and sequencing of the obtained fragment was performed. Briefly, a 1580-bp mtDNA fragment was amplified targeting whole-length MT-RNR1 gene using following primers: forward 12smtF 5′- CCGCTTCTGGCCACAGCACT -3′ (mtDNA bases 314–333), and reverse 12smtR 5′- CTTTGGCTCTCCTTGCAA –3′ (bases 1894-1877). The PCR was performed in a final volume of 25 µl. PCR mix for one reaction contained 14 ng of DNA template, 0.025 U/μl of Thermo Scientific Dream Taq Hot Start DNA polymerase (Thermo Fisher Scientific, USA), 1× Dream Taq Buffer, 0.2 μM of each primer, 0.2 mM of dNTP mix (Thermo Fisher Scientific, USA).
The PCR was performed under the following conditions: an initial denaturation at 95 °C for 3 min; 30 cycles of denaturation at 95 °C for 30 s, annealing at 61 °C for 30 s, extension at 72° for 1 min; final extension at 72 °C for 5 min. The PCR products were separated using electrophoresis on a 1.5% agarose gel (TopVision Agarose, Thermo Fisher Scientific, USA) in Tris-acetate EDTA buffer containing 0.2 mg of ethidium bromide/ml and were visualized with transillumination under UV light. Positive PCR products were purified using the ExoI and FastAP enzymes (Thermo Fisher Scientific, USA) and subsequently sequenced on both strands by Sanger method using the BigDye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems, USA). All sequences were analyzed using Contig Express software (ContigExpress, USA).
The mtDNA reference sequence which was used for primer design was obtained from the National Center for Biotechnology web site (http://www.ncbi.nlm.nih.gov/GenBank Accession No. NC_012920: Homo sapiens mitochondrion, complete genome). The Human Mitochondrial DNA Revised Cambridge Reference Sequence was used for mutation/polymorphism analysis. This sequence was obtained from the MITOMAP database available from https://www.mitomap.org/foswiki/bin/view/MITOMAP/HumanMitoSeq.
mtDNA HV1 and HV2 variation
The analysis of the two hypervariable regions (HV1 and HV2) of the control region of the mtDNA was performed by sequencing. A 609-bp fragment, which contains the HV1 region, was amplified by PCR using primers HVS1-F (5’TACACCAGTCTTGTAAACC) and HVS1-R (5’CCTGAAGTAGGAACCAGATG). The PCR was performed in a final volume of 20 µl. The PCR mix contained (per reaction) 1× Taq Buffer with 20 mM (NH4)2SO4, 3.125 mM MgCl2, 100 µM of each dNTPs, 0.25 µM of each primer, 1 U of Taq DNA polymerase (recombinant) and 21 ng of DNA template. The PCR assays were performed under the following conditions: an initial denaturation at 95 °C for 3 min; 30 cycles of denaturation at 95 °C for 30 s, primer annealing at 56 °C for 30 s, and elongation at 72 °C for 40 s; and a final elongation step at 72 °C for 5 min.
A 738-bp fragment, which contains the HV2 region, was amplified by PCR using primers HVS2-F (5’TGGGGGTAGCTAAAGTGAACT) and HVS2-R (5’GGTGATGTGAGCCCGTCTAA). The PCR master mix was identical to that used for HV1 region. The PCR assays were performed under the following conditions: an initial denaturation at 95 °C for 3 min; 30 cycles of denaturation at 95 °C for 30 s, primer annealing at 54 °C for 45 s, and elongation at 72 °C for 40 s; and a final elongation step at 72 °C for 5 min.
The PCR products were separated using electrophoresis on a 1.5% agarose gel (TopVision Agarose, Thermo Fisher Scientific, USA) in Tris-acetate EDTA buffer containing 0.2 mg of ethidium bromide/ml and were visualized with transillumination under UV light. Positive PCR products were purified using the ExoI and FastAP enzymes (Thermo Fisher Scientific, USA) and subsequently sequenced on both DNA strands using the ABI PRISM BigDye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems) according to the manufacturer’s recommendations on an ABI Prism 3100 Genetic Analyzer (PerkinElmer, USA).
The PCR reagents were purchased from Thermo Fisher Scientific, USA.
Mitochondrial haplogroups
To investigate the mtDNA hg affiliation, hierarchical PCR–RFLP analysis was performed using the method described elsewhere [23]. The classification of mtDNA hgs was based on their position in the hierarchy of the mitochondrial phylogenetic tree available from www.phylotree.org [24].
Statistical analysis
The statistical analysis was made using GraphPad Software (GraphPad Software Inc., USA) two-tailed Fisher’s exact test for categorical data (2 × 2 contingency table was analyzed). Two-tailed p value less than or equal to 0.05 was considered significant.
Results
mtDNA MT-RNR1 gene mutation analysis
PCR amplicons of the desired length were successfully obtained from all DNA samples, and sequence data for all targeted mutations were included in this study. The representative cases are shown in a Supplementary Fig. S1. In total, 7.3% of samples (14/191) had shown MT-RNR1 gene changes; 10 samples were from females (9.3%) and 4 from males (4.8%) (P = 0.2732). All detected mtDNA mutations were homoplasmic and were present in separate DNA samples.
The results have revealed the presence of six different genetic changes in the MT-RNR1 gene among ethnic Latvians (Table 1). The most frequently observed mutations in this study were m.961insC(n) and m.961T>G; these changes were identified with a frequency of 2.09% (4/191) each (Table 1).
Further, m.827A>G and m.951G>A genetic changes were found in 2 out of the 191 DNA samples each (estimated frequency in our cohort = 1.05%), while both m.1555A>G and m.961T>A mutations were identified in one carrier each with an estimated frequency of 0.52%. Sequence data analysis revealed that m.961delTinsC(n), m.1494C>T and m.1095T>C mutations, which have been previously associated with AIHL, were not present in our cohort (Table 1).
The observed prevalence of m.1555A>G mutation in Latvians (i.e., 0.52) was statistically similar to those found in studies in Finland, Poland, the United States of America (USA), New Zealand and the United Kingdom (UK) (Table 1). Similarly, the frequency of m.827A>G genetic change in Latvians was in agreement to those reported in Poland and the USA (1.05 vs. 0.2 and 0.78, respectively). The absence of rare m.1494C>T and m.1095T>C genetic changes in our study cohort was concordant to the results from other countries; previously, the low number of m.1494C>T mutation-positive samples has been reported only in the general USA and Chinese populations. Similarly, m.961delTinsC(n) mutation was absent in the ethnic Latvian population in this study; while this genetic change has been reported in Poland and the USA (frequency 0.4 and 0.78, respectively), the difference was not statistically significant (P > 0.05).
The results of this study indicated that both m.961insC(n) and m.961T>G mutations were observed significantly more often in the ethnical Latvians than in the general USA population (P = 0.0273 and P = 0.0406, respectively) (Table 1). The frequency of both mutations (i.e., 2.09) was also higher in Latvians than those reported in Polish population (0.6 and 0.8, respectively), however, the difference was not statistically significant for this study cohort.
MT-RNR1 gene mutations in mtDNA haplogroups
In order to evaluate the occurrence of MT-RNR1 mutations within specific maternal hgs, the mtDNA hg composition in the samples has been analyzed. The observed mtDNA hg frequencies found among Latvians are summarized in Table 2. As it was expected, the results showed that the composition of observed mtDNA hgs was similar to that reported earlier in Latvian population, and the vast majority of observed mtDNA variants belong to hgs which are common to most European populations [25]. Meanwhile, MT-RNR1 mutations were found in four mtDNA hgs: H, U, T, and J; these hgs were also the most frequent in our sample cohort (Table 2).
Hg H, which is the most frequent mtDNA hg in all European populations except the Saami, accounted for 38.74% of the samples in this study. Among hg H samples, three different MT-RNR1 mutations were found: m.961T>G was detected in four, m.951T>A – in two, and m.961T>A – in one sample. None of these mutations were detected in samples belonged to the other mtDNA hgs (Table 2). All four m.961T>G-positive samples belonged to the subclade H11a of the hg H. Approximately one third (32.46%) of mtDNA variants belonged to the hg U in this study. This observation was similar to the earlier results obtained for the Latvian gene pool and neighboring populations [25]. All four m.961insC(n)–positive samples belonged to the hg U in our study, and the estimated frequency of this mutation was as high as 6.45% for this mtDNA hg. Both hgs T and J were found at a relatively high proportion in our cohort: 7.33% and 9.95%, respectively. The single m.1555A>G mutation–positive sample in our study belonged to the hg J, while both samples with m.827A>G mutation belonged to the hg T. No MT-RNR1 gene mutations have been observed in the minor mtDNA hgs, such as V, I, HV, and W.
mtDNA HV1 and HV2 variation
In order to analyze if DNA samples which carryed identical mutations were not inherited the same maternal lineage, sequences from the hypervariable region HV1 of the control region of the mtDNA were obtained and analyzed. Based on this analysis, all but two samples have shown different haplogroup confirming that these DNA samples came from unrelated individuals (Table 3).
Further, two DNA samples with identical HV1 region were studied by analysis of the hypervariable region HV2. Again, an identical haplogroup was observed indicating strong possibility of the same maternal lineage (Table 3). Thus, while the information obtained from the VIGDB did not indicate any known family relationships between these samples, the founder effect could not been ruled out for these samples.
Discussion
Numerous studies have highlighted the mtDNA MT-RNR1 gene as a hotspot for the late-onset NSHL, and several mutations have been strongly associated with increased susceptibility to AIHL in different populations [3]. In this study, for the first time, the frequency of mitochondrial MT-RNR1 gene mutations were studied in the Baltic-speaking ethnic Latvian population. Overall, the genotyping results of our sample cohort were consistent with those previously reported in neighboring European populations and Caucasians. The mutational screening of MT-RNR1 gene showed the presence of six known and putative AIHL and NSHL-associated mutations, and the aggregate frequency of all variants was as high as 7.3%.
The pathogenic m.1555A>G mutation has been frequently reported among patients with AIHL in white cohort from Poland (5.5%), and Asian populations in China and Japan (up to 13.3% and 33%, respectively) [26,27,28,29]. In the Spanish population, the frequency as high as 17% was reported in adult patients affected by NSHL [30]. In general populations, m.1555A>G mutation has been rarely reported, and the frequency did not exceed 0.5%; similar results were obtained in this study for the ethnic Latvians (0.52%).
The m.1494C>T variant has also shown strong associations with the development of AIHL. Across several studies in Chinese, Spanish and North American populations, all individuals with the m.1494C>T allele have developed hearing loss after receiving an aminoglycoside antibiotic (reviewed in ref. [31]). However, this pathogenic variant has been found only rarely in the general populations in China and the USA; the carrier frequency was determined to be 0.024% and 0.05%, respectively [32, 33]. The lack of m.1494C>T mtDNA variant have been noted among Brasilian, Finnish, and Polish patients, normal controls, and/or general populations, thus indicating that it is thought to be absent from some populations [26, 34,35,36]. In accordance to these observations, the m.1494C>T allele was not detected in any of our cohort’s samples. Similarly, m.1095T>C pathogenic variant was not detected in ethnic Latvians either. Overall, m.1095T>C mutation has been very rarely reported in general populations or in normal hearing controls worldwide, however, it was linked with SNHL in patients in China, Russia, and Japan [27, 28, 37, 38]. The absence of m.1095T>C and m.1494C>T variants in our study indicates that either these mutations are very rare or that both changes do not exist in ethnic Latvian population. Similar results were observed in the neighboring Finnish population [34].
A number of different variations at position 961 within MT-RNR1 gene have been found in individuals with AIHL and NSHL. M961delTinsC(n) mutation, which has been previously reported in studies in Poland and USA (refs. 26, 32, 39), was absent in our sample cohort. In oppose, the putatively pathogenic mutations m.961T>G and m.961insC(n) were the most frequent in our study: the prevalence rate for both mutations separately was as high as 2.09%. The carrier frequency for both mutations in our cohort was significantly higher than the rates reported in the population of the USA (Table 1). All m.961insC(n)–positive samples belonged to the hg U in our study; on the other hand, this genetic change was detected in the Caucasian hg T, the Native American/Asian hg A, and at least one other mtDNA hg in the USA, indicating that multiple ethnic groups may be at risk for carrying this mutation [39].
There are various opinions concerning m.961T>G allele: it is currently a defining mutation of H11a mitochondrial hg and is often considered as a non-pathogenic polymorphism; however, there are reports about its association with AIHL and SNHL [24, 40,41,42]. In the previous study, hg H, which is the most frequent mtDNA hg in all European populations except the Saami, accounted for 45% of the mtDNA variants in Latvians, while its subclade hg H11a was detected in 3.3% (10/299) of samples (i.e., 7.5% of all hg H) [25]. In this study, the mtDNA analysis have shown that all four m.961T>G mutation-positive samples in our cohort belonged to the hg H11a, thus providing an additional indirect evidence that m.961T>G is an hg-specific variant.
In oppose to m.961T>G, the compliance of m.961T>A with any of mtDNA hgs has not been shown previously [24]. In our study, this mutation has been detected in one sample which belonged to the hg H. Up to date, m.961T>A variant has been reported only in one NSHL patient in Russia [37]. Thus more studies are required to decipher whether this genetic change is indeed pathogenic or it is normal ethnic-associated mtDNA hg variation existing among certain populations.
M.827A>G has been frequently reported in Chinese patients with NSHL and AIHL, but not in normal hearing controls; the reported frequency rate in Chinese patients was from 3.3% to 4.4% [27, 28]. Controversially, in Brasil, this mutation has been observed in both patients and normal controls with a frequency 13.2% and 8.6%, respectively [43]. In the general population studies, the carrier frequencies for m.827A>G were 0.2% and 0.78% in Poland and USA, respectively [32, 35]. In our study, m.827A>G mutation has been detected in two samples (estimated frequency 1.05%); both samples belonged to the hg T.
Worldwide studies revealed that the prevalence of mtDNA mutations considerably varies between patients and might not necessarily result in a deafness phenotype. Thus, it has been proposed that other genetic variants, including mtDNA hgs, may contribute to the manifestation of AIHL [44]. It was also shown that mtDNA hg B increases the risk for hearing loss among the Eastern Asian pedigrees carrying m.1555A>G mutation [45]. On the other hand, Torroni and colleagues showed that m.1555A>G mutation occurs on mtDNA hgs that are common in all European populations, and concluded that mtDNA backgrounds do not play a significant role in the expression of this mutation [46]. In our study, all detected MT-RNR1 gene variations occurred in separate mtDNA hgs. Whether there are some interactions between specific hgs, mtDNA MT-RNR1 gene mutations and aminoglycoside ototoxicity is an intriguing yet pending puzzle.
In conclusions, the presence of several aminoglycoside ototoxicity-related mtDNA MT-RNR1 gene mutations in Baltic-speaking Latvian population indicates the necessity to include ototoxicity-related mutation analysis in the future studies in order to determine the feasibility of DNA screening for patients before administration of aminoglycoside therapy. The exact reason and the magnitude for the occurrence of specific MT-RNR1 mutations in particular mtDNA hgs that was observed in our study remains unclear and urges additional research.
References
World Health Organization (WHO). Multi-country assessment of national capacity to provide hearing care. Geneva: World Health Organization; 2013.
Cohen MM, Gorlin RJ. Epidemiology, etiology and genetic patterns. In: Gorlin RJ, Toriello HV, Cohen MMJ, editors. Hereditary hearing loss and its syndromes. New York: Oxford University Press; 1995. p. 9–21.
Lanvers-Kaminsky C, Ciarimboli G. Pharmacogenetics of drug-induced ototoxicity caused by aminoglycosides and cisplatin. Pharmacogenomics. 2017;18:1683–95.
Kester M, Karpa KD, Vrana KE. Treatment of infectious diseases. In: Kester M, Karpa KD, Vrana KE, editors. Elsevier’s integrated review pharmacology. Second Edition. Philadelphia: W.B. Saunders; 2012. p. 41–78.
WHO. Treatment of tuberculosis guidelines. Fourth edition. Switzerland: WHO Press; 2010. p. 84–5.
Heck WE, Hinshaw HC, Parsons HG. Auditory ototoxicity in tuberculosis patients treated with a report of the incidence of hearing loss in a series of 1,150 cases. JAMA. 1963;86:18–20.
Duggal P, Sarkar M. Audiologic monitoring of multi-drug resistant tuberculosis patients on aminoglycoside treatment with long term follow-up.2007. BMC Ear Nose Throat Disord. 2007;7:5.
Selimoglu E. Aminoglycoside-induced ototoxicity. Curr Pharm Des. 2007;13(1):119–26.
Jiang M, Karasawa T, Steyger PS. Aminoglycoside-induced cochleotoxicity: a review. Front Cell Neurosci. 2007;11:308.
OMIM. Online Mendelian Inheritance in Man. An online catalog of human genes and genetic disorders. 7 June 2018 http://www.omim.org/.
Finsterer J. Mitochondriopathies. Eur J Neurol. 2004;11:163–86.
Higashi K. Unique inheritance of streptomycin-induced deafness. Clin Genet. 1989;35(6):433–6.
Prezant TR, Agapian JV, Bohlman MC, Bu X, Oztas S, Qiu WQ, et al. Mitochondrial ribosomal RNA mutation associated with both antibiotic-induced and non-syndromic deafness. Nat Genet. 1993;4(3):289–94.
Zhao H, Li R, Wang Q, Yan Q, Deng JH, Han D, et al. Maternally inherited aminoglycoside-induced and nonsyndromic deafness is associated with the novel C1494T mutation in the mitochondrial 12S rRNA gene in a large Chinese family. Am J Hum Genet. 2004;74(1):139–52.
Matthijs G, Claes S, Longo-Bbenza B, Cassiman JJ. Non-syndromic deafness associated with a mutation and a polymorphism in the mitochondrial 12S ribosomal RNA gene in a large Zairean pedigree. Eur J Hum Genet. 1996;4:46–51.
Usami S, Abe S, Kasai M, Shinkawa H, Moeller B, Kenyon JB, et al. Genetic and clinical features of sensorineural hearing loss associated with the 1555 mitochondrial mutation. Laryngoscope. 1997;107(4):483–90.
Thyagarajan D, Bressman S, Bruno C, Przedborski S, Shanske S, Lynch T, et al. A novel mitochondrial 12SrRNA point mutation in Parkinsonism, deafness, and neuropathy. Ann Neurol. 2000;48(5):730–6.
Xing G, Chen Z, Wei Q, Tian H, Li X, Zhou A, et al. Maternally inherited non-syndromic hearing loss associated with mitochondrial 12S rRNA A827G mutation in a Chinese family. Biochem Biophys Res Commun. 2006;344(4):1253–7.
Ibekwe TS, Bhimrao SK, Westerberg BD, Kozak FK. A meta-analysis and systematic review of the prevalence of mitochondrially encoded 12S RNA in the general population: Is there a role for screening neonates requiring aminoglycosides? Afr J Paediatr Surg. 2015;12(2):105–13.
Guan MX. Mitochondrial 12S rRNA mutations associated with aminoglycoside ototoxicity. Mitochondrion. 2011;11(2):237–45.
Bauskenieks M, Pole I, Skenders G, Jansone I, Broka L, Nodieva A, et al. Genotypic and phenotypic characteristics of aminoglycoside-resistant Mycobacterium tuberculosisisolates in Latvia. Diagn Microbiol Infect Dis. 2015;81(3):177–82.
Zimmerman E, Lahav A. Ototoxicity in preterm infants: effects of genetics, aminoglycosides, and loud environmental noise. J Perinatol. 2013;33(1):3–8.
Torroni A, Huoponen K, Francalacci P, Petrozzi M, Morelli L, Scozzari R, et al. Classification of European mtDNAs from an analysis of three European populations. Genetics. 1996;144(4):1835–50.
Van Oven M, Kayser M. Updated comprehensive phylogenetic tree of global human mitochondrial DNA variation. Hum Mutat. 2009;30(2):E386–94.
Pliss L, Tambets K, Loogvali EL, Pronina N, Lazdins M, Krumin A, et al. Mitochondrial DNA portrait of Latvians: towards the understanding of the genetic structure of Baltic-speaking populations. Ann Hum Genet. 2006;70:439–58.
Rydzanicz M, Wróbel M, Pollak A, Gawęcki W, Brauze D, Kostrzewska-Poczekaj M, et al. Mutation analysis of mitochondrial 12S rRNA gene in Polish patients with non-syndromic and aminoglycoside-induced hearing loss. Biochem Biophys Res Commun. 2010;395(1):116–21.
Li Z, Li R, Chen J, Liao Z, Zhu Y, Qian Y, et al. Mutational analysis of the mitochondrial 12S rRNA gene in Chinese pediatric subjects with aminoglycoside-induced and non-syndromic hearing loss. Hum Genet. 2005;117(1):9–15.
Lu J, Li Z, Zhu Y, Yang A, Li R, Zheng J, et al. Mitochondrial 12S rRNA variants in 1642 Han Chinese pediatric subjects with aminoglycoside-induced and nonsyndromic hearing loss. Mitochondrion. 2010;10(4):380–90.
Usami S, Abe S, Akita J, Namba A, Shinkawa H, Ishii M, et al. Prevalence of mitochondrial gene mutations among hearing impaired patients. J Med Genet. 2000;37(1):38–40.
Bravo O, Ballana E, Estivill X. Cochlear alterations in deaf and unaffected subjects carrying the deafness-associated A1555G mutation in the mitochondrial 12S rRNA gene. Biochem Biophys Res Commun. 2006;344:511–6.
Barbarino JM, McGregor TL, Altman RB, Klein TE. PharmGKB summary: very important pharmacogene information for MT-RNR1. Pharm Genom. 2016;26(12):558–67.
Ealy M, Lynch KA, Meyer NC, Smith RJ. The prevalence of mitochondrial mutations associated with aminoglycoside‐induced sensorineural hearing loss in an NICU population. Laryngoscope. 2011;121(6):1184–6.
Han S, Yang X, Zhou Y, Hao J, Shen A, Xu F, et al. Deafness gene mutations in newborns in Beijing. Acta Otolaryngol. 2016;136(5):475–9.
Soini HK, Karjalainen MK, Hinttala R, Rautio A, Hallman M, Uusimaa J. Mitochondrial hearing loss mutations among Finnish preterm and term-born infants. Audiol Res. 2017;7(2):189.
Rydzanicz M, Wróbel M, Cywińska K, Froehlich D, Gawecki W, Szyfter W, et al. Screening of the general Polish population for deafness-associated mutations in mitochondrial 12S rRNA and tRNA Ser(UCN) genes. Genet Test Mol Biomark. 2009;13(2):167–72.
Postal M, Palodeto B, Sartorato EL, Oliveira CA. C1494T mitochondrial DNA mutation, hearing loss, and aminoglycosides antibiotics. Braz J Otorhinolaryngol. 2009;75(6):884–7.
Dzhemileva LU, Posukh OL, Tazetdinov AM, Barashkov NA, Zhuravskii SA, Ponidelko SN, et al. Analysis of mitochondrial 12S rRNA and tRNASer(UCN) genes in patients with nonsyndromic sensorineural hearing loss from various regions of Russia. Rus J Genet. 2009;45(7):861–9.
Yano T, Nishio S, Usami S, The Deafness Gene Study Consortium. Frequency of mitochondrial mutations in non-syndromic hearing loss as well as possibly responsible variants found by whole mitochondrial genome screening. J Hum Genet. 2014;59:100–6.
Tang HY, Hutcheson E, Neill S, Drummond-Borg M, Speer M, Alford RL. Genetic susceptibility to aminoglycoside ototoxicity: how many are at risk? Genet Med. 2002;4:336–45.
Li R, Greinwald J, Yang L, Choo DI, Wenstrup RJ, Guan MX. Molecular analysis of the mitochondrial 12S rRNA and tRNASer(UCN) genes in paediatric subjects with nonsyndromic hearing loss. J Med Genet. 2004;41:615–20.
Turchetta R, Mazzei F, Celani T, Cammeresi MG, Orlando MP, Altissimi G, et al. Audiological and radiological characteristics of a family with T961G mitochondrial mutation. Int J Audiol. 2012;51(12):870–9.
Guaran V, Astolfi L, Castiglione A, Simoni E, Olivetto E, Galasso M, et al. Association between idiopathic hearing loss and mitochondrial DNA mutations: A study on 169 hearing-impaired subjects. Int J Mol Med. 2013;32(4):785–94.
Alves RM, da Silva Costa SM, do Amôr Divino Miranda PM, Ramos PZ, Marconi TG, Santos Oliveira G, et al. Analysis of mitochondrial alterations in Brazilian patients with sensorineural hearing loss using MALDI-TOF mass spectrometry. BMC Med Genet. 2016;17:41.
Lu J, Qian Y, Li Z, Yang A, Zhu Y, Li R, et al. Mitochondrial haplotypes may modulate the phenotypic manifestation of the deafness-associated 12S rRNA 1555A>G mutation. Mitochondrion. 2010;10(1):69–81.
Ying Z, Zheng J, Cai Z, Liu L, Dai Y, Yao J, et al. Mitochondrial haplogroup B increases the risk for hearing loss among the Eastern Asian pedigrees carrying 12S rRNA 1555A>G mutation. Protein Cell. 2015;6(11):844–8.
Torroni A, Cruciani F, Rengo C, Sellitto D, López-Bigas N, Rabionet R, et al. The A1555G mutation in the 12S rRNA gene of human mtDNA: recurrent origins and founder events in families affected by sensorineural deafness. Am J Hum Genet. 1999;65(5):1349–58.
Scrimshaw BJ, Faed JM, Tate WP, Yun K. The frequency in New Zealand of a mitochondrial DNA mutation (1555 A to G) associated with aminoglycoside-induced hearing loss. NZ Med J. 1999;112(1089):216–7.
Gravina LP, Foncuberta ME, Estrada RC, Barreiro C, Chertkoff L. Carrier frequency of the 35delG and A1555G deafness mutations in the Argentinean population: Impact on the newborn hearing screening. Int J Pediatr Otorhinolaryngol. 2007;71(4):639–43.
Rahman S, Ecob R, Costello H, Sweeney MG, Duncan AJ, Pearce K, et al. Hearing in 44–45 year olds with m.1555A>G, a genetic mutation predisposing to aminoglycoside-induced deafness: a population based cohort study. BMJ Open. 2012;2(1):e000411.
Landrum MJ, Lee JM, Benson M, Brown GR, Chao C, Chitipiralla S, et al. ClinVar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res. 2018;46(D1):D1062–7.
Acknowledgements
We acknowledge the Genome Database of the Latvian Population for providing DNA samples used in this study. The research was supported by Latvian National Research Program VPP “BIOMEDICINE”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Igumnova, V., Veidemane, L., Vīksna, A. et al. The prevalence of mitochondrial mutations associated with aminoglycoside-induced deafness in ethnic Latvian population: the appraisal of the evidence. J Hum Genet 64, 199–206 (2019). https://doi.org/10.1038/s10038-018-0544-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s10038-018-0544-6