Abstract
ETS proto-oncogene 1, transcription factor (ETS1) is involved in various immune responses. Genome-wide association studies on systemic lupus erythematosus in Chinese populations identified the association of ETS1 polymorphism in 3′ untranslated region, rs1128334A, which was associated with lower ETS1 expression. In view of substantial sharing of susceptibility genes across multiple autoimmune diseases, we examined whether ETS1 is associated with a rare autoimmune rheumatic disease, anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV). Association of rs1128334 was tested in 466 Japanese patients with AAV and 1099 healthy controls by logistic regression analysis under the additive model. AAV patients were classified into 285 microscopic polyangiitis (MPA), 92 granulomatosis with polyangiitis (GPA), 56 eosinophilic GPA, and 33 unclassifiable AAV, according to the European Medicines Agency (EMEA) algorithm. Among the patients, 376 were positive for MPO–ANCA and 62 for PR3–ANCA. When the patients were classified according to the EMEA classification, rs1128334A allele was significantly increased in GPA (P = 0.0060, P c = 0.030, odds ratio (OR), 1.54; 95% confidence interval (CI), 1.13–2.10). With respect to the ANCA specificity, significant association was observed in PR3–ANCA positive AAV (P = 0.0042, P c = 0.021, OR, 1.72; 95% CI, 1.19–2.49). In conclusion, ETS1 polymorphism was suggested to be associated with GPA and PR3–ANCA positive AAV in a Japanese population.
Similar content being viewed by others
Introduction
Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is a group of rare systemic vasculitides characterized by production of ANCA. AAV is classified into three subsets, microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA), and eosinophilic granulomatosis with polyangiitis (EGPA) based on clinical symptoms. Major ANCA antigens are myeloperoxidase (MPO) and proteinase 3 (PR3), and generally, MPO–ANCA is preferentially detected in MPA and EGPA, while PR3–ANCA is mainly observed in GPA [1].
Prevalence of AAV subsets substantially differs between European and Japanese populations. In contrast to the European populations where GPA and PR3–ANCA positive AAV (PR3–AAV) account for the majority of AAV, MPA, and MPO–ANCA positive AAV (MPO–AAV) are predominant in Japan. According to the population-based prospective study, annual incidence of MPA and GPA are 18.2 and 2.1/million in Japan, while 6.5 and 14.3/million in the United Kingdom, respectively [2]. In addition, about half of the Japanese GPA patients are positive for MPO–ANCA [3]. Such epidemiological differences may partly be caused by differences in the genetic background between the populations of European and Asian ancestries.
Thus far, we reported association of HLA-DRB1*09:01 and DRB1*13:02 with susceptibility and protection to MPO–AAV, respectively, in a Japanese population [4]. On the other hand, DPB1*04:01, previously shown to be associated with GPA in populations of European ancestry [5], showed a tendency toward association with PR3–AAV also in Japan [4]. Of interest, DRB1*09:01 is highly prevalent in the Japanese population (15.3%) [4], while very rare in the European populations (1.0%) (allele frequency net database; http://www.allelefrequencies.net) [6]. In contrast, DPB1*04:01 is prevalent in the European populations (42.5%) (allele frequency net database) [6], but relatively rare in the Japanese (6.3%) [4]. These findings indeed support the hypothesis that differences in the genetic background may partly account for the differences in the incidence of AAV subsets between populations.
Recently, three genome-wide association studies (GWAS) of AAV have been published in the populations of European ancestry [7,8,9]. These studies, along with previous candidate gene studies [5, 10], demonstrated association of HLA-DPB1*04 and SERPINA1, encoding α1-antitrpsin, with GPA or PR3–AAV, and also suggested several other candidate genes. However, with respect to MPA/MPO–AAV, convincing association was only reported in the HLA-DR/DQ region [7, 9]. This may partly be caused by relatively small sample size of MPA/MPO–AAV in the Caucasian studies. Thus, AAV genetics in Asian populations might provide valuable insights.
Due to the low prevalence of AAV, GWAS has not been reported in the Asian populations, and at this point, efficient selection of candidate genes is considered a reasonable approach. Recent studies have revealed that a number of susceptibility genes are shared across multiple autoimmune diseases [11]. Indeed, genes such as IRF5, STAT4, BLK, and TNFAIP3 have been shown to be associated with systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and systemic sclerosis (SSc) in a Japanese population [12,13,14,15]. With respect to HLA risk or protective alleles in AAV, DRB1*09:01 has been shown to be positively associated with SLE, RA, and type 1 diabetes [16, 17], while DRB1*13:02 is associated with protection against SLE, RA, and SSc as well [18,19,20].
ETS proto-oncogene 1, transcription factor (ETS1) is a transcription factor belonging to the ETS family characterized by an ETS DNA-binding domain, which recognizes a GGAA/T motif [21]. ETS1 plays a role in immunity, angiogenesis, and cancer progression, and is expressed in B cells, T cells, natural killer cells, endothelial cells, and cancer cells [21,22,23]. ETS1 negatively regulates B-cell differentiation into plasma cells by suppressing function of BLIMP1, a positive regulator of plasma cell differentiation. In T cells, reduction of T helper (Th) 1 cytokine, interferon γ, and decrease in regulatory T cells (Tregs) were observed in Ets1-deficient mice. On the other hand, Th17 differentiation was enhanced by Ets1 deficiency [22, 23].
GWAS on SLE in Chinese populations identified the association of two ETS1 single nucleotide polymorphisms (SNPs) in tight linkage disequilibrium (LD), rs1128334 and rs6590330 [24, 25], which was later replicated in the European populations [26]. The SNP rs1128334 is located in 3′ untranslated region (UTR) of ETS1 gene, and the SLE risk allele, rs1128334A, was reported to be associated with reduced ETS1 expression [25]. In addition, association with rs1128334A was also observed in another rheumatic disease, ankylosing spondylitis (AS), in a Chinese population [27].
Based on the functional relevance of ETS1 in AAV and previous reports of association with multiple rheumatic disease especially in the Asian populations, we considered ETS1 as a candidate gene for AAV. Thus far, the association study of ETS1 has not been reported in AAV in the Asian populations. In the present study, we investigated whether ETS1 polymorphism is associated with AAV in a Japanese population.
Materials and Methods
Patients and healthy controls
Four hundred and sixty-six Japanese patients with AAV and 1099 healthy controls were studied. The patients were recruited at the institutes participating in the Research Committee on Intractable Vasculitides and in the Research Group on Progressive Renal Diseases, both organized by the Ministry of Health, Labor, and Welfare of Japan, research groups organized by Sagamihara Hospital, National Hospital Organization, and the Tokyo Medical and Dental University. Healthy controls were recruited at University of Tsukuba, the University of Tokyo, Juntendo University, and Sagamihara Hospital. In addition, genomic DNA from 514 healthy individuals were purchased from the Health Science Research Resources Bank (Osaka, Japan).
The AAV patients were classified according to the European Medicines Agency (EMEA) algorithm (285 MPA, 92 GPA, 56 EGPA, and 33 unclassifiable) [28] or ANCA specificity (376 MPO–ANCA positive, 62 PR3–ANCA positive). Characteristics in the AAV patients and healthy controls are shown in Table 1. Forty-six patients were PR3–ANCA positive GPA, which accounts for 50% of GPA, and 74% of PR3–ANCA positive AAV.
Ethics statement
This study was reviewed and approved by the Ethics Committees of University of Tsukuba, National Hospital Organization Sagamihara Hospital, the Tokyo Medical and Dental University, Okayama University, Kyoto University, Kagawa University, Juntendo University, St. Marianna University, Kanazawa University, the University of Tokyo, Kyorin University, Saitama Medical Center Hospital, the University of Miyazaki, Toho University, Kobe University Hospital, Kitano Hospital, Shimane University, Nagoya City University, Ehime University, Jichi Medical University, Kyoto Prefectural University, Tokyo Medical University Hachioji Medical Center, Kitasato University Hospital, Hamamatsu University, National Hospital Organization Shimoshizu National Hospital, Tenri Hospital, Tokyo Metropolitan Geriatric Hospital and Institute of Gerontology, Hyogo University, Kawasaki Municipal Hospital, Sendai Shakaihoken Hospital, Tokyo Women’s Medical College, Kyoundo Hospital, Tokyo Metropolitan Komagome Hospital, Ome Municipal General Hospital, Teikyo University, Hokkaido University, Fukuoka University, Okayama Saiseikai General Hospital, Aichi Medical University, Asahikawa Medical University, Kyushu University, Iwate Prefectural Central Hospital, and Nagasaki University. Written informed consent was obtained from all participants, except for some healthy individuals who donated blood for use in medical genetics studies before 2001, that is, prior to the implementation by the Japanese government of the Ethics Guidelines for Human Genome/Gene Analysis Research. From such healthy individuals, verbal informed consent for the genetics study had been obtained. In accordance with the Japanese Ethical Guidelines for Human Genome/Gene Analysis Research, such samples were anonymized in an unlinkable fashion, and were included in this study after review and approval by the Ethics Committee of the University of Tsukuba. This study was conducted according to the principles expressed in the Declaration of Helsinki.
Genotyping
Genotypes of SNP rs1128334 were determined by the TaqMan SNP Genotyping Assays (Assay ID: C___7539918_10) (Thermo Fisher Scientific Inc, Waltham, MA).
Statistical analysis
Association was tested by logistic regression analysis under the additive model using Ekuseru-Toukei 2012 (Social Survey Research Information Co., Ltd., Tokyo, Japan). The significance level was set at 0.05. P values corrected for multiple testing by Bonferroni correction (P c) were calculated by multiplying uncorrected P values by the number of tests (n = 5). Adjustment for gender difference between patients with each AAV subset and healthy controls was performed by conditional logistic regression analysis. Power to detect statistical association at the significance level of 0.05 was calculated under the log-additive model using Quanto version 1.2.4 (http://biostats.usc.edu/Quanto.html). Sample size of each subset and healthy controls and observed odds ratio in each comparison were employed for power calculation.
For the calculation of LD values, genotype data of the polymorphisms in the ETS1 region was obtained from the 1000 Genomes browser (https://www.ncbi.nlm.nih.gov/variation/tools/1000genomes/), and r 2 values were calculated using Haploview version 4.0 software (Broad Institute, Cambridge, MA).
Genetic interaction between ETS1 rs1128334 and HLA-DPB1*04:01 was examined by logistic regression analysis as previously described [29]. The logistic regression model for interaction between gene i and gene j was defined as follows: logit(P) = β0 + βixi + βjxj + βijxixj, where xi and xj are 2 for the homozygotes for the risk alleles, 1 for the heterozygotes, and 0 for homozygotes for non-risk alleles, respectively. rs1128334A and HLA-DPB1*04:01 were risk alleles for ETS1 and HLA-DPB1.
Results
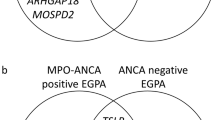
ETS1 gene is located on chromosome 11q24.3 and several ETS1 splicing isoforms were reported, among which four representative isoforms are shown in Fig. 1. LD analysis was conducted using the HapMap JPT (Japanese in Tokyo) data obtained from the 1000 Genomes browser. The SNPs associated with susceptibility to SLE, rs1128334 and rs6590330, are located in ETS1 3′ UTR and downstream of ETS1, respectively. These SNPs are in almost absolute LD (r 2 = 0.96). Therefore, rs1128334 in ETS1 3′ UTR was analyzed as the tag SNP in this study.
Structure and linkage disequilibrium status of ETS1 gene. Upper panel, four dominant ETS1 splicing isoforms (RefSeq accession numbers: NM_001143820, NM_005238, NM_001330451, and NM_001162422). Inset shows the enlarged view of the position of rs1128334 in the 3′ UTR of ETS1. Lower panel, linkage disequilibrium plot in the ETS1 region drawn using pairwise r 2 values between SNPs with minor allele frequency >0.2. SLE associated SNPs, rs1128334 and rs6590330, are indicated
First, to examine whether ETS1 rs1128334 is associated with AAV subsets based on EMEA classification (MPA, GPA, and EGPA), the frequency of rs1128334A was compared between patients of each AAV subset and healthy controls. No deviation of genotype distribution from Hardy–Weinberg equilibrium was observed in healthy controls (Hardy–Weinberg equilibrium test, P = 0.27). As shown in Table 2, rs1128334A was significantly increased in GPA compared with healthy controls under the additive model for the A allele (P = 0.0060, P c = 0.030; odds ratio (OR), 1.54; 95% confidence interval (CI), 1.13–2.10). No significant association was detected in MPA or EGPA (Table 2).
Next, the association of rs1128334 genotype with ANCA specificity of the AAV patients was examined. Significant increase of rs1128334A was observed in PR3–AAV (P = 0.0042, P c = 0.021; OR, 1.72; 95% CI, 1.19–2.49). The same trend for association was also observed in MPO–AAV, although the difference did not reach statistical significance after Bonferroni correction (P = 0.032, P c = 0.16; OR, 1.20; 95% CI, 1.02–1.43).
Statistical significance in association with GPA and PR3–AAV remained after adjustment for the gender difference between the patients and controls (GPA: P adjusted = 0.0082; OR, 1.52; 95% CI, 1.11–2.07; PR3–AAV: P adjusted = 0.0068; OR, 1.67; 95% CI, 1.15–2.43).
In the European and North American populations, HLA-DPB1*04:01 was associated with susceptibility to GPA [5, 8]. We also reported a trend for association of HLA-DPB1*04:01 with PR3–AAV in a Japanese population [4]. Therefore, we examined genetic interaction between ETS1 and HLA-DPB1*04:01. No evidence for genetic interaction between ETS1 rs1128334 and HLA-DPB1*04:01 was observed in the analysis of GPA or PR3–AAV (GPA: P = 0.75, PR3–AAV: P = 0.66).
Discussion
In this study, we detected association of a SNP rs1128334, located in the 3′UTR of ETS1, with GPA and PR3–AAV in a Japanese population. The risk allele, rs1128334A, was the same as in SLE and AS [25, 27]. Because of the low incidence of GPA and PR3–AAV in the Japanese population [2], the sample size of these subsets was small; nevertheless, the association remained significant after Bonferroni correction. Furthermore, although statistically not significant after Bonferroni correction, MPO–AAV also showed a similar trend for association. Although the sample size was larger than in GPA and PR3–AAV, the detection power was still not sufficient for MPA and MPO–AAV (0.445 and 0.565, respectively); therefore, these results need to be confirmed in future studies with a larger sample size.
To our knowledge, this is the first report to suggest association of ETS1 SNPs with AAV. A previous study in European populations reported that rs6590330, located downstream of ETS1 and is in almost absolute LD with rs1128334, did not detect any trend toward association with GPA (rs6590330A: OR, 0.98; P = 0.800) [30]. In SLE, the association of rs1128334 or rs6590330 was not detected in European GWAS; however, suggestive association with rs6590330 in European populations was detected when it was examined as a candidate SNP [26]. Frequency of the risk allele, rs1128334A, appears to be higher in Asian populations (0.351 in Hong Kong Chinese [25] and 0.387 in Japanese) as compared with that in European populations (0.106 in the HapMap CEU (residents with Northern and Western European ancestry from the CEPH collection)). Thus, it is possible that the genetic association was more sensitively detectable in the Asian populations.
rs1128334A, located in the 3′UTR of ETS1, was previously associated with reduced expression of ETS1 [25], and was predicted to constitute a binding site of microRNA, miR-381 in TargetScan Release 7.1 (http://www.targetscan.org/vert_71/). It was also reported that the SLE risk allele in rs6590330 was associated with increased binding of phosphorylated STAT1 (pSTAT1) to putative STAT1-binding site near rs6590330 and with decreased ETS1 expression [31]. These studies suggest the functional significance of both rs1128334 and rs6590330. In addition, the possibility that polymorphisms other than rs6590330 that are in LD with rs1128334 may have a functional role cannot be ruled out at this point. Twenty-one polymorphisms including rs6590330 show LD (r 2 ≥ 0.6) with rs1128334.
ETS1 has been shown to inhibit differentiation of plasma cells and Th17 cells, and to induce development of Tregs [23]. Th17 cells were reported to be increased in GPA patients [32]. Furthermore, when peripheral blood cells from the GPA patients were stimulated with PR3 in vitro, Th17 cells have been shown to increase in PR3–ANCA positive, but not in PR3–ANCA negative, GPA patients [33], suggesting that Th17 cells play a role in the pathogenesis of GPA. Moreover, functionally Ets1-deficient mice lacking the pointed domain of Ets1 showed increased plasma cell differentiation and production of autoantibodies upon TLR9 stimulation [34]. Taken together with these functional studies, our findings suggest that genetically determined reduced expression of ETS1 may result in T-cell and B-cell abnormalities, which eventually play a role in AAV.
Limitations of this study include small sample size of GPA and PR3–AAV, due to the low prevalence of these subsets in Japan. The annual incidence of GPA has been reported to be 2.1/million in Japan [2], and the total number of the registered patients of GPA in the year of 2015 in Japan was 2534, according to the report from Japan Intractable Diseases Information Center (http://www.nanbyou.or.jp/entry/5354). In fact, our current sample size was accomplished by nearly 20 years of nationwide collaboration, and is one of the largest among AAV genetics studies in Asian populations. Nevertheless, the association detected in this study needs to be replicated in future independent studies. Further extension of collaboration network is currently underway.
Case–control association studies suffer from the population stratification issue. It is generally considered that this may not be a critical problem in the Japanese population. Yamaguchi-Kabata et al. performed a principal component analysis based on 140,387 SNPs in 7003 Japanese individuals, and demonstrated that Japanese individuals were divided into two clusters, Hondo and Ryukyu, the latter includes most of the individuals from Okinawa (94.7%), and suggested that the differences in the proportion of the individuals from the Ryukyu cluster may affect the results of the case–control study [35]. However, the proportion of the individuals with the Ryukyu cluster is <3% in all regions of mainland islands of Japan, except for the Kyushu region (10.47%).
In our study, none of the controls were recruited in Okinawa and Kyushu regions, and among the patients with GPA and/or PR3–ANCA positive AAV, only two were recruited in Kyushu. Exclusion of these patients from analysis did not alter the association results (GPA vs. controls: uncorrected P = 0.0047, PR3–ANCA positive AAV vs. controls: uncorrected P = 0.0045). Thus, we believe that population stratification was not a major problem in this study.
In conclusion, this study suggested that a SNP associated with low expression of ETS1 is associated with susceptibility to GPA and PR3–AAV in a Japanese population. Although future replication studies are necessary, ETS1 was suggested to be a genetic factor shared by multiple autoimmune diseases in Asian populations.
References
Kallenberg CG, Heeringa P, Stegeman CA. Mechanisms of disease: pathogenesis and treatment of ANCA-associated vasculitides. Nat Clin Pract Rheumatol. 2006;2:661–70.
Fujimoto S, Watts RA, Kobayashi S, Suzuki K, Jayne DR, Scott DG, et al. Comparison of the epidemiology of anti-neutrophil cytoplasmic antibody-associated vasculitis between Japan and the UK. Rheumatology. 2011;50:1916–20.
Sada KE, Yamamura M, Harigai M, Fujii T, Dobashi H, Takasaki Y, et al. Classification and characteristics of Japanese patients with antineutrophil cytoplasmic antibody-associated vasculitis in a nationwide, prospective, inception cohort study. Arthritis Res Ther. 2014;16:R101; https://doi.org/10.1186/ar4550.
Kawasaki A, Hasebe N, Hidaka M, Hirano F, Sada KE, Kobayashi S, et al. Protective role of HLA-DRB1*13:02 against microscopic polyangiitis and MPO-ANCA-positive vasculitides in a Japanese population: a case-control study. PLoS ONE. 2016;11:e0154393; https://doi.org/10.1371/journal.pone.0154393.
Heckmann M, Holle JU, Arning L, Knaup S, Hellmich B, Nothnagel M, et al. The Wegener’s granulomatosis quantitative trait locus on chromosome 6p21.3 as characterized by tagSNP genotyping. Ann Rheum Dis. 2008;67:972–9.
Gonzalez-Galarza FF, Takeshita LY, Santos EJ, Kempson F, Maia MH, da Silva AL, et al. Allele frequency net 2015 update: new features for HLA epitopes, KIR and disease and HLA adverse drug reaction associations. Nucleic Acids Res. 2015;43:D784–D788.
Lyons PA, Rayner TF, Trivedi S, Holle JU, Watts RA, Jayne DR, et al. Genetically distinct subsets within ANCA-associated vasculitis. N Engl J Med. 2012;367:214–23.
Xie G, Roshandel D, Sherva R, Monach PA, Lu EY, Kung T, et al. Association of granulomatosis with polyangiitis (Wegener’s) with HLA-DPB1*04 and SEMA6A gene variants: evidence from genome-wide analysis. Arthritis Rheum. 2013;65:2457–68.
Merkel PA, Xie G, Monach PA, Ji X, Ciavatta DJ, Byun J, et al. Identification of functional and expression polymorphisms associated with risk for antineutrophil cytoplasmic autoantibody-associated vasculitis. Arthritis Rheumatol. 2017;69:1054–66.
Mahr AD, Edberg JC, Stone JH, Hoffman GS, St Clair EW, Specks U, et al. Alpha1-antitrypsin deficiency-related alleles Z and S and the risk of Wegener’s granulomatosis. Arthritis Rheum. 2010;62:3760–7.
Teruel M, Alarcon-Riquelme ME. The genetic basis of systemic lupus erythematosus: what are the risk factors and what have we learned. J Autoimmun. 2016;74:161–75.
Kawasaki A, Kyogoku C, Ohashi J, Miyashita R, Hikami K, Kusaoi M, et al. Association of IRF5 polymorphisms with systemic lupus erythematosus in a Japanese population: support for a crucial role of intron 1 polymorphisms. Arthritis Rheum. 2008;58:826–34.
Kawasaki A, Ito I, Hikami K, Ohashi J, Hayashi T, Goto D, et al. Role of STAT4 polymorphisms in systemic lupus erythematosus in a Japanese population: a case-control association study of the STAT1-STAT4 region. Arthritis Res Ther. 2008;10:R113; https://doi.org/10.1186/ar2516.
Ito I, Kawaguchi Y, Kawasaki A, Hasegawa M, Ohashi J, Kawamoto M, et al. Association of the FAM167A-BLK region with systemic sclerosis. Arthritis Rheum. 2010;62:890–5.
Shimane K, Kochi Y, Horita T, Ikari K, Amano H, Hirakata M, et al. The association of a nonsynonymous single-nucleotide polymorphism in TNFAIP3 with systemic lupus erythematosus and rheumatoid arthritis in the Japanese population. Arthritis Rheum. 2010;62:574–9.
Shimane K, Kochi Y, Suzuki A, Okada Y, Ishii T, Horita T, et al. An association analysis of HLA-DRB1 with systemic lupus erythematosus and rheumatoid arthritis in a Japanese population: effects of *09:01 allele on disease phenotypes. Rheumatology. 2013;52:1172–82.
Kawabata Y, Ikegami H, Kawaguchi Y, Fujisawa T, Shintani M, Ono M, et al. Asian-specific HLA haplotypes reveal heterogeneity of the contribution of HLA-DR and -DQ haplotypes to susceptibility to type 1 diabetes. Diabetes. 2002;51:545–51.
Furukawa H, Kawasaki A, Oka S, Ito I, Shimada K, Sugii S, et al. Human leukocyte antigens and systemic lupus erythematosus: a protective role for the HLA-DR6 alleles DRB1*13:02 and *14:03. PLoS ONE. 2014;9:e87792; https://doi.org/10.1371/journal.pone.0087792.
Oka S, Furukawa H, Kawasaki A, Shimada K, Sugii S, Hashimoto A, et al. Protective effect of the HLA-DRB1*13:02 allele in Japanese rheumatoid arthritis patients. PLoS ONE. 2014;9:e99453; https://doi.org/10.1371/journal.pone.0099453.
Furukawa H, Oka S, Kawasaki A, Shimada K, Sugii S, Matsushita T, et al. Human leukocyte antigen and systemic sclerosis in Japanese: the sign of the four independent protective alleles, DRB1*13:02, DRB1*14:06, DQB1*03:01, and DPB1*02:01. PLoS ONE. 2016;11:e0154255; https://doi.org/10.1371/journal.pone.0154255.
Dittmer J. The role of the transcription factor Ets1 in carcinoma. Semin Cancer Biol. 2015;35:20–38.
Garrett-Sinha LA. Review of Ets1 structure, function, and roles in immunity. Cell Mol Life Sci. 2013;70:3375–90.
Russell L, Garrett-Sinha LA. Transcription factor Ets-1 in cytokine and chemokine gene regulation. Cytokine. 2010;51:217–26.
Han JW, Zheng HF, Cui Y, Sun LD, Ye DQ, Hu Z, et al. Genome-wide association study in a Chinese Han population identifies nine new susceptibility loci for systemic lupus erythematosus. Nat Genet. 2009;41:1234–7.
Yang W, Shen N, Ye DQ, Liu Q, Zhang Y, Qian XX, et al. Genome-wide association study in Asian populations identifies variants in ETS1 and WDFY4 associated with systemic lupus erythematosus. PLoS Genet. 2010;6:e1000841; https://doi.org/10.1371/journal.pgen.1000841.
Wang C, Ahlford A, Järvinen TM, Nordmark G, Eloranta ML, Gunnarsson I, et al. Genes identified in Asian SLE GWASs are also associated with SLE in Caucasian populations. Eur J Hum Genet. 2013;21:994–9.
Shan S, Dang J, Li J, Yang Z, Zhao H, Xin Q, et al. ETS1 variants confer susceptibility to ankylosing spondylitis in Han Chinese. Arthritis Res Ther. 2014;16:R87; https://doi.org/10.1186/ar4530.
Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, et al. Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis. 2007;66:222–7.
Kawasaki A, Ito S, Furukawa H, Hayashi T, Goto D, Matsumoto I, et al. Association of TNFAIP3 interacting protein 1, TNIP1 with systemic lupus erythematosus in a Japanese population: a case-control association study. Arthritis Res Ther. 2010;12:R174; https://doi.org/10.1186/ar3134.
Chung SA, Xie G, Roshandel D, Sherva R, Edberg JC, Kravitz M, et al. Meta-analysis of genetic polymorphisms in granulomatosis with polyangiitis (Wegener’s) reveals shared susceptibility loci with rheumatoid arthritis. Arthritis Rheum. 2012;64:3463–71.
Lu X, Zoller EE, Weirauch MT, Wu Z, Namjou B, Williams AH, et al. Lupus risk variant increases pSTAT1 binding and decreases ETS1 expression. Am J Hum Genet. 2015;96:731–9.
Wilde B, Thewissen M, Damoiseaux J, Hilhorst M, van Paassen P, Witzke O, et al. Th17 expansion in granulomatosis with polyangiitis (Wegener’s): the role of disease activity, immune regulation and therapy. Arthritis Res Ther. 2012;14:R227; https://doi.org/10.1186/ar4066.
Abdulahad WH, Stegeman CA, Limburg PC, Kallenberg CG. Skewed distribution of Th17 lymphocytes in patients with Wegener’s granulomatosis in remission. Arthritis Rheum. 2008;58:2196–205.
Wang D, John SA, Clements JL, Percy DH, Barton KP, Garrett-Sinha LA. Ets-1 deficiency leads to altered B cell differentiation, hyperresponsiveness to TLR9 and autoimmune disease. Int Immunol. 2005;17:1179–91.
Yamaguchi-Kabata Y, Nakazono K, Takahashi A, Saito S, Hosono N, Kubo M, et al. Japanese population structure, based on SNP genotypes from 7003 individuals compared to other ethnic groups: effects on population-based association studies. Am J Hum Genet. 2008;83:445–56.
Acknowledgments
The authors are grateful to the patients and healthy donors who participated in this study, and to the doctors who recruited patients to the projects of the Research Committee on intractable vasculitides and the Japanese RPGN Study Group of progressive renal disease, Ministry of Health, Labor and Welfare of Japan (including remission induction therapy in Japanese patients with ANCA-associated vasculitides (RemIT-JAV), remission induction therapy in Japanese patients with ANCA-associated vasculitides and rapidly progressive glomerulonephritis (RemIT-JAV-RPGN), and Japanese patients with MPO ANCA-associated vasculitis (JMAAV)) and directly to this study. This work was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI (Grant numbers 25461467 and 16K09886), Japan Agency for Medical Research and Development (AMED) “The Strategic Study Group to Establish the Evidence for Intractable Vasculitis Guideline (Grant numbers 16ek0109121h0002 and 17ek0109121s0403)” and “The Study Group for Strategic Exploration of Drug Seeds for ANCA-Associated Vasculitis and Construction of Clinical Evidence (Grant number 16ek0109104h0002 and 17ek0109104s0203)”, the Japan Rheumatism Foundation, the Japan College of Rheumatology, and the SENSHIN Medical Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FH is employed by the Department of Lifetime Clinical Immunology, Tokyo Medical and Dental University (TMDU), which has received unrestricted research grants from Chugai Pharmaceutical Co., Ltd., Ono Pharmaceuticals, Mitsubishi Tanabe Pharma Co., UCB Japan, CSL Behring, Towa Pharmaceutical Co., Ltd., Abbvie Japan Co., Ltd., Japan Blood Products Organization, Ayumi Pharmaceutical Co., and Nippon Kayaku Co., Ltd. TS received honoraria for lectures from Mitsubishi Tanabe Pharma Co., Ltd., and research grants from Mitsubishi Tanabe Pharma Co., Ltd., Chugai Pharmaceutical Co., Ltd., Astellas Pharma Co., Ltd., and Ono Pharmaceutical Co., Ltd. ST received honoraria for lectures from Pfizer, and a research grant from Chugai Pharmaceutical Co., Ltd. HM serves as a consultant for Abbvie Japan Co., Ltd. and Teijin Pharma Ltd. MH has received a research grant from Abbvie. Tokyo Women’s Medical University (TWMU), particularly the Division of Epidemiology and Pharmacoepidemiology in Rheumatic Diseases, has received unrestricted research grants from Ayumi Pharmaceutical Co., Chugai Pharmaceutical Co., Ltd., Eisai Co., Ltd., Nippon Kayaku Co., Ltd., Taisho Toyama Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., Mitsubishi Tanabe Pharma Co., and Teijin Pharma Ltd., with which TWMU paid the salary of MH. NT received 2017 Novartis—Japan Rheumatism Foundation Rheumatology Prize. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kawasaki, A., Yamashita, K., Hirano, F. et al. Association of ETS1 polymorphism with granulomatosis with polyangiitis and proteinase 3-anti-neutrophil cytoplasmic antibody positive vasculitis in a Japanese population. J Hum Genet 63, 55–62 (2018). https://doi.org/10.1038/s10038-017-0362-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s10038-017-0362-2
This article is cited by
-
An immunogenetic perspective of ANCA-associated vasculitides
Egyptian Rheumatology and Rehabilitation (2022)
-
Genetics of ANCA-associated vasculitis: role in pathogenesis, classification and management
Nature Reviews Rheumatology (2022)
-
Advances in the genomics of ANCA-associated vasculitis—a view from East Asia
Genes & Immunity (2021)