Abstract
Rapid bedside determination of cerebral blood pressure autoregulation (AR) may improve clinical utility. We tested the hypothesis that cerebral Hb oxygenation (HbDiff) and cerebral Hb volume (HbTotal) measured by near-infrared spectroscopy (NIRS) would correlate with cerebral blood flow (CBF) after single dose phenylephrine (PE). Critically ill patients requiring artificial ventilation and arterial lines were eligible. During rapid blood pressure rise induced by i.v. PE bolus, ΔHbDiff and ΔHbTotal were calculated by subtracting values at baseline (normotension) from values at peak blood pressure elevation (hypertension). With the aid of NIRS and bolus injection of indocyanine green, relative measures of CBF, called blood flow index (BFI), were determined during normotension and during hypertension. BFI during hypertension was expressed as percentage from BFI during normotension (BFI%). Autoregulation indices (ARIs) were calculated by dividing BFI%, ΔHbDiff, and ΔHbTotal by the concomitant change in blood pressure. In 24 patients (11 newborns and 13 children), significant correlations between BFI% and ΔHbDiff (or ΔHbTotal) were found. In addition, the associations between Hb-based ARI and BFI%-based ARI were significant with correlation coefficients of 0.73 (or 0.72). Rapid determination of dynamic AR with the aid of cerebral Hb signals and PE bolus seems to be reliable.
Similar content being viewed by others
Main
Intact cerebral blood pressure autoregulation (AR) describes the intrinsic ability of the brain to maintain cerebral blood flow (CBF) during changes in cerebral perfusion pressure. Diverse factors, such as age of patient, illness, injury, or vasoactive drugs, have been found to impair this ability—often to an unpredictable extent. Patients with impaired or even absent AR are at increased risk for inadequate CBF and consequently for cerebral ischemia. Measuring AR may provide clinically useful information and permit more individualized critical care. Several recent studies have demonstrated the potential of so-called dynamic AR to predict outcome in adult (1) or pediatric TBI (2) and in premature infants (3). In addition, monitoring of dynamic AR may allow determination of optimal cerebral perfusion pressure (4) and determination of treatment efficacy in controlling intracranial pressure (ICP) after head injury (5). Finally, AR-guided treatment of cerebral perfusion pressure in patients suffering severe head trauma carries the potential to improve outcome (6) and has therefore been recommended in the new adult guidelines (7). Nevertheless, further work is needed to delineate the clinical utility of AR determination in critical illness, especially for the child and newborn.
Determination of the classic, steady state (or static) AR in intensive care medicine remains cumbersome and time consuming. In contrast, determination of the short-latency cerebrovascular response (or dynamic AR) to rapid perfusion pressure changes has been shown to be easily performed at the bedside and allows for repetitive measures. Several studies have shown that the findings of dynamic AR are associated with the results of static AR (8,9). Dynamic AR may be defined as an acute change in vascular resistance (10) or arteriolar caliber (11) due to acute perfusion pressure changes. This leads to acute changes in CBF, cerebral blood volume (CBV), and ICP (12). In a previous study, we have demonstrated that after a single dose of phenylephrine (PE) to increase mean arterial blood pressure (MABP), the near-infrared spectroscopy(NIRS)-derived Hb signals correlated well with ICP as a surrogate for CBV (13). NIRS-measured Hb signals after rapid increase in MABP may not only correlate with ICP but also with CBF. Therefore, aim of the study was to investigate whether noninvasive NIRS-measured Hb signals may correlate with CBF measures and may allow reliable determination of dynamic AR after i.v. PE bolus.
METHODS
Patients.
All patients admitted to the neonatal and pediatric ICU were consecutively screened on a daily basis over a 14-mo period. Patients requiring invasive ventilation, invasive arterial blood pressure monitoring, and central venous catheter due to the underlying pathology were eligible for the study. Exclusion criteria were active bleeding, hyperbilirubinemia and phototherapy, extrapulmonary cardiovascular shunts, liver dysfunction with hypoglycemia and hyperammonemia, iodine allergy, unstable cardiopulmonary situation, or intracranial hemorrhage. All patients presenting with neurological abnormalities had appropriate imaging. Once the patient fulfilled all criteria, written informed consent was obtained from parents. The study had been approved by the ethic committee of the state of Berne.
Dynamic AR determination was performed when baseline MABP was within normal range of age, end-tidal carbon dioxide (EtCO2) stable and at low normocapnic range as determined by arterial Pco2, and transcutaneous oxygen saturation (StO2) >96%. Normality of the “milieu intérieur” was confirmed by determination of blood glucose and electrolytes, arterial pH, Hb, and rectal temperature. Testing did not require additional sedation or neuromuscular paralysis of the patient. However, during most AR testing, patients were sedated with a continuous infusion of an opioid or midazolam.
Near-infrared spectroscopy.
This study was conducted with a four wavelength spectrometer (NIRO 500; Hamamatsu Photonics, Japan), which is unable to measure photon path length and therefore unable to quantify absolute tissue chromophores concentration. However, because path length is constant for any given subject after optodes are placed, absolute concentration changes from an arbitrary zero are measured. In addition, the emitted light intensity at the skin surface (power density of maximal 0.05 mW/mm2) is far below those permitted by the International Electrotechnical Commission allowing for safe application of the photosensitive indocyanine green (ICG) dye during NIRS measurements.
The application of Niro 500 has been described earlier (13,14). In this study, two fiberoptic bundles for conveying near-infrared light were placed over the frontotemporal region of the head. Optodes were positioned at 4–5 cm from each other and fixed to the skin by using adhesive rings and elastic bands. After the optode placement, the head was covered with a light-impermeable drape. Light from pulsed laser diodes was conducted through the emitting optode into the forehead. Transmitted light was collected by the detecting optode attached to a photomultiplier tube. The number of received photons at each wavelength (775, 830, 850, and 905 nm) was compared with the light output of the four lasers. With the help of extinction coefficients of the three chromophores, oxygenated Hb (HbO2), deoxygenated Hb, and ICG at each wavelength (Table 1), specific attenuation is presented online at 2 Hz with software ONMAIN (version 1.32b; Hamamatsu Photonics, Japan). The unit of NIRS signals was chosen to be OD. HbDiff was calculated as HbO2 minus Hb and defined as cerebral Hb oxygenation. HbTotal was calculated as the sum of HbO2 and Hb and defined as cerebral Hb volume. With constant hematocrit, changes in HbTotal are indicative of CBV changes.
Dynamic AR by cerebral Hb signal.
AR was assessed by i.v. bolus of PE through a central venous catheter to rapidly and transiently elevate blood pressure at least by 10% and maximally by 25% while continuously displaying (and simultaneously storing on a personal computer) HbDiff, HbTotal, MABP, StO2, and EtCO2. The PE dose needed to reach the target blood pressure elevation was carefully determined in each patient by stepwise dose increase, starting from 0.5 μg/kg. Subsequent data analysis was performed using custom software program (Labview 5.0; National Instruments, Austin, TX). Two time series were defined by the arterial blood pressure behavior as previously described (13) (Fig. 1). The first time series included a baseline of 60 s (normotension) ending with the start of blood pressure rise. This relatively long baseline period was chosen to minimize the effect of the physiological slow wave motion of cerebral vessels. The blood pressure increase from start to peak elevation lasted 15 s on average. The second time series (hypertension) started at the highest blood pressure elevation and lasted 5 s. This short time interval was chosen because of the short-lived peak blood pressure elevation after central PE bolus in pediatric patients. Each 60 s interval of MABP, StO2, EtCO2, HbDiff, and HbTotal at baseline was averaged and used as normotension value. At the highest blood pressure elevation, the 5-s interval of the signals was averaged and used as hypertension value. Each signal change was then calculated by subtracting normotension value from hypertension value (e.g. ΔHbDiff = averaged HbDiff at hypertension − averaged HbDiff at normotension). Finally, an cerebral autoregulation index (ARI) was calculated by dividing the changes in HbDiff or HbTotal by the concomitant change in MABP and expressed as either ARIHbDiff or ARIHbTotal. Such ARI is the amount of relative CBF change per millimeters of mercury MABP change. A negative ARI value means a CBF decrease at MABP peak elevation and reflects an active cerebrovascular reactivity and intact AR (Fig. 1). A positive ARI value means an CBF increase at MABP peak elevation and therefore a diminished cerebrovascular reactivity and impaired AR.
Dynamic AR by blood flow index.
ICG absorbs near-infrared light with an absorption peak around 805 nm and is strongly protein bound in blood. This enables monitoring of the passage of an injected ICG bolus through the cerebral vasculature by NIRS. Moreover, its rapid clearance from blood by hepatic uptake and biliary excretion combined with documented nontoxicity (15) makes ICG a suitable tracer for repetitive measurements at short intervals and good reproducibility (14). The blood flow index (BFI) method is a tissue blood flow determination developed by Perbeck et al. (16) from fluorescein flowmetry in the intestine. BFI was calculated from dye kinetics of each bolus ICG injection according to the algorithm BFI = maximum change in ICG absorption (ΔICGmax indicated in OD) divided by rise time. The rise time was defined by the time in seconds between 10% of ΔICGmax and 90% of ΔICGmax. ΔICGmax was calculated from a baseline value (mean of 15 s baseline before rise) subtracted from peak value (Fig. 2). Three BFI were taken during normotension, 5 min apart from each other, and averaged as BFInormotension. Then, three BFI were measured during hypertension following three PE boluses, 5 min apart, and averaged as BFIhypertension, and expressed as percentage of BFInormotension (BFI%). We chose to express BFI changes as BFI%, because BFI is as relative measure of CBF, where all constants are excluded from calculation. That means that BFI is proportional to CBF with an unknown factor of proportionality to absolute CBF numbers (14). In addition, the autoregulation index ARIBFI% was calculated by subtracting 100 from BFI% and then dividing by the concomitant change in MABP. Negative ARIBFI% values stand for intact AR and positive values for impaired AR. For BFI measurements, the central venous line was first loaded with 0.1 mg/kg body weight of ICG (Pulsion, Germany) at a concentration of 2.5 or 5 mg/mL to keep the amount of dye smaller than the dead space of the catheter and then flushed with 1 to 5 mL isotonic saline depending on the size of central venous catheter. Both ICG and flush fluids were at 37°C. For one dynamic AR by BFI (ARBFI) determination, the same central venous line, the same amount, and dilution of tracer and flush were used. The patient parameters MABP, StO2, and EtCO2 were averaged for 5 s during each BFI measurement; then the mean at normotension or hypertension conditions were calculated.
As ICG may interfere with the interpretation of Hb signal (17) because of its much higher OD changes, dynamic AR by cerebral Hb signal (ARHb) was measured first, immediately followed by ARBFI. NIRS optodes were left in place, and patient physiological parameters were kept as similar as possible during both AR determinations.
Statistics.
As ΔHbDiff (Shapiro Wilk test statistic = 0.904; p = 0.025) and part of the physiological patient parameters were nonnormally distributed, and because of the small number of patients studied, nonparametric exact tests were used whenever possible, and medians together with interquartile ranges (IQR) were calculated as summary measures (StatXact 6.0; Cytel Software Corp., Cambridge, MA). Calculation of Spearman's rank correlation coefficient with its 95% CI was used to assess associations between the changes in Hb signals (ΔHbDiff and ΔHbTotal) and changes in BFI (BFI%). Calculation of Spearman's rank correlation coefficient was also used to assess associations between ARIHbDiff (or ARIHbTotal) and ARIBFI%.
Wilcoxon's signed-rank test was used to assess whether there were differences in the physiological parameters between ARHb and ARBFI, such as differences in baseline values of MABP, StO2, or EtCO2, and differences in chances of MABP, StO2, or EtCO2. In addition, calculation of Spearman's rank correlation coefficient was used to assess associations between these potentially confounding differences in physiological parameters and the ARIs. Two-sided tests were used throughout, and p < 0.050 were considered significant.
RESULTS
Twenty-seven children had ARHb and ARBFI measured. Three of them were not included in the analysis because of unstable blood pressure after chlorpromazine, abnormal tracer kinetics secondary to residual shunting, and prolonged ICG elimination time secondary to ischemic hepatopathy in each. We thus report on the results of 24 children (Table 2), 15 boys and 9 girls. Eleven were neonates with GAs >36 wk, whereas 13 were older (2 mo to 15 y). Their main diagnoses were either cranial pathologies [six perinatal asphyxia, four severe head trauma (one death), one stroke, and one meningitis] or noncranial pathologies (five surgery of congenital heart disease, three sepsis, two repair of congenital diaphragmatic hernia, one hyaline membrane disease, and one bronchiolitis). All patients had three BFI determinations at normotension and three BFI at hypertension, except for three patients who had only two BFI determination because of time restrains.
The physiological parameters EtCO2 and StO2 remained stable throughout the experiments. Their median changes from baseline to hypertension, and the differences between the two AR determinations were <0.5 mm Hg EtCO2 or 0.5% StO2 and were all nonsignificant (data not presented except for EtCO2 at baseline). Median ΔMABP was 11.9 mm Hg (IQR, 10.3 to 15.4) during ARHb and 9.5 mm Hg (IQR, 6.9 to 13.6) during ARBFI. The median blood pressure increase was 17.6% (IQR, 15.2 to 30.4) for ARHb and 15.0% (11.2 to 22.5) for ARBFI. Between the two AR determinations, MABP at baseline was comparable (median difference, −0.5 mm Hg; IQR, −1.8 to 1.2; p = 0.86), but ΔMABP was higher during determination of ARHb when compared with ΔMAB during ARBFI (median difference, 1.7 mm Hg; IQR, 0.4 to 4.6; p = 0.003). However, there was no association found between these differences in ΔMABP and the three ARI (nonsignificant Spearman rank correlation coefficients).
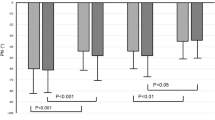
We found high positive correlations between changes in Hb signals (ΔHbDiff and ΔHbTotal) and changes in BFI expressed as BFI% (Fig. 3). The Spearman's rank correlation coefficient ρ between ΔHbDiff and BFI% was 0.78 (95% CI, 0.65 to 0.92; p < 0.001) and between ΔHbTotal and BFI% was 0.73 (95% CI, 0.51 to 0.95; p < 0.001). In addition, we found high positive correlations between the three ARI (Fig. 4): the Spearman's rank correlation coefficient ρ between ARIHbDiff and ARIBFI% was 0.73 (95% CI, 0.53 to 0.94; p < 0.001) and between ARIHbTotal and ARIBFI% was 0.72 (95% CI, 0.51 to 0.93; p < 0.001).
Changes in Hb signals correlate with changes in CBF. NIRS measured ΔHbDiff and ΔHbTotal after rapid blood pressure rise induced by PE bolus were compared with changes in BFI expressed as BFI%. The association between ΔHbDiff (•), and BFI% was positive and highly significant (ρ = 0.78 with 95% CI, 0.65 to 0.92; p < 0.001). The association between ΔHbTotal (○) and BFI% was as well positive but slightly weaker (ρ = 0.73 with 95% CI, 0.51 to 0.95; p < 0.001).
Determination of ARI by cerebral Hb signals correlate with ARI by BFI%. After rapid blood pressure rise induced by PE bolus, ARIHbDiff and ARIHbTotal were compared with ARIBFI%. The association between ARIHbDiff (▪) and ARIBFI% was positive and high (ρ = 0.78 with 95% CI, 0.65 to 0.92; p < 0.001). The association between ARIHbTotal (□) and ARIBFI% was as well positive but slightly weaker (ρ = 0.73 with 95% CI, 0.51 to 0.95; p < 0.001).
DISCUSSION
In this study, we found a highly significant correlation between cerebral Hb signals (HbDiff and HbTotal) and direct CBF measures (BFI) after rapid blood pressure rise induced by single dose PE. Other studies have also validated NIRS-derived cerebral Hb signals during acute cerebral perfusion pressure manipulations with independent CBF measures such as CBF velocities (18,19), microspheres (20), or laser-Doppler flowmetry (21,22). All those studies support the hypothesis that Hb signals are reliable CBF surrogates during pressure maneuvers and may therefore allow assessment of dynamic AR. This is the first study to validate dynamic AR based on cerebral Hb signals and after an induced rapid blood pressure rise. We found significant correlations between the autoregulation indices ARIHbDiff, ARIHbTotal, and ARIBFI%, which confirm the hypothesis that during such blood pressure increase, determination of AR based on cerebral Hb signals may be reliable.
The notion of cerebral Hb signals being surrogates of CBF has led investigators to use the associative relationship between continuously monitored cerebral Hb signals and spontaneous fluctuations in arterial blood pressure for dynamic AR determination by analysis in the frequency domain (3,23,24) or by analysis in the time domain (25–27). In addition, Brady et al. (25) and Lee et al. (26) verified the reliability of such AR determination by NIRS with AR determination by laser Doppler flowmetry during slow induction of hypotension in anesthetized piglets. Using spontaneous fluctuations for assessment of dynamic AR seems clinically attractive, because it does not require any additional blood pressure manipulation. Such technique is based on the presence of CBF waves preferably at 0.004 to 0.05 Hz with enough frequency and amplitude. These physiological, very slow waves are probably part of the well-described spontaneous oscillations or vasomotion of the cerebral vasculature, which are regulated not only by myogenic (or transmural pressure) but also by neurogenic and metabolic factors. Vasomotion has been shown to disappear, e.g. under inhalational anesthetics, hypercapnia, or ischemia (28). It is therefore obvious that this AR technique runs the risk to have low signal-to-noise ratios and has shown in clinical settings to require prolonged sampling times, extensive averaging, or incorporation of exclusion rules for adequate AR calculation (3,23–27). In contrast to dynamic AR determinations based on spontaneous blood pressure fluctuations, the PE technique is performed faster, has a better signal-to-noise ratio, and evaluates only CBF-changes specific to systemic blood pressure changes. Comparison of the two dynamic AR techniques has not been done as of now.
PE is commonly used for evaluation of static AR, because this α-1 vasoconstrictor is supposed to have no direct effect on the cerebral vasculature. For dynamic AR determination in contrast, this study and our previous study (13) are the only two studies using PE bolus. The classic maneuver for dynamic AR determination has been induction of a transient blood pressure fall by thigh cuff release (8). However, the maneuver of rising systemic blood pressure transiently seems to be less of a risk than lowering blood pressure for most critically ill children and neonates at a time when the brain may least be able to tolerate blood pressure drops and when blood pressure is typically in the lower range of normal. However, uncontrolled hypertension may provoke intracranial hemorrhage, especially in the premature infant (29). To minimize such risk, we aimed to increase blood pressure only by 10 to 25%, an increase which is within the physiological range of spontaneous blood pressure variations seen in the ventilated neonate and child. Because ΔMABP did not contribute significantly to the linear association between ARIs, we speculate that even lower doses of PE with less increase in systemic blood pressure may already suffice for dynamic AR determination.
Transcranial Doppler flow velocity is an established technique for bedside assessment of short latency CBF changes. A clinically attractive alternative is the NIRS-based determination of BFI as a relative but very rapid CBF measurement within a few seconds. BFI has a good reproducibility (14) and has been validated in diverse studies, where it showed significant correlations with CBF measured by microspheres and by transcranial Doppler ultrasound during hemorrhagic shock (30,31) and during antegrade selective cerebral perfusion (32). One clinical study, in contrast, found no correlation between BFI and 133Xenon clearance techniques (33). However, in that study, BFI was not considered as relative measure of CBF. Nevertheless, published interindividual variations of BFI measurements remain in all studies rather large despite high accuracy when using BFI for intraindividual repetitive CBF measurements over time (34).
We believe that the unique technique of dynamic AR assessment by i.v. PE bolus makes noninvasive NIRS measured Hb signals especially sensitive to intracerebral chromophores changes with little extracerebral contamination. This technique should have a high specificity for detection of AR impairment, which is the clinically important aspect: an increase in HbDiff or HbTotal during blood pressure rise can only be secondary to intracerebral vasodilatation because all extracerebral vessel vasoconstrict under the effect of the selective alpha-1 agonist PE. In addition, during this very rapid AR determination time of <2 min, cerebral Hb concentration changes other than due to CBF (such as due to Hb or oyxgen metabolic rate) should be minimal. Nevertheless, despite the significant correlations between the ARI, rather large interindividual variabilities occur. These are probably not only because of imperfect timing of BFI determination at peak blood pressure elevation but are also due to limited spacial resolution and limited absolute quantification of the NIRS instrument used in this study. There is hope that by using the new generation of NIRS instruments (35) the accuracy may increase.
In this study, ARI is defined by CBF change per MABP change, a definition widely used for dynamic AR (3,8). This definition differs from classic AR relating CBF to CPP and not to MABP. Indeed, the role of ICP in the assessment of dynamic AR remains controversial. However, the three studies comparing dynamic AR determination by CPP or by MABP found significant agreement between both methods (26,36,37). These results support the notion that MABP may reliably replace CPP or ICP for noninvasive assessment of dynamic AR.
In conclusion, noninvasive NIRS and single dose PE allows for reliable determination of dynamic AR. This rapidly performed test combined with simple bedside interpretation may motivate clinicians for large-scale dynamic AR evaluation in clinical settings and may help to further delineate the value of knowing the actual state of dynamic AR in intensive care management.
Abbreviations
- AR:
-
cerebral blood pressure autoregulation
- ARHb:
-
dynamic autoregulation by cerebral hemoglobin signal
- ARBFI:
-
dynamic autoregulation by blood flow index
- ARI:
-
cerebral autoregulation index
- ARIBFI%:
-
ARI defined by BFI%
- ARIHbDiff:
-
ARI defined by HbDiff
- ARIHbTotal:
-
ARI defined by HbTotal
- BFI:
-
blood flow index
- BFI%:
-
BFI during hypertension expressed as percentage of BFI during normotension
- CBV:
-
cerebral blood volume
- CBF:
-
cerebral blood flow
- EtCO2:
-
end-tidal carbon dioxide
- Hb:
-
deoxygenated hemoglobin
- HbO2:
-
oxygenated hemoglobin
- HbDiff:
-
cerebral hemoglobin oxygenation: HbO2 minus Hb
- HbTotal:
-
cerebral hemoglobin volume: HbO2 plus Hb
- ICP:
-
intracranial pressure
- ICG:
-
indocyanine green
- ΔICGmax:
-
ICG baseline value subtracted from ICG peak value
- IQR:
-
interquartile range
- MABP:
-
mean arterial blood pressure
- NIRS:
-
near-infrared spectroscopy
- StO2:
-
transcutaneous oxygen saturation
REFERENCES
Czosnyka M, Smielewski P, Kirkpatrick P, Laing RJ, Menon D, Pickard JD 1997 Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery 41: 11–17
Vavilala MS, Lee LA, Boddu K, Visco E, Newell DW, Zimmerman JJ, Lam AM 2004 Cerebral autoregulation in pediatric traumatic brain injury. Pediatr Crit Care Med 5: 257–263
Wong FY, Leung TS, Austin T, Wilkinson M, Meek JH, Wyatt JS, Walker AM 2008 Impaired autoregulation in preterm infants identified by using spatially resolved spectroscopy. Pediatrics 121: e604–e611
Steiner LA, Czosnyka M, Piechnik SK, Smielewski P, Chatfield D, Menon DK, Pickard JD 2002 Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med 30: 733–738
Oertel M, Kelly DF, Lee JH, McArthur DL, Glenn TC, Vespa P, Boscardin WJ, Hovda DA, Martin NA 2002 Efficacy of hyperventilation, blood pressure elevation, and metabolic suppression therapy in controlling intracranial pressure after head injury. J Neurosurg 97: 1045–1053
Howells T, Elf K, Jones PA, Ronne-Engström E, Piper I, Nilsson P, Andrews P, Enblad P 2005 Pressure reactivity as a guide in the treatment of cerebral perfusion pressure in patients with brain trauma. J Neurosurg 102: 311–317
Bratton SL, Chestnut RM, Ghajar J, McConell Hammond FF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, Schouten J, Shutter L, Timmons SD, Ullman JS, Videtta W, Wilberger JE, Wright DW 2007 Cerebral perfusion thresholds. J Neurotrauma 24: S59–S64
Tiecks FP, Lam AM, Aaslid R, Newell DW 1995 Comparison of static and dynamic cerebral autoregulation measurements. Stroke 26: 1014–1019
Steiner LA, Coles JP, Johnston AJ, Chatfield DA, Smielewski P, Fryer TD, Aigbirhio FI, Clark JC, Pickard JD, Menon DK, Czosnyka M 2003 Assessment of cerebrovascular autoregulation in head-injured patients: a validation study. Stroke 34: 2404–2409
Paulson OB, Strandgaard S, Edvinsson L 1990 Cerebral autoregulation. Cerebrovasc Brain Metab Rev 2: 161–192
Bayliss WM 1902 On the local reactions of the arterial wall to changes of internal pressure. J Physiol 28: 220–231
Green HD, Rapela CE 1964 Blood flow in passive vascular beds. Circ Res 15: S11–S16
Wagner BP, Pfenninger J 2002 Dynamic cerebral autoregulatory response to blood pressure rise measured by near-infrared spectroscopy and intracranial pressure. Crit Care Med 30: 2014–2021
Wagner BP, Gertsch S, Ammann RA, Pfenninger J 2003 Reproducibility of the blood flow index as noninvasive, bedside estimation of cerebral blood flow. Intensive Care Med 29: 196–200
Keller E, Ishihara H, Nadler A, Niederer P, Seifert B, Yonekawa Y, Frei K 2002 Evaluation of brain toxicity following near infrared light exposure after indocyanine green dye injection. J Neurosci Methods 117: 23–31
Perbeck L, Lund F, Svensson L, Thulin L 1985 Fluorescein flowmetry: a method for measuring relative capillary blood flow in the intestine. Clin Physiol 5: 281–292
De Visscher G, Van Rossem K, Van Reempts J, Borgers M, Flameng W, Reneman RS 2002 Cerebral blood flow assessment with indocyanine green bolus transit detection by near-infrared spectroscopy in the rat. Comp Biochem Physiol A Mol Integr Physiol 132: 87–95
Tsuji M, duPlessis A, Taylor G, Crocker R, Volpe JJ 1998 Near infrared spectroscopy detects cerebral ischemia during hypotension in piglets. Pediatr Res 44: 591–595
Al-Rawi PG, Smielewski P, Kirkpatrick PJ 2001 Evaluation of a near-infrared spectrometer (NIRO 300) for the detection of intracranial oxygenation changes in the adult head. Stroke 32: 2492–2500
Soul JS, Taylor GA, Wypij D, Duplessis AJ, Volpe JJ 2000 Noninvasive detection of changes in cerebral blood flow by near-infrared spectroscopy in a piglet model of hydrocephalus. Pediatr Res 48: 445–449
Kurth CD, Levy WJ, McCann J 2002 Near-infrared spectroscopy cerebral oxygen saturation thresholds for hypoxia-ischemia in piglets. J Cereb Blood Flow Metab 22: 335–341
Pryds A, Tønnesen J, Pryds O, Knudsen GM, Greisen G 2005 Cerebral pressure autoregulation and vasoreactivity in the newborn rat. Pediatr Res 57: 294–298
Bassan H, Gauvreau K, Newburger JW, Tsuji M, Limperopoulos C, Soul JS, Walter G, Laussen PC, Jonas RA, du Plessis AJ 2005 Identification of pressure passive cerebral perfusion and its mediators after infant cardiac surgery. Pediatr Res 57: 35–41
Soul JS, Hammer PE, Tsuji M, Saul JP, Bassan H, Limperopoulos C, Disalvo DN, Moore M, Akins P, Ringer S, Volpe JJ, Trachtenberg F, du Plessis AJ 2007 Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res 61: 467–473
Brady KM, Lee JK, Kibler KK, Smielewski P, Czosnyka M, Easley RB, Koehler RC, Shaffner DH 2007 Continuous time-domain analysis of cerebrovascular autoregulation using near-infrared spectroscopy. Stroke 38: 2818–2825
Lee JK, Kibler KK, Benni PB, Easley RB, Czosnyka M, Smielewski P, Koehler RC, Shaffner DH, Brady KM 2009 Cerebrovascular reactivity measured by near-infrared spectroscopy. Stroke 40: 1820–1826
Steiner LA, Pfister D, Strebel SP, Radolovich D, Smielewski P, Czosnyka M 2009 Near-infrared spectroscopy can monitor dynamic cerebral autoregulation in adults. Neurocrit Care 10: 122–128
Hudetz AG, Biswal BB, Shen H, Lauer KK, Kampine JP 1998 Spontaneous fluctuations in cerebral oxygen supply. An introduction. Adv Exp Med Biol 454: 551–559
Goddard J, Lewis RM, Armstrong DL, Zeller RS 1980 Moderate, rapidly induced hypertension as a cause of intraventricular hemorrhage in the newborn beagle model. J Pediatr 96: 1057–1060
Kuebler WM, Sckell A, Habler O, Kleen M, Kuhnle GE, Welte M, Messmer K, Goetz AE 1998 Noninvasive measurement of regional cerebral blood flow by near-infrared spectroscopy and indocyanine green. J Cereb Blood Flow Metab 18: 445–456
Bein B, Meybohm P, Cavus E, Tonner PH, Steinfath M, Scholz J, Doerges V 2006 A comparison of transcranial doppler with near infrared spectroscopy and indocyanine green during hemorrhagic shock: a prospective experimental study. Crit Care 10: R18
Meybohm P, Hoffmann G, Renner J, Boening A, Cavus E, Steinfath M, Scholz J, Bein B 2008 Measurement of blood flow index during antegrade selective cerebral perfusion with near-infrared spectroscopy in newborn piglets. Anesth Analg 106: 795–803
Schytz HW, Wienecke T, Jensen LT, Selb J, Boas DA, Ashina M 2009 Changes in cerebral blood flow after acetazolamide: an experimental study comparing near-infrared spectroscopy and SPECT. Eur J Neurol 16: 461–467
Kuebler WM 2008 How NIR is the future in blood flow monitoring?. J Appl Physiol 104: 905–906
Wolf M, Ferrari M, Quaresima V 2007 Progress of near-infrared spectroscopy and topography for brain and muscle clinical applications. J Biomed Opt 12: 062104
Lang EW, Lagopoulos J, Griffith J, Yip K, Mudaliar Y, Mehdorn HM, Dorsch NW 2003 Noninvasive cerebrovascular autoregulation assessment in traumatic brain injury: validation and utility. J Neurotrauma 20: 69–75
Czosnyka M, Smielewski P, Lavinio A, Pickard JD, Panerai R 2008 An assessment of dynamic autoregulation from spontaneous fluctuations of cerebral blood flow velocity: a comparision of two models, index of autoregulation and mean flow index. Anesth Analg 106: 234–239
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Department of Clinical Research, University of Berne, and the Swiss National Science Foundation (grant 32-51078.97).
Rights and permissions
About this article
Cite this article
Wagner, B., Ammann, R., Bachmann, D. et al. Rapid Assessment of Cerebral Autoregulation by Near-Infrared Spectroscopy and a Single Dose of Phenylephrine. Pediatr Res 69, 436–441 (2011). https://doi.org/10.1203/PDR.0b013e3182110177
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3182110177
This article is cited by
-
Ipsi- and contralateral frontal cortex oxygenation during handgrip task does not follow decrease on maximal force output
Journal of Physiological Anthropology (2015)