Abstract
Backround
Microcephaly can either be isolated or it may coexist with other neurological entities and/or multiple congenital anomalies, known as syndromic microcephaly. Although many syndromic cases can be classified based on the characteristic phenotype, some others remain uncertain and require further investigation. The present study describes the application of array-comparative genomic hybridization (array-CGH) as a diagnostic tool for the study of patients with clinically unknown syndromic microcephaly.
Methods
From a cohort of 210 unrelated patients referred with syndromic microcephaly, we applied array-CGH analysis in 53 undiagnosed cases. In all the 53 cases except one, previous standard karyotype was negative. High-resolution 4 × 180K and 1 × 244K Agilent arrays were used in this study.
Results
In 25 out of the 53 patients with microcephaly among other phenotypic anomalies, array-CGH revealed copy number variations (CNVs) ranging in size between 15 kb and 31.6 Mb. The identified CNVs were definitely causal for microcephaly in 11/53, probably causal in 7/53, and not causal for microcephaly in 7/53 patients. Genes potentially contributing to brain deficit were revealed in 16/53 patients.
Conclusions
Array-CGH contributes to the elucidation of undefined syndromic microcephalic cases by permitting the discovery of novel microdeletions and/or microduplications. It also allows a more precise genotype–phenotype correlation by the accurate definition of the breakpoints in the deleted/duplicated regions.
Similar content being viewed by others
Main
Microcephaly is defined as an occipitofrontal head circumference, which is 2 or more SDs below the mean (−2 SD) for age and sex. It results from the premature fusion of the cranial sutures due to impaired neurogenesis. Most countries have created their own standard growth curves for term and preterm infants according to sex and age. Many classifications regarding microcephaly have been proposed by experts. The most accurate classification is the one that is based on the time of onset, and it defines microcephaly as congenital or postnatal (1). Both categories can be due to genetic or non-genetic factors. Nevertheless, genetic factors are more frequently responsible for congenital microcephaly, whereas non-genetic factors often cause postnatal microcephaly.
Non-genetic factors, such as radiation, smoking, alcohol, intrauterine hypoxemia, antiepileptic drugs, poorly controlled maternal phenylketonuria or diabetes, and congenital infections due to rubella, cytomegalovirus, toxoplasmosis, and herpes virus, may affect the infant prenatally. Other causes including respiratory distress, hypoxic-ischemic encephalopathy, hyperthermia, central nervous system infections, and intracranial bleeding can potentially influence the infant perinatally, whereas malnutrition, congenital heart diseases, and chronic diseases can cause microcephaly, which presents postnatally (2).
Microcephaly due to genetic causes includes isolated and syndromic microcephaly, various metabolic diseases, Fanconi anemia, primary craniosynosteosis, and brain malformations. Syndromic microcephaly is associated with other neurological entities and/or dysmorphic features or multiple congenital anomalies. It may be due to an autosomal-dominant or -recessive disorder, an X-linked-dominant or -recessive defect, numerical chromosomal abnormalities, structural chromosomal abnormalities of >5–10 Mb detected by conventional Karyotype, and submicroscopic genomic rearrangements identified by high-throughput molecular technologies (2). In the present study, we describe the extensive application of array comparative genomic hybridization (array-CGH) in patients with unexplained syndromic microcephaly and discuss the clinical interpretation of genotype–phenotype correlation.
Methods
Subjects
From a cohort of 210 patients with syndromic microcephaly who were referred for genetic evaluation during a 4-year period, we applied array-CGH in 53 undiagnosed cases in order to identify genetic causes of microcephaly. The study is both retrospective and prospective and has received approval from the Ethical Committee of “Aghia Sophia” Children’s Hospital.
The selection of the 53 patients was based on a well-standardized five-step protocol:
Step 1: (i) Detailed personal history including obstetric and perinatal history. (ii) Detailed parental and family history.
Step 2: Detailed physical examination and genetic evaluation carried out by experienced clinical geneticists.
Step 3: Developmental, neurological—including brain MRI and cardiological, opthalmological, and audiological evaluations in all patients.
Step 4: (i) In all patients, clinical and/or laboratory exclusion of the following medical conditions: non-genetic causes of microcephaly, craniosynosteosis, and metabolic diseases. Patients with the three most common numerical chromosomal aberrations (trisomy 21, trisomy 13, and trisomy 18) were not included in the present study. In all cases, except one, previous standard karyotype was normal. (ii) In a number of patients, according to their phenotype, targeted genetic investigation for monogenic microcephaly syndromes, such as Angelman, Rett, and Cornelia de Lange syndrome, was performed.
Step 5: Further investigation by array-CGH was performed: (i) in five patients with characteristic phenotype who were clinically suspected of having a well-known syndrome such as Wolf Hircshhorn syndrome and DiGeorge syndrome and (ii) in 53 undiagnosed cases in order to identify genetic causes of microcephaly.
We define microcephaly, the occipitofrontal head circumference, which is 2 or more SDs below the mean (-2SD) for age and sex.
Informed written consent was obtained from the parents of all the patients participating in the study.
Array-CGH Analysis
Genomic DNA from 58 patients and their parents was obtained from 3 ml of peripheral blood using the BioRobot M48 System (Qiagen, Hilden, Germany) and the commercially available kit MagAttract DNA Blood Midi M48 Kit (Qiagen). The quality and quantity of the DNA samples was determined using a NanoDrop ND-1000 UV–VIS spectrophotometer. High-resolution 4 × 180 K and 1 × 244 K Agilent SurePrint G3 arrays (>170,000 and >236,000 probes, respectively, average resolution >8.9 kb) were used in this study (Agilent Technologies, Santa Clara, CA, www.agilent.com). Labeling, hybridization, and data processing were carried out according to the manufacturer’s recommendations and as previously described (3). The benign CNVs (or copy number polymorphisms) reported in the Database for Genomic Variants (http://dgv.tcag.ca/dgv/app/home) were removed from the results.
Further genetic analysis of genes involved in autosomal-recessive primary microcephaly (microcephaly primary hereditary) was not performed.
Results
Array comparative genomic hybridization (array-CGH) was carried out in the following way:
-
a)
In five patients with distinguishable phenotype for clinical confirmation (Table 1a—Patients 1–5). In all these cases, array-CGH confirmed the clinical diagnosis and revealed syndromes that are known to cause microcephaly. In patient No 5, fluorescence in situ hybridization analysis was pathogenic, but because of the severe phenotype, array-CGH was performed to exclude the coexistence of other pathogenic copy number variations (CNVs).
Table 1a CNVs in patients with syndromic microcephaly and suspect clinical diagnosis of a microdeletion/microduplication syndrome -
b)
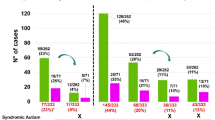
In 53 patients who presented with syndromic microcephaly of unknown etiology. In 25 out of the 53 patients (10 male/15 female patients) various chromosomal aberrations (a total of 23 microdeletions and 12 microduplications) ranging in size between 15 kb and 31.6 Mb were detected (Table 1b). Complex rearrangements contributed to the overall clinical phenotype in 10 out of the 25 patients. In all the 25 patients, microcephaly was accompanied by dysmorphic features and developmental delay/intellectual disability (mild to severe; 100%). Other associated symptoms included the following: epilepsy in 5/25, hypotonia in 9/25, congenital heart disease in 4/25, and other congenital anomalies in 3/25 cases. Brain MRI was pathogenic in 12 out of the 25 patients.
Table 1b CNVs in patients with Unknown Syndromic Microcephaly
On the basis of CNV findings, we subdivided the 25 patients into the following three groups:
Group A (Table 1b, patients: 1–11): cases with CNVs related with microcephaly. The identified CNVs are known microdeletion/microduplication syndromes that have already been associated with microcephaly.
Group B (Table 1b, patients 12–18): cases with CNVs probably related with microcephaly. The CNVs include genes that could potentially contribute to the small brain size.
Group C (Table 1b, patients 19–25): cases with CNVs not related with microcephaly. On the basis of the existing literature, these CNVs have been linked with the pathologic phenotype, but they cannot explain microcephaly.
In summary, CNVs related with microcephaly were identified in 11/53 (20.75%; GROUP A), CNVs probably related with microcephaly were revealed in 7/53 (13.2%; GROUP B), and CNVs not related with microcephaly were present in 7/53 (13.2%; GROUP C) patients. In the remaining 28 out of the 53 cases (52.83%), array-CGH revealed only copy number polymorphisms and they were considered as normal.
Parental DNA samples were examined by array-CGH for all patients.
Discussion
The aim of our study was to determine the contribution of gene-dosage alterations in the etiology of unexplained microcephaly through genome-wide screening using array-CGH analysis in patients and their parents. Array-CGH is an advanced well-known high-throughput genetic diagnostic technology that allows the identification of microdeletions and microduplications not detected by G-banding karyotype and other conventional methods.
In patients 1, 2, 9, and 11 (Table 1b, GROUP A), array-CGH revealed large chromosomal alterations. In patient 1, the previous standard karyotype revealed a derivative chromosome 9 (46, XY, der (9)) and further investigation by array-CGH was performed. In the other three patients, the karyotype was normal because of low band resolution that was applied. For patients 2 and 11, conventional karyotyping was carried out in chorionic villi sample, whereas in patient 9 it was carried out in amniotic fluid.
Defects in genes that are implicated in DNA repair, DNA damage response, DNA replication, and in S-phase progression or those disrupting the microtubule network have already been suspected of causing microcephaly (4). Seltzer et al. (5) highlighted specific biological pathways associated with postnatal microcephaly, with genes implicated in the regulation of gene expression in the developing brain, in histone modification, and in GTPase signal transduction.
In accordance with the literature, we identified candidate genes that may contribute to the microcephaly phenotype in all the patients in whom array-CGH testing was performed only for clinical confirmation. The four recognized genes, WHSC1, WHSC2, SLBP, and RANBP1 (Tables 1aand 2), have already been associated with microcephaly (4, 6, 7). In 16 out of the 25 patients with unknown microcephaly and CNV findings (Table 2), we identified genes that could potentially have a significant role in small head circumference. From a total of 21 candidate genes, only 6 (FREM1, SOX1, ARHGEF7, EHMT1, CHD5, and RE(RE)) have been previously reported to be involved in brain deficit causing microcephaly (Tables 1b, and 2) (8, 9, 10, 11, 12, 13).
GROUP A: Cases with CNVs Related with Microcephaly
In 11 out of the 25 patients (No: 1–11; GROUP A, Table 1b), one or more of the identified CNVs are known microdeletion or microduplication syndromes that have already been associated with syndromic microcephaly—1p36 microdeletion, 9p duplication, 9q34.3 microdeletion (Kleefstra syndrome), 13q33-q34 microdeletion, 16q21-q22.1 microdeletion, 15q13.2 microdeletion, intermediate 1q microdeletion syndrome, and distal 4p trisomy. In patients 1 and 2, the probability of the existence of a balanced translocation in one parent was excluded, as the parental standard karyotype was normal. Genes probably contributing to microcephaly were identified in 9 out of the 11 patients with known syndromes.
9p partial duplication syndrome (patients Nos 1 and 2; GROUP A) is characterized by microcephaly, specific dysmorphic features, growth, and mental retardation. A critical region ranging from 9p22.3 to 9p22.2 is mainly responsible for the specific 9p partial trisomy phenotype (14). It is interesting that patient No 17 (GROUP B), a 3-year-old female with microcephaly of unknown onset, psychomotor retardation, and mild facial dysmorphic features has a 9p24.3 microduplication, 67.12 kb in size, containing the DOCK8 gene. DOCK8 protein belongs to the Dock-C subgroup of the Dock family of guanine nucleotide exchange factors that interact with Rho GTPases and are components of intracellular signaling networks (15). Mutations in the DOCK8 gene cause the autosomal-recessive hyper IgE recurrent infection syndrome (OMIM #243700), and DOCK8 deficiency has been reported as the cause of autosomal-dominant mental retardation type 2 (OMIM #614113). Regarding the 9p partial duplication syndrome, it has been suggested that the DOCK8 gene may contribute to the autistic spectrum disorder phenotype (14). We presume that, as the DOCK8 protein interacts with Rho GTPases, DOCK8 duplication could also have a role in microcephaly and mental retardation regarding the 9p duplication syndrome.
GROUP B: Cases with CNVs Probably Related with Microcephaly
In seven patients (No: 12-18; GROUP B, Table 1b), the identified CNVs have not been associated with microcephaly so far; however, they include genes that are implicated in genetic pathways reported as crucial for the brain and head development (4, 5).
In patient 14, a 2.5-year-old boy with severe congenital microcephaly, dysmorphic face, psychomotor retardation, hypertonia, and epilepsy, the 19p13.3 microdeletion encompasses only the following three genes: CIRBP, C19orf24, and EFNA2. The EFNA2 gene encodes a membrane-bound protein, member of the ephrin family receptor-interacting protein. It binds with ephrin receptors, which are also membrane-bound proteins via direct cell–cell interaction. The signaling pathway regulates a variety of biological processes during embryonic development including the guidance of axon growth cones, which could contribute to the small head circumference. However, previous publications (16, 17) do not support a causative role for microcephaly for these genes.
Patient 16, a 10-month-old male with postnatal microcephaly, delayed motor and cognitive skills, and multiple congenital anomalies, is the first case involving terminal 1p36 microduplication accompanied by a 22q11.2 distal deletion. 1p36 microduplications are very rare, and it is unknown whether there is any association with microcephaly (18, 19). The 22q11.2 distal deletions are recurrent genomic rearrangements located in the region immediately telomeric to the ~3 Mb common DiGeorge and Velocardiofacial deleted region (20, 21). In our patient, the small 22q11.2 microdeletion, between LCR22-5 and LCR22-6, 655.9 kb in size, encompasses the following four important genes: BCR, RAB36, GNAZ, and RTDR1. RAB36 codes a protein that is one of the essential mediators for neurite outgrowth downstream of RAB35 (ref. (22)) and may contribute to the microcephalic phenotype. Haploinsufficiency of BCR, GNAZ, and RTDR1 genes does not seem to have a role in microcephaly formation (23).
GROUP C: Cases with CNVs not Related with Microcephaly
In seven patients (Nos: 19–25; GROUP C, Table 1b), the identified CNVs include genes that could partially explain the patients’ phenotype. These CNVs have not been associated with microcephaly nor do they include genes that could contribute to reduced head circumference.
Interstitial deletions of the short arm of chromosome 12 are very rare structural anomalies. Microcephaly has been described in a number of reported patients while important genes such as SSPN, SOX5, Kras, and STK38L have also been proposed (24). Patient No 21, a 5-year-old male, presented with a phenotype resembling Floating Harbor syndrome (extremely low birth weight, short stature, postnatal microcephaly, intellectual disability, and dysmorphic features, such as triangular face, prominent nasal bridge and collumella, short philtrum, thin upper lip, and cryptorchidism). The 12p12.2p12.1 microdeletion contained only the SLCO1B3 and SLCO1B1 genes. Both genes belong to the organic anion transporter family involved in the membrane transport of bile acids, conjugated steroids, and thyroid hormones. A case has been reported in DECIPHER with a de novo 12p12.2p12.1 deletion, with similar breakpoints as our patient and phenotypic features such as intellectual disability and microcephaly (DECIPHER ID: 251269). Another patient with a similar deletion of paternal origin presented with speech delay and macrocephaly (DECIPHER ID: 282690). The 12p12.2p12.1 deletion could contribute to our patient’s clinical phenotype. However, these chromosomal aberrations are rare events.
The results of our study show that array-CGH may be considered as an invaluable diagnostic tool in patients with syndromic microcephaly. Array-CGH is a useful first-line diagnostic tool for the recognition of submicroscopic chromosomal aberrations in patients with syndromic microcephaly of unknown etiology. Further delineation of such genetic abnormalities, along with well-characterized clinical phenotypes, must be reported in order to identify new syndromes related with microcephaly and to recognize candidate genes, the haploinsufficiency of which could result in a small brain size.
In the future, the extensive application of whole-exome sequencing and whole-genome sequencing in patients with syndromic microcephaly of unknown etiology will provide more information regarding genes implicated in brain development.
References
Abuelo D . Microcephaly syndromes. Semin Pediatr Neurol 2007;14:118–27.
Von der Hagen M, Pivarcsi M, Liebe J et al, Diagnostic approach to microcephaly in childhood: a two-center study and review of the literature. Dev. Med Child Neurol 2014;56:732–41.
Tzetis M, Kitsiou-Tzeli S, Frysira H, Xaidara A, Kanavakis E . The clinical utility of molecular karyotyping using high-resolution array-comparative genomic hybridization. Expert Rev Mol Diagn 2012;12:449–57.
Kerzendorfer C, Colnaghi R, Abramowicz I, Carpenter G, O'Driscoll M . Meier-Gorlin syndrome and Wolf-Hirschhorn syndrome: two developmental disorders highlighting the importance of efficient DNA replication for normal development and neurogenesis. DNA Repair 2013;12:637–44.
Seltzer LE, Paciorkowski AR . Genetic disorders associated with postnatal microcephaly. Am J Med Genet C Semin Med Genet 2014;166C:140–55.
Okamoto N, Ohmachi K, Shimada S, Shimojima K, Yamamoto T . 109 kb deletion of chromosome 4p16.3 in a patient with mild phenotype of Wolf-Hirschhorn syndrome. Am J Med Genet A 2013;161A:1465–9.
Paronett EM, Meechan DW, Karpinski BA, LaMantia AS, Maynard TMv . Ranbp1, deleted in DiGeorge/22q11.2 deletion syndrome, is a microcephaly gene that selectively disrupts layer 2/3 cortical projection neuron generation. Cereb Cortex 2015;25:3977–93.
Guilherme RS, Meloni VA, Perez AB et al, Duplication 9p and their implication to phenotype. BMC Med Genet 2014;15:142.
Abdallah-Bouhjar IB, Mougou-Zerelli S, Hannachi H et al, Molecular cytogenetic and phenotypic characterization of ring chromosome 13 in three unrelated patients. J Pediatr Genet 2013;2:147–55.
Walczak-Sztulpa J, Wisniewska M, Latos-Bielenska A et al, Chromosome deletions in 13q33-34: report of four patients and review of the literature. Am J Med Genet A 2008;146A:337–342.
Tan WH, Bird LM, Thibert RL, Williams CA . If not Angelman, what is it? A review of Angelman-like syndromes. Am J Med Genet A 2014;164A:975–92.
Bishop B, Ho KK, Tyler K et al, The chromatin remodeler chd5 is necessary for proper head development during embryogenesis of Danio rerio. Biochim Biophys Acta 2015;1849:1040–50.
Kim BJ, Zaveri HP, Shchelochkov OA et al, An allelic series of mice reveals a role for RERE in the development of multiple organs affected in chromosome 1p36 deletions. PLoS ONE 2013;8:e57460.
Abu-Amero KK, Hellani AM, Salih MA et al, A de novo marker chromosome derived from 9p in a patient with 9p partial duplication syndrome and autism features: genotype-phenotype correlation. BMC Med Genet 2010;11:135.
Gadea G, Blangy A . Dock-family exchange factors in cell migration and disease. Eur J Cell Biol 2014;93:466–77.
Resta N, Giorda R, Bagnulo R et al, Breakpoint determination of 15 large deletions in Peutz-Jeghers subjects. Hum Genet 2010;128:373–82.
Peddibhotla S, Khalifa M, Probst FJ et al, Expanding the genotype-phenotype correlation in subtelomeric 19p13.3 microdeletions using high resolution clinical chromosomal microarray analysis. Am J Med Genet A 2013;161A:2953–63.
Brandigi E, Molinaro F, Bulotta AL, Angotti R, Pavone M, Messina M . Chromosome 18q-syndrome and 1p terminal duplication in a patient with bilateral vesico-ureteral reflux: case report and literature revision. Ital J Pediatr 2013;39:6.
Giannikou K, Fryssira H, Oikonomakis V et al, Further delineation of novel 1p36 rearrangements by array-CGH analysis: narrowing the breakpoints and clarifying the "extended" phenotype. Gene 2012;506:360–8.
Ben-Shachar S, Ou Z, Shaw CA. et al, 22q11.2 distal deletion: a recurrent genomic disorder distinct from DiGeorge syndrome and velocardiofacial syndrome. Am J Hum Genet 2008;82:214–21.
Mikhail FM, Burnside RD, Rush B et al, The recurrent distal 22q11.2 microdeletions are often de novo and do not represent a single clinical entity: a proposed categorization system. Genet Med 2014;16:92–100.
Kobayashi H, Etoh K, Ohbayashi N, Fukuda M . Rab35 promotes the recruitment of Rab8, Rab13 and Rab36 to recycling endosomes through MICAL-L1 during neurite outgrowth. Biol Open 2014;3:803–814.
Wozniak K, Piaskowski S, Gresner SM et al, BCR expression is decreased in meningiomas showing loss of heterozygosity of 22q within a new minimal deletion region. Cancer Genet Cytogenet 2008;183:14–20.
Hoppe A, Heinemeyer J, Klopocki E et al, Interstitial 12p deletion involving more than 40 genes in a patient with postnatal microcephaly, psychomotor delay, optic nerve atrophy, and facial dysmorphism. Meta Gene 2014;2:72–82.
Sollis E, Graham SA, Vino A et al, Identification and functional characterization of de novo FOXP1 variants provides novel insights into the etiology of neurodevelopmental disorder. Hum Mol Genet 2016;25:546–57.
Lo Vasco VR . Role of phosphoinositide-specific phospholipase C η2 in isolated and syndromic mental retardation. Eur Neurol 2011;65:264–9.
Jordan VK, Zaveri HP, Scott DA . 1p36 deletion syndrome: an update. Appl Clin Genet 2015;8:189–200.
Speed D, Hoggart C, Petrovski S et al, A genome-wide association study and biological pathway analysis of epilepsy prognosis in a prospective cohort of newly treated epilepsy. Hum Mol Genet 2014;23:247–58.
Hu P, Wang Y, Meng LL et al, 1q25.2-q31.3 Deletion in a female with mental retardation, clinodactyly, minor facial anomalies but no growth retardation. Mol Cytogenet 2013;6:30.
Pennucci R, Talpo F, Astro V et al, Loss of either Rac1 or Rac3GTPase differentially affects the behavior of mutant mice and the development of functional GABAergic networks. Cereb Cortex 2016;26:873–90.
van der Heide LP, Wijchers PJ, von Oerthel L et al, FoxK2 is required for cellular proliferation and survival. J Cell Physiol 2015;230:1013–23.
Hamada N, Ito H, Iwamoto I et al, Role of the cytoplasmic isoform of RBFOX1/A2BP1 in establishing the architecture of the developing cerebral cortex. Mol Autism 2015;6:56.
Steinecke A, Gampe C, Zimmer G, Rudolph J, Bolz J . EphA/ephrinA reverse signaling promotes the migration of cortical interneurons from the medial ganglionic eminence. Development 2014;141:460–71.
Butler MG, Dagenais SL, Garcia-Perez JL et al, Microcephaly, intellectual impairment, bilateral vesicoureteral reflux, distichiasis, and glomuvenous malformations associated with a 16q24.3 contiguous gene deletion and a Glomulin mutation. Am J Med Genet A 2012;158A:839–49.
Fasching L, Kapopoulou A, Sachdeva R et al, TRIM28 represses transcription of endogenous retroviruses in neural progenitor cells. Cell Rep 2015;10:20–8.
Lee JA, Liu L, Javier R, Kreitzer AC, Delaloy C, Gao FB . ESCRT-III subunits Snf7-1 and Snf7-2 differentially regulate transmembrane cargos in hESC-derived human neurons. Mol Brain 2011;4:37.
Acknowledgements
We thank the families of the patients for their contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tsoutsou, E., Tzetis, M., Giannikou, K. et al. Application of high-resolution array comparative genomic hybridization in children with unknown syndromic microcephaly. Pediatr Res 82, 253–260 (2017). https://doi.org/10.1038/pr.2017.65
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2017.65