Abstract
Background
Congenital anomalies of the kidney and urinary tract (CAKUT) are the most prevalent etiologies of pediatric chronic kidney disease (CKD). However, no robust mass screening methods have been developed to detect patients with CAKUT, making early intervention to prevent progressive renal failure challenging.
Methods
We applied tandem mass spectrometry (MS/MS) to measure the creatinine (Cr) value from dried blood spot (DBS) analysis, which has been used for newborn mass screening. Subsequently, we evaluated the correlation between DBS Cr measured by MS/MS and serum Cr measured by the conventional method in pediatric patients with CKD. Finally, DBS Cr was measured in 190 full-term, healthy newborns on days 4–6 after birth.
Results
We established a system of MS/MS-based measurement of Cr from DBS. Measured DBS Cr in the pediatric patients showed a strong association with serum Cr (r=0.86; P<0.01). The median DBS Cr value in newborns was 0.222 (interquartile range: 0.189, 0.269) mg/dl. No significant correlations were found between DBS Cr values and body weight, Apgar score, gestational age, and sex in newborns.
Conclusion
We successfully established a method for MS/MS-based measurement of Cr for newborn screening and determined normal reference values for full-term newborns.
Similar content being viewed by others
Main
Congenital anomalies of the kidney and urinary tract (CAKUT) are the most prevalent etiologies of pediatric chronic kidney disease (CKD) (1). The prognosis of CKD is poor in children. A prospective cohort study of Japanese children with CKD stages 3–5 demonstrated that disease progression to a higher CKD stage or end-stage kidney disease (ESKD) occurred in a sizeable number of children, particularly in those with advanced (stages 4/5) CKD (1). The mortality rate in pediatric ESKD is also quite high (2, 3) because of fatal complications. In the United States, 705 of 3,450 children younger than 5 years (98.8/1,000 person-years) who started dialysis between 1990 and 2010 died during dialysis treatment (4).
It has been reported that early intervention for CAKUT can prevent disease progression (5, 6, 7, 8, 9, 10, 11, 12, 13). Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers help delay or prevent progression to ESKD in children (5, 6, 7, 8, 9, 10, 11, 12, 13). These drugs have not only antihypertensive action but also antiproteinuric, antifibrotic, and anti-inflammatory actions. According to the Effect of Strict Blood Pressure Control and ACE Inhibition on Progression of Chronic Renal Failure in Pediatric Patients (ESCAPE) trial, strict blood pressure control (in which mean arterial pressure levels are kept below the 50th percentile) in CKD children who receive a fixed high dose of an ACE inhibitor prevents the progression of CKD to ESKD (8). Therefore, early identification of patients with CAKUT is crucial to protect the remaining renal function and prevent complications in other organs due to CKD.
In Japan, urine screening using dipsticks in 3-year-old children has been carried out for identification of CAKUT, but it has not been very useful (14). Sekhar et al. (15) reported that urine dipstick screening is a poor test for CKD and is not cost-effective. Ishikura et al. (1) reported that only 10% of CKD cases were found by urine screening in 3-year-old children. This is partly because the urine of CAKUT patients is dilute because of reduced urine-concentrating ability; thus, underestimation of proteinuria in these patients is inevitable. A more reliable and ideal approach for finding CAKUT is an ultrasound study. However, ultrasound screening is too expensive to be applied as mass screening. The alternative method for identification of CAKUT is screening of renal function. Patients with severe CAKUT show low renal function; therefore, such patients can be identified by renal function screening. Renal function is estimated through the glomerular filtration rate, which is commonly estimated using creatinine (Cr). Serum Cr reference values (16) and Cr-based estimated glomerular filtration rates (17) have been established in Japanese children aged between 3 months and 16 years, and over 1 year of age, respectively. However, data on Cr values in newborns are limited, and some studies have reported that Cr values change in newborns (18, 19, 20). Therefore, there is an urgent need to determine reference values of Cr as early as days 4–6 after birth for the purpose of newborn mass screening for CAKUT.
In Japan, newborn mass screening using tandem mass spectrometry (MS/MS) and dried blood spot (DBS) analysis for 19 inherited metabolic disorders has been in effect since 2013. Therefore, renal function-based mass screening for CAKUT using the same DBS analysis is reasonable and applicable for all Japanese children. In the present study, we sought to establish a new method for mass screening of renal function using DBS analysis and MS/MS.
Methods
Samples
For the initial study, we recruited 100 pediatric patients who were admitted to the Department of Nephrology of Aichi Children’s Health and Medical Center. Their age, sex, and underlying diseases were not considered. Eight patients with serum Cr >1.2 mg/dl were excluded. Of the patients, 53 were male and 39 were female. Their median age was 7.9 years (IQR: 4.53, 12.40), and median Cr was 0.39 (IQR: 0.31, 0.51) mg/dl. Overall, 39 of them were diagnosed with nephrotic syndrome, 21 with urologic disease, 16 with nephropathy, 11 with hypoplastic/dysplastic kidney and so on. An additional 0.1 ml of blood was collected for DBS analysis simultaneously with blood drawn for serum Cr measurement.
We then collected samples from 190 newborns (males, 99; females, 91) from four hospitals. One hospital is a perinatal medical center and the other three hospitals are private clinics. The blood samples were collected on days 4–6 of life from full-term, well newborns, with the informed consent of their parents. To include normal infants, the following exclusion criteria were applied. First, infants whose mothers were on medications were excluded. Second, babies receiving specific medical support were excluded. Any infants with proven or suspected CAKUT, infections, hypovolemia, or muscle disease, or whom the attending physician judged unsuitable for this study were excluded. At the time of blood sampling for tandem mass screening, two additional spots were collected on filter paper. Gestational age, birth weight, Apgar score (5 min), and age in weeks at the time of blood sampling were noted on the registration form.
This study was approved by the ethics committees of the Nagoya City University Graduate School of Medical Sciences (receipt number: 859-2) and Aichi Children’s Health and Medical Center (receipt number: 201317).
Experimental Methods
Chemicals
Creatinine of standard reference range was purchased from the National Institute of Advanced Industrial Science and Technology (Tsukuba, Japan), and stable isotope-labeled Cr (d3-creatinine) was obtained from Cambridge Isotope Laboratories (Tewksbury, MA, USA). Acetonitrile, methanol, and formic acid were purchased from Wako Pure Chemical Industries (Osaka, Japan). The DBS papers were purchased from ADVANTEC (Tokyo, Japan).
To ensure accurate measurement from DBS analysis, we used the internal standard method. A known amount of internal standard (d3-Cr), which is used in Japanese newborn mass screening, was added to every sample, which enabled accurate calibration by plotting the ratio of the analyte signal to the internal standard signal (21).
Sample Preparation and Mass Spectrometry
On the filter paper, a 1/8-inch circle was punched out from each blood spot (~3 μl) into the individual wells of a 96-well microplate, immersed in 10 μl of fixing solution (methanol-to-acetone-to-water ratio, 7:7:2), and dried at 37 °C for 30 min. Then, 100 μl of extract solution with a known concentration of a stable isotope-labeled standard (0.01 mg/dl d3-Cr) was added to every sample, and the samples were shaken at room temperature for 30 min. Thereafter, the samples (10 μl) were introduced to the LCMS-8040 mass spectrometer (Shimadzu, Kyoto, Japan), which is commonly used for newborn tandem mass screening in Japan. The mobile phase was prepared from a mixture of acetonitrile, methanol, and water at a ratio of 2:2:1, and 0.05% formic acid was added. MS/MS analyses were performed in multiple reaction monitoring mode. The LabSolutions program (Shimadzu) allowed data processing. This software integrated the area under the chromatogram. The LCMS-8040 spectrometer (Shimadzu) was used for MS/MS analysis. Nitrogen served as the auxiliary, curtain, and collision gas. Cr was analyzed in positive ion multiple reaction monitoring mode.
Statistical Methods
All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R commander, which is designed to add statistical functions frequently used in biostatistics (22). The Shapiro–Wilk test was used to determine whether the distribution of DBS Cr was normal. Pearson’s linear correlation coefficient test was used to investigate the association between serum Cr and DBS Cr. Bland–Altman plots were performed to measure agreement with the DBS method estimate. One-way ANOVA was used to investigate significant differences in body weight, Apgar score, gestational age, and sex. In all analyses, P<0.05 was taken to indicate significance.
Results
We successfully established the conditions of MS/MS to measure Cr as follows. The multiple reaction monitoring transitions monitored were m/z 114.10>44.10 for Cr and m/z 117.05>47.10 for d3-Cr (internal standard). The cone voltage and collision energy were 18 V and 18 eV. The retention time of Cr and d3-Cr was ~0.91 min within the 2.0 min chromatography run time (Figure 1). The calibration curve showed good linearity, which ranged from 0.039 to 5.0 mg/dl with an accuracy of 81.6–104.9% and coefficient of variation of 0.1–5.8%.
Chromatograms of creatinine and d3-creatinine with a patient sample. The multiple reaction monitoring (MRM) transitions monitored were m/z 114.10>44.10 for creatinine and m/z 117.05>47.10 for d3-creatinine, respectively. The cone voltage and collision energy were 18 V and 18 eV. The retention time of creatinine and d3-creatinine was ~0.91 min within the 2.0-min chromatography run time. These parameters were tabulated below the graph.
After developing the MS/MS method, we performed the initial study for infancy through childhood. A high correlation (R=0.863) of the serum Cr level with the DBS Cr level (0.5693 times lower than the serum Cr level) was observed in the full range (Figure 2a). Pottel et al. reported a mean value of 0.55 mg/dl (range 0.41–0.75 mg/dl) at day 4 and 0.48 mg/dl (range 0.36–0.69 mg/dl) at day 6 (ref. 23). Stage 3 CKD is 25–50% of renal function, and thus re-calculations were performed in the range of serum Cr up to 0.8 mg/dl. The correlation score was 0.723, and the regression formula was 0.5653 times lower than the serum Cr level in the range of 0.12 (the lowest) to 0.8 mg/dl (Figure 2b). The Bland–Altman analysis to measure the validity of each coefficient shown in Figure 2c showed close to zero bias, and 95% limits of disagreement of −0.087 to +0.095 mg/dl in the full range and of −0.081 to +0.091 mg/dl in the range of serum Cr up to 0.8 mg/dl.
Correlation between serum Cr and DBS Cr and Bland–Altman plots to measure validity. Correlation between serum Cr and DBS Cr for the range of serum Cr <1.2 mg/dl (a) and for serum Cr less than 0.8 mg/dl (b). Bland–Altman plots for 0.565 × serum Cr vs. DBS Cr (serum Cr <1.2 mg/dl) (c) and for 0.570 × serum Cr vs. DBS Cr (serum Cr <0.8 mg/dl) (d). The solid line denotes bias (mean of difference), the small dashed line denotes 95% coefficient interval, and the large dashed line denotes 95% limits of agreement.
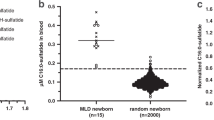
We then applied the DBS MS/MS method on 190 newborns. The mean body weight was 3,168 (interquartile range (IQR): 2,906, 3,455) g in male newborns and 3,068 (IQR: 2,844, 3,262) g in female newborns. Other characteristics of the newborns in the present study are shown in Table 1. The distribution of the DBS Cr levels in relation to each profile is shown in Figure 3. The median DBS Cr value in all newborns was 0.222 (IQR: 0.189, 0.269) mg/dl. The median DBS Cr value was 0.215 (IQR: 0.186, 0.256) mg/dl in the male newborns and 0.229 (IQR: 0.195, 0.278) mg/dl in the female newborns, with no significant difference between the two. The histograms did not follow a normal distribution. One-way analysis of variance (ANOVA) demonstrated no significant difference in DBS Cr values on days 4–6 after birth by body weight, Apgar score, or gestational age, respectively, and Student’s t-test showed no significant difference by sex.
DBS Cr levels in 190 newborns and their distribution in relation to each profile. (a) Histogram of gender-separated DBS Cr. (b) Student’s t-test showed no significant difference in the DBS Cr values on days 4–6 after birth by sex. One-way analysis of variance (ANOVA) demonstrated no significant difference by Apgar score (c), body weight (d), or gestational age (e).
Discussion
To the best of our knowledge, this is the first study of DBS Cr measurement in newborns using a mass screening method. MS/MS has been applied in newborn screening programs around the world to detect inherited metabolic disorders (24). The method used in the present study was MS/MS without columns, which is used in Japanese newborn mass screening. As our method has been widely used for newborn mass screening of metabolic diseases in Japan, successful establishment of DBS Cr measurement by the same system would demonstrate the potential use of DBS Cr-based newborn screening for patients with CAKUT.
The results of our initial study, observed along an age scale from infancy through childhood, showed an approximately two-fold difference between serum Cr and DBS Cr levels. The reason is that whole blood includes hemocytes and is rich in hemoglobin and low in serum components. Thus, the DBS Cr level is always lower than the serum Cr level in the same blood sample (25). The DBS Cr level measured by the method we developed was lower than that in previous studies (25, 26). Our method is exactly the same as that for newborn mass screening in Japan. It is well known that the results of mass spectrometry depend on the methods and instruments. Therefore, the results of different methods would vary significantly between each other. In fact, previous reports have shown substantially different results. As a major application of DBS Cr is in newborn mass screening, a strong correlation of the given measurement with the serum Cr value is crucial. The present results clearly demonstrated a strong association between serum Cr and DBS Cr using Pearson’s linear correlation coefficient test in the range of serum Cr up to 1.2 mg/dl, which is 2–3 times the normal serum Cr at days 4–6 (ref. 23), implying the validity of the measurement.
DBS Cr screening for newborns using MS/MS demonstrated a median DBS Cr of 0.231 (IQR: 0.189, 0.269) mg/dl, which is approximately half of the standard serum Cr level (0.49 mg/dl) for the same age (in days) reported previously (23). This is consistent with the equation in our initial experiment for children—i.e., DBS Cr being 0.5693 times lower than serum Cr. In our newborn study, sex, Apgar score, gestation day, and body weight were not correlated with DBS Cr on days 4–6 after birth.
The estimation of newborn renal function is not easy because it changes rapidly during the first week of life. Renal plasma flow in newborns varies dynamically after birth. At birth, the neonate’s serum Cr reflects the maternal serum Cr, and the neonate’s serum Cr decreases for some time after birth. This movement is controlled by kidney maturation and increasing muscle volume. The Cr level at day 6 in newborns is lower than that at day 4 (ref. 23), but the difference between the predicted serum Cr on day 4 and that on day 6 is 0.07 mg/dl (day 4: 0.55 mg/dl; day 6: 0.48 mg/dl). Therefore, we should use a day-dependent cutoff value. Few samples at days 5 and 6 were available in this study, and therefore we intend to perform a further large study to determine a day-dependent cutoff value. For practical purposes, the small difference can be ignored after day 4 for neonatal screening. Pottel et al. showed that the serum Cr reached a plateau level after ~3 weeks to 1 month after birth, and thus it is ideal to measure renal function at 1 month of age. However, newborn mass screening at 1 month is not practical, at least in Japan, because of the cost and the current health care system. Therefore, the development of newborn screening using DBS screening around day 4 is crucial. The present results show that DBS Cr can be used to identify severe renal dysfunction at around day 4. At least it can be used to identify high-risk neonates who would be invited for more precise screening at 1 month of age.
DBS Cr may vary depending on the hematocrit level. Jeffery reported that neonates born at 35–42 weeks of gestation had mean hematocrit values of about 49% (5% value 34%, 95% value 62%) (27). This means that a serum proportion of about 51% (5% value 38%, 95% value 66%) would create a margin of error of about 30%. Mass screening for congenital hypothyroidism (CH) has the same problem. Whole-blood thyroid-stimulating hormone depends on the neonate’s hematocrit level, but it could be applied for newborn screening for CH (28). Indeed, serum volume varies for the samples, but the cutoff is expected to be high enough to overcome the variability of the serum volume. Therefore, DBS Cr could also be applied for newborn screening if an acceptable cutoff level were set, which will be tested in future studies.
Japanese Society for Mass Screening recommends a cutoff value of +3 to 6 SD for the positive rate (29). Referring to the work of Pottel et al. (23), we looked up a serum Cr value of 0.69 mg/dl at day 6 and 0.75 mg/dl at day 4 for the 97.5th percentile. For DBS Cr, this would correspond to threshold values of 0.39–0.42 mg/dl. In our study, the highest DBS Cr in the present study was 0.42 mg/dl. The cutoff DBS Cr value of 0.39–0.42 would be reasonable for the initial study.
No CAKUT patients were found among the 190 full-term, well newborns in the present study. We followed up on the infant with the highest DBS Cr (0.42 mg/dl) and performed a detailed examination when she was 1 month old. Her serum Cr was 0.29 mg/dl, which was within the normal range for her age, and her DBS Cr was 0.15 mg/dl. Ultrasound study revealed normal kidney sizes of 46.3 mm (right) and 49.6 mm (left) without hydronephrosis. The high DBS Cr of the baby might have reflected the maternal value at birth. In full-term newborns, maternal and neonate serum Cr levels are similar in the first week of life (30). Bariciak et al. (31) reported a strong correlation between maternal and newborn Cr up to 72 h after birth. DBS Cr at day 4 (96 h) would be influenced by the maternal renal function. Our study did not measure maternal Cr at birth, and it is not always possible to obtain maternal data in newborn screening because most clinics do not perform maternal blood examination at birth. Another factor we should discuss is an ethnic effect. It is known that the maternal serum Cr levels of Japanese females are lower than those of White females (32). It suggests that the Japanese infant cutoff value would be lower than the cutoff value used in Pottel’s study. Therefore, further study with a substantial number of Japanese infants should be performed to determine the appropriate cutoff value for the Japanese infant population. An antenatal ultrasound scan is a good test to identify a newborn at risk for CKD, but the test cannot identify all CAKUT patients. Tabel reported that 57.9% (44/76) of CAKUT patients negative on antenatal renal ultrasonography were diagnosed by postnatal ultrasonography screening (33). Although postnatal renal ultrasonography is very important, it should only be carried out for selected neonates because of its considerable cost. We believe that our screening would help identify the neonates not detected by antenatal ultrasound scans.
In Japan, newborn screening is performed in over 100 million babies per year; therefore, it is important that it be affordable and cost-effective. The method we developed is inexpensive. The internal standard (d3-Cr) screens 8,000 babies/dollar. The MS/MS equipment we used is common in MS/MS screening. Most inspection institutes where mass screening is carried out possess the equipment and could perform DBS Cr-based screening without further investment.
Conclusion
We have developed a new method for MS/MS-based measurement of DBS Cr, and we demonstrated that it is practical and cost-effective and can be used as a screening method to detect CAKUT in the neonatal period. This method can be a realistic screening method with respect to the fact that nationwide screening is possible owing to the tandem mass screening method that is already in use. Further studies involving more neonates including CAKUT patients should be carried out.
References
Ishikura K, Uemura O, Hamasaki Y et al, Progression to end-stage kidney disease in Japanese children with chronic kidney disease: results of a nationwide prospective cohort study. Nephrol Dial Transplant 2014;29:878–84.
Oh J, Wunsch R, Turzer M et al, Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 2002;106:100–5.
Chadha V, Warady BA . Epidemiology of pediatric chronic kidney disease. Adv Chronic Kidney Dis 2005;12:343–52.
Mitsnefes MM, Laskin BL, Dahhou M, Zhang X, Foster BJ . Mortality risk among children initially treated with dialysis for end-stage kidney disease, 1990-2010. JAMA 2013;309:1921–9.
Hadtstein C, Schaefer F . Hypertension in children with chronic kidney disease: pathophysiology and management. Pediatr Nephrol 2008;23:363–71.
Wühl E, Schaefer F . Therapeutic strategies to slow chronic kidney disease progression. Pediatr Nephrol 2008;23:705–16.
Ellis D, Vats A, Moritz ML, Reitz S, Grosso MJ, Janosky JE . Long-term antiproteinuric and renoprotective efficacy and safety of losartan in children with proteinuria. J Pediatr 2003;143:89–97.
Wühl E, Trivelli A, Picca S et al, Strict blood-pressure control and progression of renal failure in children. N Engl J Med 2009;361:1639–50.
Ellis D, Moritz ML, Vats A, Janosky JE . Antihypertensive and renoprotective efficacy and safety of losartan. A long-term study in children with renal disorders. Am J Hypertens 2004;17:928–35.
Soergel M, Verho M, Wühl E, Gellermann J, Teichert L, Schärer K . Effect of ramipril on ambulatory blood pressure and albuminuria in renal hypertension. Pediatr Nephrol 2000;15:113–8.
White CT, Macpherson CF, Hurley RM, Matsell DG . Antiproteinuric effects of enalapril and losartan: a pilot study. Pediatr Nephrol 2003;18:1038–43.
Simonetti GD, von Vigier RO, Konrad M, Rizzi M, Fossali E, Bianchetti MG . Candesartan cilexetil in children with hypertension or proteinuria: preliminary data. Pediatr Nephrol 2006;21:1480–2.
von Vigier RO, Zberg PM, Teuffel O, Bianchetti MG . Preliminary experience with the angiotensin II receptor antagonist irbesartan in chronic kidney disease. Eur J Pediatr 2000;159:590–3.
Yanagihara T, Hamada R, Ishikura K et al, Urinary screening and urinary abnormalities in 3-year-old children in Japan. Pediatr Int 2015;57:354–8.
Sekhar DL, Wang L, Hollenbeak CS, Widome MD, Paul IM . A cost-effectiveness analysis of screening urine dipsticks in well-child care. Pediatrics 2010;125:660–3.
Uemura O, Honda M, Matsuyama T et al, Age, gender, and body length effects on reference serum creatinine levels determined by an enzymatic method in Japanese children: a multicenter study. Clin Exp Nephrol 2011;15:694–9.
Uemura O, Nagai T, Ishikura K et al, Creatinine-based equation to estimate the glomerular filtration rate in Japanese children and adolescents with chronic kidney disease. Clin Exp Nephrol 2014;18:626–33.
Boer DP, de Rijke YB, Hop WC, Cransberg K, Dorresteijn EM . Reference values for serum creatinine in children younger than 1 year of age. Pediatr Nephrol 2010;25:2107–13.
Bueva A, Guignard JP . Renal function in preterm neonates. Pediatr Res 1994;36:572–7.
van den Anker JN, de Groot R, Broerse HM et al, Assessment of glomerular filtration rate in preterm infants by serum creatinine: comparison with inulin clearance. Pediatrics 1995;96:1156–8.
Linda L, Ng PD . Validation of Chromatographic Methods. US Food and Drug Administration: Silver Spring, MD, 2014.
Kanda Y . Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 2013;48:452–8.
Pottel H, Vrydags N, Mahieu B, Vandewynckele E, Croes K, Martens F . Establishing age/sex related serum creatinine reference intervals from hospital laboratory data based on different statistical methods. Clin Chim Acta 2008;396:49–55.
Rashed MS . Clinical applications of tandem mass spectrometry: ten years of diagnosis and screening for inherited metabolic diseases. J Chromatogr B Biomed Sci Appl 2001;758:27–48.
den Burger JC, Wilhelm AJ, Chahbouni AC, Vos RM, Sinjewel A, Swart EL . Haematocrit corrected analysis of creatinine in dried blood spots through potassium measurement. Anal Bioanal Chem 2015;407:621–7.
Koop DR, Bleyle LA, Munar M, Cherala G, Al-Uzri A . Analysis of tacrolimus and creatinine from a single dried blood spot using liquid chromatography tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 2013;926:54–61.
Jopling J, Henry E, Wiedmeier SE, Christensen RD . Reference ranges for hematocrit and blood hemoglobin concentration during the neonatal period: data from a multihospital health care system. Pediatrics 2009;123:e333–7.
Nagasaki K, Minamitani K, Anzo M et al, Guidelines for mass screening of congenital hypothyroidism (2014 revision). Clin Pediatr Endocrinol 2015;24:107–33.
Gary LH, Blas C, Donald HC, Sara C . Newborn Screening by Tandem Mass Spectrometry; Approved Guideline. Clinical and Laboratory Standards Institute: Wayne, PA, 2010.
Schwartz GJ, Feld LG, Langford DJ . A simple estimate of glomerular filtration rate in full-term infants during the first year of life. J Pediatr 1984;104:849–54.
Bariciak E, Yasin A, Harrold J, Walker M, Lepage N, Filler G . Preliminary reference intervals for cystatin C and beta-trace protein in preterm and term neonates. Clin Biochem 2011;44:1156–59.
Lim E, Miyamura J, Chen JJ . Racial/ethnic-specific reference intervals for common laboratory tests: a comparison among Asians, Blacks, Hispanics, and White. Hawaii J Med Public Health 2015;74:302–10.
Tabel Y, Haskologlu ZS, Karakas HM, Yakinci C . Ultrasonographic screening of newborns for congenital anomalies of the kidney and the urinary tracts. Urol J 2010;7:161–7.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
STATEMENT OF FINANCIAL SUPPORT
This research was partially supported by Grants-in-Aid for research on efficient screening and health check-ups of infants based on epidemiology from the Japan Agency for Medical Research and Development (AMED). This study was supported by the Japan Agency for Medical Research and Development.
Rights and permissions
About this article
Cite this article
Nakano, M., Uemura, O., Honda, M. et al. Development of tandem mass spectrometry-based creatinine measurement using dried blood spot for newborn mass screening. Pediatr Res 82, 237–243 (2017). https://doi.org/10.1038/pr.2017.56
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2017.56
This article is cited by
-
Assessment of creatinine concentration in whole blood spheroids using paper spray ionization–tandem mass spectrometry
Scientific Reports (2022)
-
Creatinine standardization: a key consideration in evaluating whole blood creatinine monitoring systems for CKD screening
Analytical and Bioanalytical Chemistry (2022)
-
Acute Kidney Injury in the Preterm Neonate
Current Treatment Options in Pediatrics (2018)