Abstract
Background
In children with congenital heart disease (CHD), altered pulmonary circulation compromises gas exchange. Moreover, pulmonary dysfunction is a complication of cardiac surgery with cardiopulmonary bypass (CPB). No data are available on the effect of different CHDs on lung injury. The aim of this study was to analyze epithelial lining fluid (ELF) surfactant composition in children with CHD.
Methods
Tracheal aspirates (TAs) from 72 CHD children (age 2.9 (0.4–5.7) months) were obtained before and after CPB. We measured ELF phospholipids, surfactant proteins A and B (SP-A, SP-B), albumin, and myeloperoxidase activity. TAs from 12 infants (age 1.0 (0.9–2.9) months) with normal heart/lung served as controls.
Results
Heart defects were transposition of great arteries (19), tetralogy of Fallot (TOF, 20), atrial/ventricular septal defect (ASD/VSD, 22), and hypoplastic left heart syndrome (11). Increased levels of ELF SP-B were found in all defects, increased myeloperoxidase activity in all except the TOF, and increased levels of ELF albumin and SP-A only in ASD/VSD patients. Postoperatively, ELF findings remained unchanged except for a further increase in myeloperoxidase activity.
Conclusion
ELF composition has distinctive patterns in different CHD. We speculate that a better knowledge of the ELF biochemical changes may help to prevent respiratory complications.
Similar content being viewed by others
Main
Congenital heart diseases (CHDs), affecting 7–10 per 1,000 births, are the leading cause of infant mortality due to birth defects (1).
The cardiovascular and respiratory systems are closely interdependent, since congenital cardiovascular malformations change the pattern of pulmonary blood flow. Depending upon the type of cardiac defect, lungs may be overperfused, like in the atrio/ventricular septal defect (ASD/VSD) and in the obstruction of the left ventricular outflow tract, or underperfused like in the obstruction of the right ventricular outflow tract (2, 3). In infants with transposition of great arteries (TGAs), pulmonary blood flow progressively increases after birth with the reduction of pulmonary vascular resistance. Other causes of respiratory failure associated with CHD may arise through several other mechanisms, such as direct compression of the airways by dilated and pulsatile main arteries or atria walls, changes in lung water distribution, or increased risk of infection (4).
Surgical repair of CHD with or without cardiopulmonary bypass (CPB) can also lead to a lung insult, extending from microscopic atelectasis to fulminant acute respiratory distress syndrome (5, 6), by the activation of a systemic inflammatory response (7). In addition, during CPB, the lungs are collapsed and pulmonary blood derives only from the bronchial arteries. In the post CPB phase, the mismatch between pulmonary oxygen demand and supply can result in oxidative stress leading to the generation of free oxygen radicals, which play an important role in the increase of vascular permeability and interstitial lung fluid overload (8, 9).
Pulmonary surfactant, a mixture of lipids and proteins (SPs), regulates surface tension at the alveolar interface (10). SP-A is the most abundant SP with an important role in lipid turnover and lung defense (11). SP-B enhances the spreading and stability of the surfactant film and is the only protein absolutely required for proper lung function (12).
Previous animal studies have found changes of the surfactant system after CPB, including an increase in the phospholipid-to-protein ratio in tracheal aspirates (TAs), an increase of the fraction of SP-B associated with subfractions of the surfactant easy to sediment, and high plasma levels of mature SP-B (13, 14).
These studies have tried to establish a correlation between the type of CHD and the composition of the fluid that bathes the airways. Gutierrez et al. (13) found that increased pulmonary blood flow decreases the concentration of SP-A and SP-B in lung lavage fluid obtained from 4-week-old lambs with CHD, whereas no significant differences were found in the same animal model in the first few weeks of life (14). To the best of our knowledge, no data are available on the effect of different types of CHD on the ELF composition in children. Therefore, we designed this study to determine if infants with CHD have a different predisposition to develop acute lung injury postoperatively, based on their cardiac malformation. Second, we aimed to determine the acute changes on surfactant composition and on alveolar capillary leak induced by the CPB in the same group of infants.
Methods
Study Subjects and Design
Between 2014 and 2016, we prospectively studied 72 children with CHD undergoing surgical correction.
Study inclusion criteria were children with CHD, scheduled to elective cardiac surgery, with CPB time >60 min, on a stable hemodynamic condition with no inotropic support and constant intravenous fluid infusion for at least 24 h before the study.
Exclusion criteria were age >48 months, liver or renal failure (factor V<20% and/or creatinine clearance <30%), mechanical ventilation before surgery, perioperative diagnosis of chromosomal abnormalities, and preexisting lung diseases.
Management of anesthesia was uniform in all children. After anesthesia induction with fentanyl and muscle relaxation with vecuronium bromide, the children were intubated and anesthesia was maintained using fentanyl and midazolam.
After administration of heparin (activated clotting time about 480 s), CPB was initiated. A CPB hematic prime was used to maintain a hematocrit between 25 and 30%. During CPB, mild-to-deep hypothermia was applied and lungs were not ventilated. After rewarming, circulation was reestablished and ventilation was started with an inspired oxygen fraction (FiO2) of 1.0. Once the clinical condition was stable, children were transferred to the cardiac intensive care unit (CICU). Clinical complications were recorded until hospital discharge and at the follow-up visit performed 12 months after surgery.
Twelve infants of <6 months of age with no cardiopulmonary disease served as controls. None of them had a history of chronic respiratory symptoms or recent upper or lower respiratory tract infections. They underwent elective surgery for anorectal (n=4), facial (n=1), and gastrointestinal (n=4) malformation, subdural hematoma (n=1), retroperitoneal mass (n=1), and central venous line placement (n=1).
The study was approved by the local ethics committee (Protocol number 3142/AO/14; Padova Hospital, Padova, Italy), and parental informed consent was obtained for all study patients.
Sample Collection
TAs were collected, immediately after anesthesia induction and intubation and, in children with CHD, at the end of the surgery with a standardized procedure. Briefly, the child was placed in a supine position with the head turned on one side to guide the catheter into the lower lobe. A concentration of 0.5 ml/kg of 0.9% saline were instilled down the endotracheal tube via a side port connector and after five ventilator cycles, the suction catheter (Diameter ET <2.5 → 5 Ch, Diameter ET >2.5 → 6–7 Ch) was gently inserted 0.5 cm beyond the tube tip and the airway fluid was suctioned into a sterile Lukens trap (NB-BALTrap; CAIR LGL, Lissieu, France) with 5–10 kPa (37–75 mm Hg) of negative pressure. After eight ventilator cycles, the head was turned to the opposite side and the procedure was repeated, to have a high chance of suctioning the lung on the opposite side. Part of the liquid recovered was used as such and a part was centrifuged at 400g for 10 min to sediment cells and cell debris. Aliquots of whole TAs and supernatants were stored at −80 °C. At the same time point, 100 μl of fresh blood was drawn into Vacutainer tubes containing EDTA. After being centrifuged at 1,400g for 10 min, the plasma was frozen at −80 °C until analysis.
Sample Analysis
Phospholipids (PLs), SP-A, SP-B, and albumin were measured in TA supernatants. Myeloperoxidase activity (MPO) was measured in whole TAs.
Lipids were extracted from TAs with chloroform/methanol (15) and PL concentration was determined according to Bartlett (16).
SP-A concentration was measured using an enzyme-linked immunosorbent assay developed and validated at the Department of Medicine, University of Padova, Italy (17). To perform it, a surfactant was obtained from the lung lavage fluid of a patient with alveolar proteinosis and SP-A was isolated according to Hawgood et al. (18). SP-A was then used to immunize a rabbit. An IgG fraction anti-SP-A was finally isolated from the whole serum using the Econo-Pac Serum IgG Purification Kit (Bio-Rad, Hercules, CA).
The assay was done in the following way. SP-A in 5 mM Tris-HCl, pH 7.4 (0.7 μg/ml per well) was allowed to bind for 90 min at room temperature to Maxisorp microwell plates (Nunc Immuno; Sigma-Aldrich, Saint Louis, MO). After washing three times with 0.1% Triton X-100 in phosphate-buffered saline (PBST), the wells were quenched for 1 h at room temperature with 250 μl of 3% of BSA in PBST (PBSTA). Although wells are coated with SP-A and quenched, in separate vials, 0–125 ng of pure SP-A or 0–10 μl of TA were mixed with 25 μg of rabbit IgG anti-SP-A and incubated for 2 h at 37 °C in a total volume of 400 μl of 3% EDTA in PBSTA. At the end, 100 μl of these mixtures were added in triplicate to the wells and the incubation was allowed to take place for 2 h at room temperature. The wells were washed, goat anti-rabbit IgG conjugated with peroxidase (Sigma-Aldrich; 1:1,000) in PBSTA was added, and the plate was incubated for 60 min at room temperature. After a final wash with PBST, OPD (1.3 mg/ml) in 5 mM of H2O2 citrate buffer, pH 4.65, was added, and after stopping the reaction with 2 M H2SO4, absorbance was measured at 492 nm. The assay can detect 0.5–25 ng of SP-A with an intra- and interassay coefficient of variation of 4.5 and 4.7%.
The enzyme-linked immunosorbent assay for SP-B has been described in detail by Kramer et al. (19). SP-B standard was obtained from human bronchoalveolar lavage fluid originating from patients with alveolar proteinosis by LH60 chromatography in methanol/chloroform/0.1 M HCl (47.5:47.5:5). Antiserum anti-SP-B was raised in a rabbit using SP-B as an antigen isolated by Bond Elute NH2 chromatography from a chloroform extract of a purified human surfactant. The purity of the antigen is documented in Simonato et al. (20).
This assay can detect 0.2–30 ng of SP-B with an intra-assay coefficient of variation of 2.4% and an interassay coefficient of 9.7%.
Albumin concentration was measured with the bromocresol green method (21). MPO was measured as reported previously (22).
TA dilution was calculated by analyzing plasma and TA urea levels using a commercial kit (QuantiChrom Urea Assay Kit; Bioassay System, Hayward, CA). TA samples with urea concentration below 0.08 mg/dl (kit linear detection range 0.08–100 mg/dl) were discarded. The ratio of plasma urea to TA urea was used to calculate the dilution of epithelial lining fluid (ELF) as described previously (23). This dilution factor was applied to all TA biomarker calculations to obtain the ELF concentration.
Lung function was assessed by the PaO2/FiO2 ratio and by the alveolar–arterial oxygen pressure gradient calculated within 1 h from the arrival in the CICU. At the same time, oxygenation index and dynamic compliance were also calculated. The mean vasoactive-inotrope score (VIS) (24) was calculated for each study infant in the first 12 h after the admission to the CICU.
Statistical Analysis
Continuous data were tested for normal distribution with the Lilliefors-corrected Kolmogorov–Smirnov test. Variables were reported as mean values and standard deviations if normally distributed or as median values and interquartile range. χ2 test or Fisher’s exact test were used to compare categorical variables. One-way ANOVA and Kruskal–Wallis ANOVA were used to determine the difference between groups, whereas paired t-test or Wilcoxon’s test were used to evaluate intrasubject variability. To compare CHD groups with controls, we used the Mann–Whitney U-test. Spearman’s correlation was performed to evaluate the correlation between biomarker data and clinical parameters.
All tests were two-sided, and a P value lower than 0.05 was considered statistically significant. Statistical analysis was performed using PASW Statistics 18.0 (IBM Corp, Armonk, NY).
Results
Population Description
Seventy-two children with CHD undergoing elective cardiac surgery were included in this study (Table 1). TGA diagnosis was made in 19 patients, tetralogy of Fallot (TOF) in 20, ASD/VSD in 22, and hypoplastic left heart syndrome (HLHS) in 11. The ASD/VSD group included mostly VSD (18 patients), whereas the remaining four patients were affected by ASD, ASD, and VSD, and common atrioventricular canal (two patients). The baseline demographic and surgical variables of the CHD group are reported in Table 1.
The median age at surgery was 2.9 (0.4–5.7) months in the CHD group and 1.0 (0.9–2.9) months in the control group (difference not significant). Among the control children, all were born at term and 7 out of 12 were male. The mean weight of controls at surgery was 3.7 (3.5–5.4) kg.
There were significant differences among CHDs with regard to age, weight, and preoperative oxygen saturation, as expected by the study design. According to the surgical procedure, there were significant differences in surgery and CPB time, temperature nadir, and hypothermia duration among CHDs (Table 1). Among the 72 patients, six (8%) required extracorporeal membrane oxygenation support in the immediate postoperative period, and five (7%) were admitted to the CICU with open chest. Six children (8%) died in the CICU (two TOF; one ASD/VSD; and three HLHS). No other patient died until hospital discharge. Three patients were lost at the follow-up.
Preoperative Measurements
Among the TA samples collected in the preoperative phase, one hematic sample (TGA group) and three (ASD/VSD group) with low urea concentration (below 0.08 mg/dl) were discarded.
As shown in Table 2, increased levels of ELF SP-B, with respect to controls, were found in all defects, the increase going from 2.7 times in ASD/AVD to 6.2 times in HLHS. We observed increased MPO activity in all heart defects, excluding TOF. Increased levels of ELF albumin and SP-A were observed only in patients with atrial or ventricular septal defects. Globally, atrial and ventricular septal defects showed the greatest difference with respect to controls in ELF composition.
There were no significant differences in ELF MPO, SP-A, and SP-B concentration among groups even if the median value of ELF SP-A in the ASD/VSD group was almost twice that of the TOF patients. Children with TGA had significantly higher ELF PL concentration than those with TOF. ELF albumin concentration was significantly higher in the ASD/VSD group compared with the other CHD groups (Table 2).
Postoperative Clinical Data and Measurements
PaO2/FiO2 ratio, alveolar–arterial oxygen pressure gradient 2, oxygenation index, and dynamic compliance were calculated in 61 out of the 72 patients. Patients with an open chest (n=5) or dependent on mechanical support (extracorporeal membrane oxygenation, n=6) were excluded from the analysis. The duration of mechanical ventilation and the VIS score was calculated for all study patients.
As expected, at CICU admission, HLHS patients had the highest postoperative requirement of inotrope support (VIS score 18 (11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22); P<0.001) and higher oxygenation index and lower PaO2/FiO2 with respect to ASD/VSD patients (P=0.02 in both). The median duration of mechanical ventilation was significantly longer in the HLHS group (P=0.011 vs. TOF group; P<0.001 vs. ASD/VSD group) and in the TGA group (P<0.001 vs. ASD/VSD group) (Table 1).
In the postoperative period, atelectasis developed in 26 (nine TGA; six TOF; eight ASD/VSD; and three HLHS) and pneumothorax in six children (one TGA; two TOF; one ASD/VSD; and two HLHS).
Among the TAs collected at the post CPB phase, one hematic sample (ASD/VSD) and five samples (one TGA, two TOF, and two ASD/VSD) with low urea concentration (below 0.08 mg/dl) were discarded.
Postoperative findings remained largely unchanged, but ELF PL concentration was still significantly higher in TGA than in TOF (Table 2). Intragroup comparison showed an increase in MPO activity, but the change was significant only for children with TOF and ASD/VSD (P=0.04 and P=0.03, respectively).
In patients requiring intubation and ventilation for more than 48 h postoperatively, basal ELF SP-B was higher (P<0.01) than in those extubated within 48 h (Figure 1). This difference persisted even when patients with cardiovascular instability (VIS ≥15) were excluded (P<0.01, data not shown) (25).
Relationship between the epithelial lining fluid level of preoperative surfactant protein B (SP-B) and the duration of mechanical ventilation (MV). Patients were divided into two groups using a cutoff value for mechanical ventilation length of 48 h. Data are presented as traditional Tukey’s box-and-whisker plot. Outliers are presented as circle dots. The P value was calculated using the Mann–Whitney U-test. P<0.05 was considered statistically different. **P<0.01.
Correlations Between TA Composition and Clinical Variables
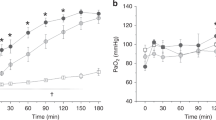
Overall, pre- and post-CPB ELF SP-B concentration correlated inversely with dynamic compliance (Spearman’s ρ=−0.555, P=0.001 and Spearman’s ρ=−0.496, P=0.006, respectively) Figure 2.
Correlation with pre- and postoperative surfactant protein B (SP-B) (μg/ml) and dynamic compliance. Spearman’s ρ =−0.555, P<0.001 (a) and ρ =−0.496, P<0.01 (b). ASD, atrial septal defect; HLHS, hypoplastic left heart syndrome; TGA, transposition of great arteries; TOF, tetralogy of Fallot; VSD, ventricular septal defect.
There was no significant correlation between post-CPB ELF concentrations of PL, SP-A, SP-B, and albumin and the mean of the following parameters recorded during the surgery: minimum temperature; CPB, hypothermia, and rewarming duration; hemodilution (measured as mean hemoglobin value during CPB); mean cerebral regional perfusion saturation; and mean lactates measured during surgery.
MPO increase was inversely correlated with mean cerebral regional perfusion saturation (P=0.005, Spearman’s ρ=−0.409) and with mean lactate levels (P=0.006, Spearman’s ρ=−0.408).
Discussion
This study examined the ELF composition obtained before and after surgery in children with four different classes of CHDs. Data, corrected for dilution, were compared with those obtained from a control population of children of comparable age and normal cardiac and lung function. It appears that TAs have specific composition in the different CHDs and that TA analysis may contribute usefully to the description of lung changes associated with CHD.
In summary, we found an increased SP-B concentration in airway fluids in all cardiac defects, an increased neutrophil activity in all defects except TOF, and an increased concentration of albumin and SP-A only in patients with atrial or ventricular septal defects. Postoperative findings remained largely unchanged, except for a further increase in ELF neutrophil activity.
SP-B increase could have different explanations. It could be the expression of changes in fetal lung development. As an example in fetuses with TGA, the blood enters the pulmonary artery with an oxygen saturation considerably higher than that during normal fetal life (26), and it has been shown that chronic hyperoxia leads to increased expression of SPs (27) and that the hydrophobic SPs (SP-B and SP-C) could facilitate the oxygen transport capability through the air–water interface (28). On the other side, increased levels of SP-B could be related to the pattern of breathing, since all patients were tachypneic, and in rats, it has been found that prolonged tachypnea increases the expression of SP-B (29). Increased levels of SP-B could also be associated with an increased cost of breathing, as suggested by the negative correlation between SP-B levels and dynamic compliance and by the finding that children ventilated for more than 48 h had a higher preoperative SP-B amount than those extubated within 48 h. Please note that this correlation was also confirmed in infants with stable hemodynamic conditions (VIS<15) where the length of mechanical ventilation could be due to respiratory failure. Thus, SP-B could be a marker of lung injury, as previously reported in mice after endotoxin-mediated lung injury (30), or in neonatal pneumonia at the onset of respiratory failure (31).
It is worth noting that in our study, ELF total PL was within normal limits, but the proportion between surfactant subtypes was not addressed and measured SP-B does not distinguish between mature SP-B and other isoforms present in the airways, nor between active or spent surfactant (32). Moreover, mature SP-B, which is synthesized in the distal airways, could not be in equilibrium with that obtained in the upper airways by the tracheal aspiration technique.
ELF SP-A level was significantly increased with respect to controls only in children with ASD/VSD. The causes could be many, like previous respiratory infections, especially frequent in this population (33), the need of increasing surfactant spreading in a protein-rich environment, the direct effect of increased pulmonary blood flow, or the need to increase the clearance of materials accumulating in the airways as a consequence of increased microvascular permeability.
Except for children with TOF, who appeared to be protected, children with TGA, ASD/VSD, and HLHS were all characterized by an increased ELF MPO activity in the airways. This finding is apparently new and deserves further investigation. The reduced pulmonary blood flow in TOF infants may explain the reduced MPO activity found in this group of infants before cardiac surgery.
Compared with controls, children with ASD/VSD had higher ELF levels of albumin, a sign of increased microvascular permeability (29). CHD with large left-to-right shunts is characterized by increased pulmonary blood flow that leads to decreased lung volumes, decreased compliance, and increased production of interstitial fluid (2). These lung changes require several weeks to fully develop, since in the early postnatal period, lungs are protected by the high vascular resistance of the neonatal period that smoothens over time (26, 34). Our ELF finding can explain why these infants are at higher risk to develop severe respiratory infection before cardiac surgery. Unfortunately, we could not correlate the albumin levels in TAs and blood flow through the lungs since this measurement was not available.
CBP has a cost for the lungs, particularly in children due to their immature lungs (35). In our study, TA composition remained largely unchanged, except for an increase in neutrophil recruitment. Only two previous reports described surfactant composition changes in children with CHD after CPB (36, 37). In the first one, Friedrich et al. (36) investigated the composition of a surfactant in 35 children undergoing CPB and in 15 infants who underwent cardiovascular surgery without bypass procedure (called control group). Before surgery, both groups showed no differences with regard to the biochemical composition of the large aggregate fraction of the tracheal aspirate. This is in contrast with our data but the difference might be explained by patients’ characteristics as our control group is composed of infants with no cardiopulmonary disease. Focusing on the CPB group, they find an early increase in total proteins that became significant after 4 h, and a later increase in SP-B and PL, whereas SP-A remained unchanged. These data are thus comparable with our findings concerning the immediate postoperative period; in fact, only MPO significantly increased early after CPB. Unfortunately, since we did not collect samples during the CICU stay, we cannot comment on changes that may occur at a later time. In the other paper, Griese et al. (37) characterized the biochemical composition of the pulmonary surfactant of 19 infants with CPB and of 13 children who required elective intubation for magnetic resonance imaging. After the surgery, PL, TP, SP-A, and SP-B were elevated upon the level of the control infants. These results are consistent with our data, but in that report, the preoperative tracheal aspirate composition is missing; therefore, it is difficult to ascribe the difference to CPB rather than to the CHD.
Increase in MPO during CPB has already been reported (38). Ischemia during CPB results in endothelial activation upon reperfusion (39); during this phase, the mismatch between pulmonary oxygen demand and supply can result in oxidative stress, in which excessive reactive oxygen species accumulate (40). Interestingly, we found that MPO increase is inversely correlated with both mean cerebral regional perfusion saturation (P=0.005, Spearman’s ρ=−0.409) and with mean lactate levels (P=0.006, Spearman’s ρ=−0.408), implying that a marginal cardiac output could sustain an oxidative cascade that could ultimately lead to multiorgan system failure.
There are limitations in this study. First, although the differences in TA composition among groups appear to be consistent, our findings are based on patients collected in a single center. Furthermore, we could not correlate ELF composition with variables such as left-to-right shunt, pressure regimens in the pulmonary circulation, or ventilation patterns. Finally, other markers of inflammation could have been measured.
Conclusion
TA has specific composition in the different CHDs considered in this study. Increased levels of SP-B were found in all defects, suggesting that SP-B concentrations in TAs might be used as a marker of lung derangement. Neutrophil recruitment was also found in all children, except those with TOF. All CHD children seem to have a damage to the alveolar–capillary membrane, but infants with a septal defect seem to be the most severely affected with increased levels of TA albumin and SP-A. In this group of patients, an earlier repair might thus play a protective role.
Postoperative findings remained largely unchanged, except for a further increase in neutrophil lung recruitment.
TA analysis may help to construe a coherent picture of lung changes associated with CHD, clarifying, e.g., the contribution of surfactant changes, lung hyperperfusion, or inflammation to respiratory failure observed in children with CHD. These findings will help to spot specific strategies to counteract the acute lung injury in CHD infants postoperatively.
References
Hoffman JI, Kaplan S . The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890–1900.
Cooper DS, Jacobs JP, Chai PJ et al. Pulmonary complications associated with the treatment of patients with congenital cardiac disease: consensus definitions from the Multi-Societal Database Committee for Pediatric and Congenital Heart Disease. Cardiol Young 2008;18 (Suppl 2): 215–221.
Rao PS . Diagnosis and management of cyanotic congenital heart disease: part I. Indian J Pediatr 2009;76:57–70.
Healy F, Hanna BD, Zinman R . Pulmonary complications of congenital heart disease. Paediatr Respir Rev 2012;13:10–15.
Allen BS, Ilbawi MN . Hypoxia, reoxygenation and the role of systemic leukodepletion in pediatric heart surgery. Perfusion 2001;16 (Suppl): 19–29.
Apostolakis E, Filos KS, Koletsis E et al. Lung dysfunction following cardiopulmonary bypass. J Card Surg 2010;25:47–55.
Pavelkova M, Kubala L, Ciz M et al. Blood phagocyte activation during open heart surgery with cardiopulmonary bypass. Physiol Res 2006;55:165–173.
Brasil LA, Gomes WJ, Salomao R et al. Inflammatory response after myocardial revascularization with or without cardiopulmonary bypass. Ann Thorac Surg 1998;66:56–59.
Babik B, Asztalos T, Petak F et al. Changes in respiratory mechanics during cardiac surgery. Anesth Analg 2003;96:1280–1287 table of contents.
Serrano AG, Perez-Gil J . Protein–lipid interactions and surface activity in the pulmonary surfactant system. Chem Phys Lipids 2006;141:105–118.
Crouch E, Wright JR . Surfactant proteins a and d and pulmonary host defense. Annu Rev Physiol 2001;63:521–554.
Weaver TE, Conkright JJ . Function of surfactant proteins B and C. Annu Rev Physiol 2001;63:555–578.
Gutierrez JA, Parry AJ, McMullan DM et al. Decreased surfactant proteins in lambs with pulmonary hypertension secondary to increased blood flow. Am J Physiol Lung Cell Mol Physiol 2001;281:L1264–L1270.
Lee JW, Ovadia B, Azakie A et al. Increased pulmonary blood flow does not alter surfactant protein gene expression in lambs within the first week of life. Am J Physiol Lung Cell Mol Physiol 2004;286:L1237–L1243.
Bligh EG, Dyer WJ . A rapid method of total lipid extraction and purification. Can J Biochem Physiol 1959;37:911–917.
Bartlett GR . Phosphorus assay in column chromatography. J Biol Chem 1959;234:466–468.
Baritussio A, Alberti A, Quaglino D et al. SP-A, SP-B, and SP-C in surfactant subtypes around birth: reexamination of alveolar life cycle of surfactant. Am J Physiol 1994;266:L436–L447.
Hawgood S, Benson BJ, Schilling J et al. Nucleotide and amino acid sequences of pulmonary surfactant protein SP 18 and evidence for cooperation between SP 18 and SP 28-36 in surfactant lipid adsorption. Proc Natl Acad Sci USA 1987;84:66–70.
Kramer HJ, Schmidt R, Gunther A et al. ELISA technique for quantification of surfactant protein B (SP-B) in bronchoalveolar lavage fluid. Am J Respir Crit Care Med 1995;152:1540–1544.
Simonato M, Baritussio A, Pioselli B et al. Surfactant protein C metabolism in human infants and adult patients by stable isotope tracer and mass spectrometry. Anal Bioanal Chem 2014;406:6225–6233.
Shirole R, Kshatriya AA, Kshatriya AA et al. Mechanistic evaluation of butea monosperma using in vitro and in vivo murine models of bronchial asthma. Int J Res Ayurveda Pharm 2013;4:322–331.
Lamonica G, Amigoni M, Vedovelli L et al. Pulmonary surfactant synthesis after unilateral lung injury in mice. J Appl Physiol (1985) 2014;116:210–215.
Rennard SI, Basset G, Lecossier D et al. Estimation of volume of epithelial lining fluid recovered by lavage using urea as marker of dilution. J Appl Physiol (1985) 1986;60:532–538.
Gaies MG, Jeffries HE, Niebler RA et al. Vasoactive-inotropic score is associated with outcome after infant cardiac surgery: an analysis from the Pediatric Cardiac Critical Care Consortium and Virtual PICU System Registries. Pediatr Crit Care Med 2014;15:529–537.
Mittnacht AJ, Thanjan M, Srivastava S et al. Extubation in the operating room after congenital heart surgery in children. J Thorac Cardiovasc Surg 2008;136:88–93.
Rudolph AM . Congenital cardiovascular malformations and the fetal circulation. Arch Dis Child Fetal Neonatal Ed 2010;95:F132–F136.
ter Horst SA, Fijlstra M, Sengupta S et al. Spatial and temporal expression of surfactant proteins in hyperoxia-induced neonatal rat lung injury. BMC Pulm Med 2006;6:8.
Olmeda B, Villen L, Cruz A et al. Pulmonary surfactant layers accelerate O(2) diffusion through the air–water interface. Biochim Biophys Acta 2010;1798:1281–1284.
Yogalingam G, Doyle IR, Power JH . Expression and distribution of surfactant proteins and lysozyme after prolonged hyperpnea. Am J Physiol 1996;270:L320–L330.
Ikegami M, Falcone A, Whitsett JA . STAT-3 regulates surfactant phospholipid homeostasis in normal lung and during endotoxin-mediated lung injury. J Appl Physiol (1985) 2008;104:1753–1760.
D'Aronco S, Simonato M, Vedovelli L et al. Surfactant protein B and A concentrations are increased in neonatal pneumonia. Pediatr Res 2015;78:401–406.
Rodriguez-Capote K, Manzanares D, Haines T et al. Reactive oxygen species inactivation of surfactant involves structural and functional alterations to surfactant proteins SP-B and SP-C. Biophys J 2006;90:2808–2821.
Jung JW . Respiratory syncytial virus infection in children with congenital heart disease: global data and interim results of Korean RSV-CHD survey. Korean J Pediatr 2011;54:192–196.
Rudolph AM . The changes in the circulation after birth. Their importance in congenital heart disease. Circulation 1970;41:343–359.
Whiting D, Yuki K, DiNardo JA . Cardiopulmonary bypass in the pediatric population. Best Pract Res Clin Anaesthesiol 2015;29:241–256.
Friedrich B, Schmidt R, Reiss I et al. Changes in biochemical and biophysical surfactant properties with cardiopulmonary bypass in children. Crit Care Med 2003;31:284–290.
Griese M, Wilnhammer C, Jansen S et al. Cardiopulmonary bypass reduces pulmonary surfactant activity in infants. J Thorac Cardiovasc Surg 1999;118:237–244.
Quaniers JM, Leruth J, Albert A et al. Comparison of inflammatory responses after off-pump and on-pump coronary surgery using surface modifying additives circuit. Ann Thorac Surg 2006;81:1683–1690.
Verrier ED, Boyle EM Jr . Endothelial cell injury in cardiovascular surgery. Ann Thorac Surg 1996;62:915–922.
Ding J, Zhang Q, Luo Q et al. Alda-1 attenuates lung ischemia–reperfusion injury by reducing 4-hydroxy-2-nonenal in alveolar epithelial cells. Crit Care Med 2016;44:e544–e552.
Acknowledgements
This study was supported by Fondazione Just Italia “Bando Nazionale 2016” and by Cariparo Young Investigator on Pediatric Research 2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Simonato, M., Baritussio, A., Carnielli, V. et al. Influence of the type of congenital heart defects on epithelial lining fluid composition in infants undergoing cardiac surgery with cardiopulmonary bypass. Pediatr Res 83, 791–797 (2018). https://doi.org/10.1038/pr.2017.326
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2017.326
This article is cited by
-
Chorioamnionitis alters lung surfactant lipidome in newborns with respiratory distress syndrome
Pediatric Research (2021)