Abstract
Background
Hypoxic–ischemic encephalopathy (HIE) is a major cause of neonatal morbidity and mortality. Therapeutic hypothermia (TH) is the only available intervention, but neuroprotection is incomplete and variable. Seizures are common in infants with HIE undergoing TH and may worsen outcome. Phenobarbital (PB) is sometimes added, although use of prophylactic PB is controversial in the neonate. We hypothesize that prophylactic PB will not reduce, and may enhance, the neuroprotective effects of TH on brain injury and motor outcomes in the postnatal day 10 (P10) hypoxic–ischemic (HI) rat.
Methods
P10 rat pups were subjected to unilateral HI and 4 h recovery with: normothermia (N); hypothermia (TH); and hypothermia with phenobarbital (TH+PB). Brain damage was assessed longitudinally at 24 h and 2 weeks using brain magnetic resonance imaging and 12 weeks using histochemical analysis. Motor function was assessed with the beam walk and cylinder tests.
Results
TH and TH+PB induced neuroprotection, as measured by global brain damage score and improved motor function. Exploratory analyses suggest that TH+PB may confer enhanced protection, especially to the extent of damage.
Conclusion
Prophylactic PB with TH is not deleterious and may provide additional long-term neuroprotection, including improvement of motor outcomes following HI in the term-equivalent, neonatal rat.
Similar content being viewed by others
Main
Perinatal asphyxial brain damage resulting in hypoxic–ischemic encephalopathy (HIE) is a major cause of acute neonatal mortality and chronic neurological morbidity in infants and children (1, 2); 20–50% of infants with HIE die within the newborn period; up to 25% of survivors exhibit permanent neuropsychological handicaps. Therapeutic hypothermia (TH) is considered standard therapy for term newborns at risk for evolving encephalopathy (3). Multiple randomized controlled clinical trials have demonstrated significant reduction in death and neurological disability in newborns with HIE treated with TH (4, 5, 6). However, neuroprotection is variable among treated neonates and long-term outcome is not well defined. Thus additional preclinical studies are needed to explore adjunct therapies to improve the efficacy of TH in a larger population of affected newborns.
There have been multiple experimental investigations into TH, alone and with other adjunct therapies in neonatal rodents; the results are variable. Most animal studies used the P7 rat model as originally described (7). However, the P7 rat brain more closely approximates a preterm 32–36 week gestational age infant, potentially making it less relevant to the full-term newborn, for which TH is currently approved (8). Our laboratory recently described a reproducible, preclinical model of HI plus TH in the more relevant, P10–12 animal, which closely approximates a full-term 36–40 week (gestational age) infant (9). With this model, we demonstrated that TH reduces neurodegeneration and improved outcome after HI with significant long-term protection beyond 10 weeks of recovery (9).
Seizures are common in infants with HIE undergoing TH and may exacerbate brain injury (10, 11). In the Cool Cap Study, seizures at enrollment were evident in approximately 60% of patients and had a negative impact on neurodevelopmental outcome (12). Phenobarbital (PB), a gamma-amino-butyric acid (GABA) agonist, is recommended as the first-line antiepileptic drug to treat seizures in infants (13, 14). Seizures are often intractable once initiated (14), making the prophylactic use of antiepileptic drugs prior to seizure onset a potential option. There have been limited animal and clinical studies investigating the adjunctive neuroprotective effect of combining TH with PB, with conflicting results (15, 16, 17, 18). Additionally, the timing of administration of the drug varied among these studies, which may have impacted outcome.
There are controversies surrounding the use of prophylactic PB due to its potential effect on neuronal apoptosis in rodent models (19, 20, 21, 22). However, these studies were performed in otherwise healthy animals as compared with animals with HI brain injury, in which the neuroprotective benefits of PB may outweigh the risks of potential apoptosis. Therefore, the adjunctive neuroprotective effect vs. risk of prophylactic PB with TH in HIE on long-term outcomes remains unclear and warrants further study.
Thus the objective of this initial study was to determine whether prophylactic PB is an effective, and not deleterious, additive intervention with hypothermia for neuroprotection following HI in the term-equivalent neonatal rat. The primary hypothesis was that TH+PB is at least as protective as TH alone, with additional statistics to explore a potential benefit of adding PB over TH alone. We intentionally aimed for a moderate insult in order to demonstrate either enhanced neuroprotection or injury exacerbation from PB-induced cell death. The study was designed to evaluate each animal longitudinally and examine differences across treatments at each time point. Our primary outcome measures included both neuroanatomic and motor function but not the effect of PB on seizure modulation.
Methods
Animal Model of Unilateral HI Plus Hypothermia
Timed pregnant Wistar rats (Charles River Laboratories, Wilmington, MA) in groups of three were purchased on embryonic day (E) 15, housed individually, and allowed to deliver vaginally. On the day of birth, pups were randomized among the 3 dams, 10/litter, with equal male and female pups. On the day of the experiment, we weighed all of the animals and excluded animals that were not within our average weight range for P10 pups of 18–22 g. Each HI experiment then involves 20 animals. Unilateral HI was induced in the right hemisphere at P10 according to our standard protocol permanent ligation of the right common carotid artery, 90 min recovery with the dam, followed by hypoxia (8% O2/balance N2). Determination of the relation between duration of hypoxic exposure and pathological end point is a standard part of our procedure prior to each set of experiments. Preliminary validation experiments confirmed that a hypoxic duration of 80–85 min produced predominantly moderate damage and was utilized for this set of experiments. During hypoxia, the temperature in the chamber was maintained at 34.5 °C to achieve an average rectal temperature of 36–36.5 °C (nesting temperature), monitored in two non-ligated pups (Physitemp, Clifton, NJ). Following hypoxia, pups were randomly assigned to three groups: normothermic (N), therapeutic hypothermia (TH), and therapeutic hypothermia+phenobarbital (TH+PB). The goal was for six pups/experimental group plus two naive controls, adjusted as necessary due to deaths during HI. Pups were injected subcutaneously with 0.1 mL (20 mg/kg) of either phosphate-buffered saline (N, TH) or PB (TH+PB) within 10 min of completion of HI and again 30 min later (total dose of 40 mg/kg). TH was achieved as previously described (9). Briefly, pups in both the hypothermic groups were placed in open jars in a water bath (28–30 °C) to maintain a target rectal temperature of 32 °C; normothermic pups were maintained in the original chamber at 34.5 °C in room air for 4 h. Rectal temperatures were monitored hourly. A total of six pups died either during or shortly following HI. Pups were returned to the dams, adding non-experimental littermates to maintain litters of 10, and weaned at P21. In this series of experiments, one of the litters exhibited weight loss following the 24 h magnetic resonance imaging (MRI), attributed to maternal neglect, and were removed from the cohort, resulting in a total of 39 experimental animals to which we added 1–2 naive controls depending on the analysis. Animals were randomly divided into three groups as follows: N (n=9), TH (n=15), and (TH+PB (n=15). Following MRI and behavioral analyses, animals were deeply anesthetized with a fatal dose of pentobarbital prior to perfusion fixation with 4% paraformaldehyde. All procedures were approved by the Weill Cornell Medical College Animal Care and Use Committee (IACUC).
MRI Analysis
Acquisition of images: T2-weighted images were acquired at 24 h and 2 weeks post-HI using a RARE sequence on a Bruker Biospec 7.0-T MR (Bruker Biospec Corp., Billerica, MA, USA) scanner with the following acquisition parameters: RARE factor 10, matrix 256 × 256, field of view 20 × 20 mm2, slice thickness 1 mm, 17 contiguous coronal sections at P11 and 20 contiguous coronal sections at P25; TReff=2,191.1 ms at P11 and 25.8 ms at P25, TEeff 42.9 ms. A 72 mm Bruker linear coil was used for excitation and a quadrature brain coil was used for signal reception. MRI images from Bregma 2.52 to −5.40 (8 images) were given gross and regional (cortex, hippocampus, thalamus) damage score according to the ordinal scale as previously described (9). This simple scale scores damage across the spectrum from mild to severe with: 0, no damage; 1, mild “atrophy” only; 2, moderate, “atrophy” with ventriculomegaly; 3, moderate–severe, 10–25% infarct; 4, severe, 25–100% infarct; and 5, bilateral injury. It should be noted that the reduction in hemispheric size noted as “atrophy” is not classic atrophy but represents the dynamic balance between cell and ongoing growth of healthy tissue. Regions of interest were traced using the Image J software (NIH, Bethesda, MD) and results used in the exploratory analyses are presented in Table 1.
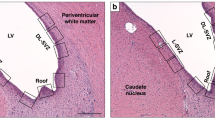
Histochemical Analysis
Following MRI and behavioral analysis, animals were deeply anesthetized with a fatal dose of pentobarbital prior to perfusion fixation with 4% paraformaldehyde. Brains were removed, cryoprotected, and 50 μm sections were cut on a freezing microtome (Microm, Walldorf, Germany). Coronal brain sections from Bregma 2.52 to −5.40 (one out of every sixth section) were mounted onto gelatin-coated slides. The sections were stained with a 1% cresyl violet solution (Sigma, St. Louis, MO) and evaluated with light microscopy (Olympus, Tokyo, Japan). Using the same scoring system used for the MRI, overall and regional damage scores were determined for each section.
Behavioral Analysis
Beam walking test and cylinder test was used to evaluate gross motor function at 6 weeks post-HI. The beam walk test measures the rodent’s ability to traverse an elevated beam, a robust test of locomotor control that is particularly sensitive to hindlimb deficits (23). Rats were tested on two beams of increasing difficulty. Beams were 40 cm long, elevated 32 cm from the table surface. Level 1 beam was flat and 2.5 cm wide; Level 2 beam was a cylindrical rod of 2.5 cm diameter. A dark box was at the end of the beam; rats instinctively advance into the box when placed on a beam. Rats were placed on the beam 10 cm from the box to learn the test. Then each rat was placed 40 cm from the box and given 5 attempts to cross the beam. Videos were recorded and the fails, i.e., inability to cross, and right and left foot slips were recorded by an investigator blinded to the treatment. Videos were analyzed for right and left (affected hindlimb) slips and falls. Inclusion criteria: all animals were required to have data from both difficulty levels, i.e., either complete crossing or fall. Animals failing to meet this, by group, were as follows: N, 1 animal did not initiate level 2, 7/8 included; TH 1 animal failed/incomplete data, 1 animal outlier >2.5 SD from mean), 12/14 included; TH+PB: 1 animal incomplete data, 13/14 included; CON: 4 animals either failed to initiate or had incomplete data, 4/8 included.
In the cylinder test (24), each animal was placed into a clear cylinder for 3 min. Exploratory behavior was recorded by a video camera, and the use of ipsilateral, contralateral, and both forepaws were scored during the vertical exploration along the cylinder walls; frequency of reliance on ipsilateral forepaw and both forepaws was used as an unambiguous measure of motor impairment. There were no exclusions from the cylinder test; all animals were included.
Statistics
All values are expressed as mean±SEM. Hypotheses were one-tailed reflecting the hypothesis that TH, TH+PB and, for behavior, non-ischemic control groups would show less severe brain damage and behavioral deficits than the N group. Protective effects of TH and TH+PB on brain injury were assessed with analysis of variance (ANOVA) or multivariate ANOVA tests as stated in Results with Dunnett’s post hoc tests with the N group as the reference. Exploratory analyses of relative protective effects of TH+PB vs. TH on global brain damage, and specifically on neocortex, hippocampus, and thalamus, were assessed with a multivariate ANOVA within the three brain regions as the multiple outcomes across the three post-HI time points. Comparisons of TH+PB to TH on behavior were conducted with ANOVA with covariates as described. The observed effect size (25) was derived from an exploratory pairwise comparison between treatment groups, and the estimated sample size (26) was required to test the hypothesis (H1) that combined TH+PB treatment has a significantly greater therapeutic benefit than TH alone. Effect sizes estimated from these analyses were used to estimate sample sizes needed to detect a pairwise difference at a power of >0.9.
Results
PB does not Alter Animal Temperature Profile During Hypothermia
PB administration can itself lower body temperature, which might confuse the effects of TH. To examine this effect, P10 pups were treated with the same dose of PB, or saline, to be used in the full study (4 pups/group), placed in the temperature-controlled chamber, and body temperature was measured over 4 h. The mean temperature of the PB-treated pups was 37.0±0.2, which did not differ from the control group of 37.4±0.4. During each subsequent experiment, core body temperature of each animal was monitored using rectal temperature probes during the 4 h of hypothermia. There were no significant differences (P⩾0.05, unpaired t-test) between mean temperatures at any time point for the hypothermia alone (TH) vs. hypothermia and PB (TH+PB) treated animals (Figure 1).
Temperature profile of normothermia (N), therapeutic hypothermia (TH), and therapeutic hypothermia with phenobarbital (TH+PB) rats during therapeutic hypothermia (TH), immediately post-hypoxia–ischemia (post-HI). There were no significant differences between mean rectal temperatures of rats in either the TH or the TH+PB groups at any time point during 4 h of cooling post-HI. The N animals were significantly warmer as compared with both TH and TH+PB animals. (analysis of variance, P<0.05). Data are expressed as mean±SEM.
PB with Hypothermia Confers Both Early and Long-Term Neuroprotection
Brain damage was evaluated longitudinally with in vivo brain MRI at 24 h and 2 weeks post-HI and post-mortem at 12 weeks (following completion of behavioral testing) using histologically processed brain sections. The images depicted in Figure 2 demonstrate the progression of injury/repair in representative animals from each group. MRIs and histological sections for all of the animals were analyzed using our standard damage score system (9) as described in Methods section.
Effects of normothermia (N), therapeutic hypothermia (TH), and therapeutic hypothermia with phenobarbital (TH+PB) on progression of injury following hypoxia–ischemia: sequential T2-weighted magnetic resonance imaging (T2MRI) and histology. Representative MRI images obtained from one N (a–c), one TH (d–f), and one TH+PB (g–i) pup at 24 h (a, d, g), 2 weeks (b, e, h), and 12 weeks (c, f, i). Bar=5 mm. Data are expressed as mean±SEM.
Global protection
Figure 3a–c show the distribution of individual global damage scores for the 3 groups at 24 h, 2, and 12 weeks, respectively. A mixed two-way ANOVA showed a significant effect of treatment (P<0.05) on global damage scores, and changes over time post-HI (P<0.05). Across time points, the ranking across groups was TH+PB<TH<N. Dunnett’s post hoc comparisons of time-average damage scores showed significantly lower damage for the TH and TH+PB groups, relative to the normothermic group (Figure 3d).
Effect of hypoxia–ischemia (HI), therapeutic hypothermia (TH), and therapeutic hypothermia with phenobarbital (TH+PB) on short- and long-term damage scores. Scatterplots showing individual damage scores for rats in the normothermia (N), TH, and TH+PB groups assessed longitudinally at (a) 24 h (magnetic resonance imaging (MRI)), (b) 2 weeks (MRI), and (c) 12 weeks (postmortem histology); and bar graph showing time-averaged damage scores across the treatment groups (d). Analysis of variance showed significant effects of treatment (F(2,31)=4.1, P<0.05) and time after hypoxia–ischemia (F(2,62)=4.9, P<0.05). *P<0.05 TH<N; **P<0.01, TH+PB<N, Dunnett’s post hoc comparisons. Data are expressed as mean±SEM.
PB with Hypothermia Preserves Hemispheric Brain Volume
Whole hemispheric brain volumes were calculated for ipsilateral and contralateral hemispheres on 2-week MRIs. Examination of individual ipsilateral/contralateral ratios is a measure of extent of growth of the injured, relative to the contralateral, hemisphere. An abnormality in the contralateral hemisphere is determined by comparison with control. Contralateral volumes were not significantly different from controls in any group (P>0.05) (Figure 4a). We noted a significant increase in the hemispheric ratio across the three groups: N 0.77±0.04, TH 0.84±0.03, TH+PB 0.92±0.03, P<0.01, ANOVA (Figure 4b). Hypothermia alone did not significantly protect brain volume (P>0.05) in this cohort of animals. However, hypothermia coupled with PB led to a significant increase in this ratio (P<0.01).
Effects of normothermia (N), therapeutic hypothermia (TH), and therapeutic hypothermia with phenobarbital (TH+PB) on ratio of ipsilateral/contralateral hemispheric brain volume post-hypoxia–ischemia. Volume of healthy brain tissue in contralateral and ipsilateral hemispheres were calculated from 2-week magnetic resonance images as described in Methods section. Data are expressed as mean±SEM. (a) Contralateral volumes: There were no significant differences between contralateral hemispheric brain volumes. (b) Combination therapy with hypothermia and phenobarbital conferred the most significant neuroprotection. Effects of treatment determined by one-way analysis of variance, *P<0.05 less damage than normothermic group, Dunnett’s post hoc comparisons.
PB with Hypothermia Improves Motor Function
To characterize protection of sensorimotor function conferred by TH and TH+PB, rats were tested as young adults (P50–70) on the beam walk and cylinder tests (Figure 5).
Improvement in beam walking and cylinder test by therapeutic hypothermia (TH) and therapeutic hypothermia with phenobarbital (TH+PB) treatments. (a) Beam test: Treatment group × beam difficulty × side analysis of variance (ANOVA) showed highly significant differences in the frequency of slips across treatment groups (F(3,31)=4.7, P<0.01) and side of body (left>right; F(1,31)=24.8, P<0.001). Dunnett’s post hoc tests showed that, relative to the normothermia (N) group, TH (*P<0.05) and TH+PB (**P<0.01) groups showed fewer total slips. (b) Cylinder test: ANOVA showed significant group differences in the total number of contacts with ipsilateral forepaw (F(3,31)=3.8, P<0.05). Post hoc Dunnett’s comparison (one-tailed) showed that, compared with N rats, TH (*P<0.05) and TH+PB (**P<0.01) rats were significantly less impaired. Data are expressed as mean±SEM.
TH and TH+PB animals showed improvement in beam walking (Figure 5a). Treatment group × beam difficulty × side ANOVA showed highly significant differences in the frequency of slips across treatment groups (P<0.01) and side of body (left>right; P<0.001); Normothermic rats were significantly impaired relative to all other groups (Dunnett’s post hoc comparisons, P<0.05). TH and TH+PB treatments each produced significant improvement relative to N (P<0.05, P<0.01, respectively).
Normal rodent behavior in the cylinder test is to rear, either standing free on back legs or contacting the wall with one forepaw or the other, with more contacts by the dominant forepaw (24). Impairment is indicated by preferential use of the forepaw ipsilateral to the lesion, alone or both forepaws simultaneously. Relative to N, TH and TH+PB animals showed significantly less use of the ipsilateral forepaw (Figure 5b), (P<0.05, TH; P<0.01, TH+PB).
Exploratory analyses comparing TH+PB to TH
The above data suggest that adding PB to TH may augment the neuroprotective effects of TH, which would be important to test with future studies. Exploratory analyses of treatment were run to estimate the effect sizes of TH+PB compared with TH and the sample sizes needed to detect this difference with statistical significance (Table 1). Table 1 shows the results of these analyses for global damage scores and for regions of interest, i.e., neocortex (Ctx), hippocampus (Hipp), and thalamus (Thal), as well as behavior. Relative to behavior, neuroanatomical measures are more sensitive to the potential benefit of PB, with regional effect size ranking Ctx>Hipp>Thal.
Discussion
To our knowledge, this is the first study that has demonstrated an enhanced, long-term neuroprotective effect of prophylactic PB with TH following cerebral HI in the neonatal rat. This study used the P10 animal to more closely model the clinical situation of TH following intrapartum HI in the term infant, for whom cooling is the standard practice (8, 9). Neuroprotection was notable for a reduction of gross and regional brain damage scores at 24 h and 2 weeks on MRI and 12 weeks on histology (Figure 2) coupled with an increase in ipsilateral/contralateral hemispheric brain volume ratios at 2 weeks on MRI (Figure 4). TH and TH+PB also improved motor function on both the beam walk and cylinder tests.
Hypothermia alone conferred long-term neuroprotection at 2 and 12 weeks post-HI, but not at 24 h, consistent with previously reported data from our laboratory (9). Our previous study demonstrated more significant neuroprotection with cooling than we report here. However, that study was performed with a larger number of animals and the significant effect of cooling was seen only when animals were divided into moderate and severe cohorts.
Animal-to-animal variability in this model is well known. Since the original publication in 1982, we, and others, have made numerous technical adjustments to minimize the variability, including controlling litter size, reduced time of anesthesia, and prewarming prehypoxia. However, as in human infants, there is still a variable response to HI, ranging from none to mild, moderate, or severe. In this study, as in all studies in our laboratory, we first validate the relation between duration of hypoxia and degree of injury. For the purpose of this study, we aimed for a moderate degree of brain injury, which increases the variability. Additionally, the therapeutic effect of hypothermia is also variable, with the greatest benefit in the context of moderate injury in both clinical trials and experimental studies. A mild degree of injury could have limited the ability to detect an effect of the hypothermia alone, as we previously reported (9), or combined with PB. However, although TH is protective in the context of a severe insult (9), it might have been difficult to detect potential exacerbation of cell death due to PB itself.
Importantly, in addition to the protective effects of TH+PB on brain damage, the present study demonstrated reproducible improvement on motor function using two different functional tests. Defects in locomotor and cognitive function are common in children with HIE and experimental animals following unilateral HI (27). An effective neuroprotective intervention must include long-term functional improvement, in addition to reduction in brain damage. Injury to the ipsilateral sensorimotor cortex is characteristic of this animal model and the resulting motor impairments can be reliably detected by both the beam walk test (23) and cylinder test (24). Rat pups treated with combined TH+PB showed highly significant improvement of motor function, relative to their corresponding normothermic littermates, assessed with both beam and cylinder test. We did not perform novel object recognition, a behavioral test of temporal lobe-mediated object memory, as our previous study did not show any differences between N and TH animals (9).
Previous clinical studies have examined the use of PB as a neuroprotective agent. A small prospective, randomized clinical trial showed that 40 mg/kg of PB given to non-cooled, term infants with perinatal asphyxia did not reduce the incidence of clinical seizures but reduced the incidence of cerebral palsy at 3 years of age (18). Two retrospective clinical studies examined the adjunctive use of PB with cooling with opposing results. One found that prophylactic PB with cooling led to a significant reduction of clinically detectable seizures and was associated with improved neurodevelopmental outcome at 18 months (17). However, another study found that PB with cooling was associated with an increase in death or abnormal brain MRI (16). These clinical studies were limited by small size, retrospective design, and a more severe degree of encephalopathy in the PB group in the latter study.
We speculate that PB may act via several mechanisms, including a reduction of seizure burden and cerebral excitation. HIE is a common cause of seizures that have been show to worsen outcome in infants with HI brain injury (28). Although hypothermia alone has antiepileptic effects (29), seizures often persist (30, 31). PB exerts a cerebral inhibitory effect by prolonging and potentiating the action of GABA on the GABAA receptor leading to hyperpolarization of neurons (32). One study found that PB reduced the amplitude and propagation of seizures in term infants with varying etiologies, including HIE (33). Other potential neuroprotective mechanisms of PB include decreased cerebral metabolism and oxygen consumption, stabilization of neuronal cell membranes, and reduced free radical generation (34). A secondary analysis of the Whole Body Hypothermia Trial demonstrated that PB administration prior to cooling was associated with lower mean temperatures and a shorter time to hypothermic temperatures (35). It is unlikely that PB acted via modulation of temperature in the present study, as we found no significant difference in the temperature profile of TH or TH+PB animals. Significant controversies remain surrounding the use of PB in the neonate due to potential enhancement of neuronal apoptosis. PB given to healthy, P7 rats resulted in profound apoptotic neurodegeneration with a dose-dependent response in several studies (19, 20, 21, 22). A second study in P7 rats found that PB resulted in hippocampal neuronal degeneration and a decrease in the expression of glutamate receptor subunits (33). However, these studies were performed in healthy, preterm equivalent animals, coinciding with the brain growth spurt period (22), and not in term-equivalent animals subjected to HI with or without subsequent hypothermia, as in our study. Furthermore, evidence of PB-induced neuronal apoptosis has only been demonstrated in animal models and not in human studies. Additionally, these studies evaluated acute effects on apoptosis (24 h) with no long-term neuropathological, functional, or behavioral outcomes. The present study evaluated long-term outcomes and demonstrated a lasting improvement both on brain growth and on motor function in animals treated with PB and cooling. HI is a known cause of neuronal apoptosis and necrosis; however, hypothermia is neuroprotective by reducing both pathways of cell death (36). Our study did not specifically examine apoptosis, however, we found better preservation of ipsilateral brain volume 2 weeks after HI with the combined use of hypothermia and PB. Contralateral hemispheric volumes, which were also exposed to PB, were not altered as compared with control volumes. This likely indicates a lack of significant cell death due to PB. Therefore, the data suggest that the neuroprotective benefits of PB with hypothermia after HI may outweigh the potential risks of neuronal apoptosis caused by PB itself.
A major strength of this study is the longitudinal evaluation of each animal from initial injury through to behavioral outcome and histochemical analysis. In the context of the large main effects of treatment observed in this study, this approach can be used to analyze the time course of recovery for each treatment. Moreover, this design allows for examination of neuropathological–behavioral correlations over time, harnessing the well-known animal-to-animal viability within the HI model. The exploratory analyses of treatment in specific brain regions of interest suggested regional differences in the protection conferred by TH and TH+PB. Future studies could be designed to determine regional differences in protective effects of treatment.
A limitation of this study is the absence of behavioral and electrophysiological data on seizure burden and lack of pharmacokinetic data for PB. Assessing these variables was beyond the scope of the present study, which was an initial proof of principle of the therapeutic potential of adding PB treatment to TH. Another slight limitation was the immediate initiation of treatment following HI, rather than testing efficacy over intervals.
In conclusion, prophylactic PB with hypothermia following HI confers long-term neuroprotection as demonstrated by a reduction of brain injury and improvement of motor function in the term-equivalent, neonatal rat. The extent of this protection is at least as strong as TH alone and may warrant future studies to determine added benefit (37).
References
Wu YW, March WM, Croen LA et al. Perinatal stroke in children with motor impairment: a population-based study. Pediatrics 2004;114:612–9.
Vannucci RC . Hypoxic-ischemic encephalopathy. Am J Perinatol 2000;17:113–20.
Gonzalez FF, Ferriero DM . Therapeutics for neonatal brain injury. Pharmacol Ther 2008;120:43–53.
Shankaran S, Pappas A, McDonald SA et al. Childhood outcomes after hypothermia for neonatal encephalopathy. N Engl J Med 2012;366:2085–92.
Gluckman PD, Wyatt JS, Azzopardi D et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicenter randomized trial. Lancet 2005;365:663–70.
Azzopardi DV, Strohm B, Edwards AD et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med 2009;361:1349–58.
Rice JE, Vannucci RC, Brierley JB . The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 1981;9:131–41.
Patel SD, Pierce L, Ciardiello AJ et al. Neonatal encephalopathy: pre-clinical studies in neuroprotection. Biochem Soc Trans 2014;42:564–8.
Patel SD, Pierce L, Ciardiello A et al. Therapeutic hypothermia and hypoxia-ischemia in the term-equivalent neonatal rat: characterization of a ranslational pre-clinical model. Pediatr Res 2015;78:264–71.
Tekgul H, Gauvreau K, Soul J et al. The current etiologic profile and neurodevelopmental outcomes of seizures in term newborn infants. Pediatrics 2006;117:1270–80.
Yap V, Engel M, Takenouchi T, Perlman JM . Seizures are common in term infants undergoing head cooling. Pediatric Neurol 2009;41:327–31.
Gluckman PD, Wyatt JS, Assopardi D et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomized trial. Lancet 2005;365:663–70.
Slaughter LA, Patel AD, Slaughter JL . Pharmacological treatment of neonatal seizures: a systematic review. J Child Neurol 2013;28:351–64.
Mathieson SR, Livingstone V, Low E, Pressler R, Rennie JM, Boylan GB . Phenobarbital reduces EEG amplitude and propagation of neonatal seizures but does not alter performance of automated seizure detection. Clin Neurophysiol 2016;127:3343–50.
Barks JD, Liu YQ, Shangguan Y, Silverstein FS . Phenobarbital augments hypothermic neuroprotection. Pediatr Res 2010;67:532–7.
Sarkar S, Barks JD, Bapuraj JR et al. Does phenobarbital improve the effectiveness of therapeutic hypothermia in infants with hypoxic-ischemic encephalopathy? J Perinatol 2012;32:15–20.
Meyn DF Jr, Ness J, Ambalavanan N, Carlo WA . Prophylactic phenobarbital and whole-body cooling for neonatal hypoxic-ischemic encephalopathy. J Pediatr 2010;157:334–6.
Hall RT, Hall FK, Daily DK . High-dose phenobarbital therapy in term newborn infants with severe perinatal asphyxia: a randomized, prospective study with three-year follow-up. J Pediatr 1998;132:345–8.
Kaushal S, Tamer Z, Opoku F, Forcelli PA . Anticonvulsant drug-induced cell death in the developing white matter of the rodent brain. Epilepsia 2016;57:727–34.
Forcelli PA, Kim J, Kondratyev A, Gale K . Brief communication: Pattern of antiepileptic drug induced cell death in limbic regions of the neonatal rat brain. Epilepsia 2011;52:e207–11.
Katz I, Kim J, Gale K, Kondratyev A . Effects of lamotrigine alone and in combination with MK-801, phenobarbital, or phenytoin on cell death in the neonatal rat brain. J Pharmacol Exp Ther 2007;322:494–500.
Bittigau P, Sifringer M, Ikonomidou C . Antiepileptic drugs and apoptosis in the developing brain. Ann NY Acad Sci 2003;993:103–14 discussion 123–4.
Goldstein LB . Model of recovery of locomotor ability after sensorimotor cortex injury in rats. ILAR J 2003;44:125–9.
Schallert T . Behavioral tests for preclinical intervention assessment. Neuropharmacology 2006;3:497–504.
Cohen J . “A power primer”. Psychol Bull 1992;112:155–9.
Faul F, Erdfelder E, Lang A-G, Buchner A . G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods, (2007;39:175–91.
Schallert T, Fleming SM, Leasure JL, Tillerson JL, Bland ST . CNS plasticity and assessment of forelimb sensorimotor outcome in unilateral rat models of stroke, cortical ablation, parkinsonism and spinal cord injury. Neuropharmacology 2000;39:777–87.
Glass HC, Glidden D, Jeremy RJ, Barkovich AJ, Ferriero DM, Miller SP . Clinical neonatal seizures are independently associated with outcome in infants at risk for hypoxic-ischemic brain injury. J Pediatrics 2009;5:318–23.
Boylan GB, Kharoshankaya L, Wusthoff CJ . Seizures and hypothermia: importance of electroencephalographic monitoring and considerations for treatment. Semin Fetal Neonatal Med 2015;20:103–8.
Low E, Boylan GB, Mathieson SR et al. Cooling and seizure burden in term neonates: an observational study. Arch Dis Child Fetal Neonatal Ed 2012;97:F267–72.
Lynch NE, Stevenson NJ, Livingstone V et al. The temporal characteristics of seizures in neonatal hypoxic ischemic encephalopathy treated with hypothermia. Seizure 2015;33:60–5.
Mathieson SR, Livingstone V, Low E, Pressler R, Rennie JM, Boylan GB . Phenobarbital reduces EEG amplitude and propagation of neonatal seizures but does not alter performance of automated seizure detection. Clin Neurophysiol 2016;127:3343–50.
Liu Y, Wang XY, Li D, Yang L, Huang SP . Short-term use of antiepileptic drugs is neurotoxic to the immature brain. Neural Regen Res 2015;10:599–604.
Singh D, Kumar P, Majumdar S, Narang A . Effect on phenobarbital on free radicals in neonates with hypoxic ischemic encephalopathy – a randomized controlled trial. J Perinat Med 2004;32:278–81.
Sant’Anna G, Laptook AR et al. Phenobarbital and temperature profile during hypothermia for hypoxic-ischemic encephalopathy. J Child Neurol 2012;27:451–7.
Ohmura A, Nakajima W, Ishida A et al. Prolonged hypothermia protects neonatal rat brain against hypoxic-ischemia by reducing both apoptosis and necrosis. Brain Dev 2005;27:517–26.
Shetty J . Neonatal seizure in hypoxic-ischemic encephalopathy – risks and benefits of anticonvulsant therapy. Dev Med Child Neurol 2015;57 (Suppl 3): 40–3.
Acknowledgements
We thank Dr. Shyama Patel and Bradley Hutton for their assistance and contribution to these studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Statement of Financial Support
This work was supported in part by grants from the LeDucq Foundation, France and National Institutes of Health, USA (NIH)/R21NS083425 (both to S.J.V.). H.M. receives support from the Sidney R. Baer, Jr. Foundation and the New York State Office of Mental Health.
Rights and permissions
About this article
Cite this article
Krishna, S., Hutton, A., Aronowitz, E. et al. The effects of adding prophylactic phenobarbital to therapeutic hypothermia in the term-equivalent hypoxic–ischemic rat. Pediatr Res 83, 506–513 (2018). https://doi.org/10.1038/pr.2017.266
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2017.266
This article is cited by
-
Mild Hypothermia Protects Brain Injury After Intracerebral Hemorrhage in Mice Via Enhancing the Nrdp1/MyD88 Signaling Pathway
Neurotoxicity Research (2022)
-
High-Dose Melatonin and Ethanol Excipient Combined with Therapeutic Hypothermia in a Newborn Piglet Asphyxia Model
Scientific Reports (2020)
-
Adjunctive Neuroprotective Therapies for Treatment of Hypoxic-Ischemic Encephalopathy (HIE)
Current Pediatrics Reports (2020)
-
Acute LPS sensitization and continuous infusion exacerbates hypoxic brain injury in a piglet model of neonatal encephalopathy
Scientific Reports (2019)
-
Evaluating anti-epileptic drugs in the era of therapeutic hypothermia
Pediatric Research (2019)