Abstract
Background:
Oral propranolol reduces retinopathy of prematurity (ROP) progression, although not safely. This study evaluated safety and efficacy of propranolol eye micro-drops in preterm newborns with ROP.
Methods:
A multicenter open-label trial, planned according to the Simon optimal two-stage design, was performed to analyze safety and efficacy of propranolol micro-drops in newborns with stage 2 ROP. To this end, hemodynamic and respiratory parameters were monitored, and blood samples were collected weekly, for 3 wk. Propranolol plasma levels were also monitored. The progression of the disease was evaluated with serial ophthalmologic examinations.
Results:
Twenty-three newborns were enrolled. Since the fourth of the first 19 newborns enrolled in the first stage of the study showed a progression to stage 2 or 3 with plus, the second stage was prematurely discontinued. Even though the objective to complete the second stage was not achieved, the percentage of ROP progression (26%) was similar to that obtained previously with oral propranolol administration. However, no adverse effects were observed and propranolol plasma levels were significantly lower than those measured after oral administration.
Conclusion:
Propranolol 0.1% eye micro-drops are well tolerated, but not sufficiently effective. Further studies are required to identify the optimal dose and administration schedule.
Similar content being viewed by others
Main
Retinopathy of prematurity (ROP) is a sight-threatening disease due to pathological angiogenesis that occurs in the incompletely vascularized retina of preterm newborns. Despite current therapeutic strategies, ROP still represents a significant cause of morbidity and disability in childhood, and as many as ~50,000 preterm infants worldwide become blind or visually impaired from ROP each year (1). Although ROP has been recognized as a relevant cause of blindness in high-income countries since the 1940s and 1950s, while survival rates of most preterm and very-low-birth-weight babies were improving, in the early 1990s an emerging epidemic of blindness due to ROP was also recorded in middle-income countries (2). Currently, Asia is the region presenting the highest incidence of blindness due to ROP, followed by Latin America, where some countries account for an incidence of blindness/severe visual impairment related to ROP that is 2.4 times higher than in highly industrialized countries (1,3,4,5,6). Therefore, the detection of a new inexpensive and easily affordable treatment strategy might be a relevant issue of global interest.
Apart from the reduction in oxygen tension, which may be considered the master regulator inducing the expression of angiogenic growth factors in proliferative retinopathies, other mechanisms including the activation of inflammatory signaling pathways, oxidative stress, and the production of nitric oxide are involved in the vascular response to ischemia/hypoxia (7). Recently, several studies performed using the C57BL/6J mouse model of oxygen-induced retinopathy (OIR) (8,9) to analyze the role of the β-adrenergic system in the pathogenesis of ROP (10,11,12) have demonstrated that retinal exposure to hypoxia results in an increase of the catecholamine release, which participates in the up-regulation of proangiogenic factors leading to retinal angiogenesis (11). In addition, these studies have shown that β-adrenoreceptor (β-AR) blockade by the nonselective β1/β2-AR antagonist propranolol prevents both the up-regulation of proangiogenic factors and retinal neovascularization (10,11,12). The observation that vascular abnormalities in the superficial plexus that characterize OIR are abolished in β1/2-AR knockout mice, while the development of the deep plexus is aided (13), confirms the pivotal role of β2-ARs in the pathogenesis of OIR and the possible efficacy of propranolol. Conflicting results have been reported in the 129S6 mice (14), a strain with a predisposition to develop a more aggressive neovascularization (15) and characterized by an enormous increase in the expression of β3-ARs (14). This characteristic may be responsible for the insensitivity to propranolol of this strain, as β3-ARs are only minimally blocked by propranolol (16). This discrepancy is most likely due to the different genetic background of the mice that may have contributed to the different responses of the retina to hypoxia (17).
The efficacy of propranolol in inhibiting retinal neo-vascularization in mouse models suggests a potential therapeutic role also in preterm newborns. Propranolol is commonly used in newborns as an antiarrhythmic drug to treat supraventricular tachycardia (18), neonatal thyrotoxicosis (19), hypertension (20), and hypercyanotic spells in newborns with Fallot’s tetralogy (21). Therefore, a pilot randomized controlled trial was performed (22) to verify the efficacy and safety of oral propranolol in preterm newborns with an advanced stage of ROP (stage 2 without plus in zone II) (23). Oral propranolol proved to be effective in reducing ROP progression, as also confirmed by other studies (24,25,26), and its possible role in ROP prevention is currently under investigation (Sanghvi KP, Singh U, manuscript in preparation).
However, serious adverse events including severe bradycardia and hypotension have been observed, and even though they occurred mainly in conjunction with other conditions (i.e., sepsis, anesthesia or tracheal stimulation), these findings did not suggest that oral administration was a guarantee of adequate safety (22). Nevertheless, topical administration of propranolol was tested in animal models and resulted in being effective in reducing proangiogenic factors and inhibiting retinal neo-vascularization (27), thus also ensuring plasma drug concentrations significantly lower than oral propranolol and an optimal tolerability profile, characteristics that suggest a reduced risk of adverse events (28).
The aim of this study was to evaluate the safety and efficacy of propranolol 0.1% eye micro-drops in preterm newborns with an advanced stage of ROP.
Methods
Definitions
In order to establish the location and severity of ROP, the standard international ROP classification was adopted (23).
Patients
A multicenter, open-label, pilot trial was performed in order to analyze the safety and efficacy of propranolol eye micro-drops in treating preterm newborns with gestational age <32 wk, diagnosed with stage 2 ROP without plus in zone II (23), who were admitted to the neonatal care units (NICUs) taking part in the study (NICUs of A. Meyer University Children’s Hospital of Florence; University Hospital of Siena; and Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, University of Milan). The exclusion criteria included newborns with heart failure, hypotension, recurrent bradycardia (heart rate <90 beats per min), second or third degree atrio-ventricular block and congenital cardiovascular anomalies, except for persistent ductus arteriosus, patent foramen ovale and small ventricular septal defects; newborns with renal failure, parenchymal cerebral hemorrhage, and other diseases that contraindicate the use of β-AR blockers on enrollment were also excluded.
Treatment was started immediately after stage 2 ROP was diagnosed at the discretion of the examiners (R.P. and P.F. for Meyer Hospital of Florence; S.O. for Mangiagalli Hospital of Milan; and M.V. for Le Scotte Hospital of Siena). The newborns were enrolled without stratification by gestational age. All newborns enrolled received propranolol treatment as an ophthalmic solution (concentration 0.1%): three micro-drops of 6 μl propranolol solution (6 μg propranolol every microdrop) were topically applied in each eye by nursses using a variable volume pipette, three times daily (every 8 h). After administration, the nasolacrimal duct was carefully compressed for 30 s to decrease the percentage of the drug absorbed through the conjunctival and nasal vessels. The procedure was recorded in the newborns’ medical records.
It was initially planned to continue this treatment until complete development of retinal vascularization, but no longer than 60 d. The treatment was discontinued at least 24 h before surgery and/or anesthesia, restarted again when the newborns reached clinical stability at the discretion of the treating physician. In fact, unstable newborns (i.e., after anesthesia induction) have previously shown a high risk of adverse events (hypotension and bradycardia) after systemic propranolol administration (22). The ophthalmologic approach for the newborns enrolled in this study was in accordance with the guidelines adopted by the ETROP Cooperative Group and the AAP/AAO/AAPOS guidelines (29,30). Therefore, newborns with ROP who progressed to stage 2 plus or stage 3 plus were treated with laser photocoagulation or intravitreal antivascular endothelial growth factor (bevacizumab) administration (30). The ophthalmologists chose the treatment they considered most appropriate.
Eye-drops were prepared by diluting propranolol hydrochloride powder purchased from A.C.E.F. (Fiorenzuola d’Arda, Piacenza, Italy), in sterile water for injections at a concentration of 1%. Following this, the propranolol 0.1% solution was obtained in a horizontal laminar flow hood by adding 9 ml of sterile saline solution to 1 ml of the propranolol 1% preparation. The solution was prepared sterilely in compliance with the microbiological standards established by European Pharmacopoeia (28). The stability and absence of antimicrobial activity of propranolol eye-drops have recently been reported (28).
Safety
Cardiovascular and respiratory parameters were continuously monitored (Infinity Delta, Dräger Medical System, Telford, PA, and IntelliVue MX800 Philips, Philips Healthcare, Saint-Laurent, Quebec, Canada). Bradycardia was defined as a single heart-rate drop below 100 bpm; apnea, as a pause in breathing for more than 20 s or less when associated with desaturation, bradycardia, pallor, or reduced tone; hypotension, as mean arterial blood pressure less than the tenth centile for gestation/birth weight and postnatal age (31). In addition, blood gas analyses, complete blood counts, glucose levels, serum levels of electrolytes, total protein levels, and renal and liver function tests were measured before starting treatment and once a week for the first 3 wk of treatment. Similarly, electrocardiograms and echocardiograms were performed before starting treatment and once a week for the next 3 wk. In cases of hypotension and/or bradycardia unresponsive to adrenaline, atropine, isoproterenol hydrochloride, terlipressin or glucagon were available. Salbutamol and betamethasone were available for treating cases of bronchospasm. Weight was recorded daily.
Plasma Propranolol Evaluation
Plasma propranolol was monitored by measuring the plasma level on dried blood spots with the liquid-chromatography tandem-mass spectrometry test (32) before starting treatment, during the first 3 d of treatment, and at steady-state on the tenth day of treatment (33).
Efficacy
The main indicator of the efficacy of the propranolol eye-drops treatment was the rate of progression of the disease from stage 2 ROP without plus to stage 2 ROP with plus or stage 3 with plus. Complete ophthalmologic evaluations were performed in accordance with international guidelines (29,30); however, considering the possibility of topical adverse effects, during the first 21 d of treatment these clinical examinations were also performed every 3–4 d. The ophthalmologic exam verified the absence of local adverse events due to treatment with propranolol eye micro-drops, and also monitored the ROP progression using indirect ophthalmoscopy. The RetCam Imaging System II (Clarity Medical Systems, Pleasanton, California) was systematically used by ophthalmologists (R.P. and P.F. for the Meyer Hospital of Florence; S.O. for the Mangiagalli Hospital of Milan; and M.V. for the Le Scotte Hospital of Siena) to compare the ROP evolution.
Stop Criteria and Dose Changes
In the event of any severe adverse events attributable to topical propranolol treatment (bradycardia, bronchospasm, severe hypotension or severe local signs) the study would promptly have been stopped. However, with approval from the Ethic Committee, the study would have been restarted reducing the dosage to two micro-drops of 6 μl propranolol solution (0.1%), in each eye, three times a day. Similarly, if the trial had failed during the first stage because the plasma concentrations of propranolol were higher than 20 ng/ml (the mean plasma concentration observed at steady-state after oral administration of 1 mg/kg/d) (22,33), the study would have been restarted with a reduced dose (two micro-drops, in each eye, three times a day).
Ethical Approval and Informed Consent
The study was approved by the Italian Medicines Agency Institutional Review Board and performed in accordance with the guidelines for human experimentation. The Ethics Committees of all the centers involved in the trial approved this study. Written informed consent was obtained from the parents of the newborns.
Experimental Plan and Data Analysis
This study was planned according to the Simon optimal two-stage design for phase II clinical trials (34). A limited number of patients were enrolled in stage 1: if the number of clinical failures had been more than a preset value, the trial would have been stopped due to failure to demonstrate efficacy. Otherwise, an additional group of patients would have been enrolled in stage 2. If the cumulative number of clinical failures had been greater than another preset value, the trial would have ended by declaring the topical administration of propranolol at a concentration of 0.1% noneffective. Otherwise, the treatment would have been considered sufficiently effective for further investigation. Clinical failure in this study was defined as a progression of ROP to stage 2 or 3 with plus and/or a mean propranolol plasma concentration at the steady-state >20 ng/ml.
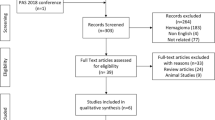
The progression rate from stage 2 ROP to stage 2 or 3 plus previously reported in our units was ~38% (22). The treatment was considered effective if it halved the progression ratio. Hence, considering an alpha error of 0.05 and a power of 80%, the treatment would have been considered noneffective if we had observed at least 4 failures in the first 19 newborns enrolled (stage 1), or at least 12 out of 55 newborns enrolled (stage 2) ( Figure 1 ). The total duration of the study would have been 2 y.
The Simon two-stage optimal design algorithm of the study.
Newborns were divided into two groups, of 23–25 and 26–32 wk to evaluate the safety of propranolol treatment in newborns with different gestational ages. Biochemical data were grouped according with the data of samplings: at enrollment, after 7, 14, and 21 d. The t-test was used to assess possible differences in such data between these groups. Moreover, explorative statistical analyses were conducted to assess the association between predictors and clinical failure. The Fisher’s exact test was used for categorical variables and the Kruskal–Wallis test for continuous variables. The null hypothesis was accepted with a P-value higher than 0.05.
Results
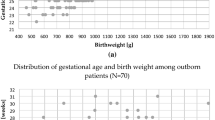
A total of 23 newborns were enrolled and received propranolol eye micro-drops. Treatment was started at 66.5 ± 25 d of life (postmenstrual age 36.3 ± 3.7 wk), as soon as stage 2 ROP was diagnosed. The demographic and obstetric characteristics of the study population are summarized in Table 1 . Fifteen patients (65.2%) were outborn, and the majority was transferred to our NICUs for a surgical emergency. Globally, the comorbidities recorded ( Table 1 ) did not substantially differ from those previously reported in our settings (22) and included a high number of newborns undergoing surgery. Interestingly, 21 newborns (91.3%) underwent at least one surgical operation: 12 surgical closures of patent ductus arteriosus, two neurosurgeries, and 12 abdominal operations (seven for necrotizing enterocolitis, three for bowel perforation, and two for intestinal malformation). Treatment was temporarily discontinued in two newborns (one before a ventriculoperitoneal shunt implant and the other before intestinal recanalization) for 2 and 3 d, respectively.
Safety
During the study, none of the severe adverse events usually related to propranolol (i.e., bradycardia, bronchospasm, apnea, and severe hypotension) or severe local signs due to propranolol eye micro-drops was observed. Hemodynamic and respiratory parameters, continuously monitored during the treatment period, did not present relevant abnormalities, and no significant differences were observed between newborns of different gestational ages (see Supplementary Figures S1 and S2 online). No extended hospital stays were observed for newborns involved in the study due to apnea, bradycardia, or other side effects. No resuscitation was needed during the study.
Electrocardiographic and cardiac ultrasounds were normal in all newborns. Finally, no significant abnormalities were recorded for the variables of blood gas analysis, complete blood count, blood glucose, serum electrolytes, serum total protein, C-reactive protein, renal, and liver function. In particular, no substantial differences were observed between the values on enrollment and the values after 7, 14 or 21 d (see Supplementary Table S1 online).
As shown in Figure 2 , plasma propranolol during the first 3 d of treatment and on the tenth day (steady-state) was consistently below the cut-off value of 20 ng/ml, and ~10 times lower than that reported after oral administration of 1 mg/kg/d of propranolol (22,33). None of the enrolled newborns showed propranolol values higher than 20 ng/ml in any blood samplings, and, therefore, no clinical failure was attributable to excessively high levels of plasma propranolol.
Plasma propranolol concentrations measured by DBS in the 23 newborns (continuous black line), during the first 3 d (a) and in the tenth day of treatment (b), compared with plasma propranolol concentrations obtained in the previous study after oral (1 mg/kg/d) propranolol administration (dotted black line).
Efficacy
The study was discontinued after a total of 23 newborns were enrolled, when the fourth of the first 19 newborns presented a progression of ROP from stage 2 to the threshold for the ophthalmologic treatment (stage 2 or 3 with plus). Therefore, the objective to complete the second stage was not reached. The ophthalmologic outcomes, assessed by RetCam images, are summarized in Table 2 and Figure 3 show three patients treated with eye micro-drops. One newborn was treated for the development of ROP stage 2 plus after only 14 d of eye micro-drops administration. Five newborns developed ROP stage 3 plus. Two of these were treated just 13 and 19 d, because the ROP progressed rapidly; the other three newborns were treated for a longer period (38, 44, and 65 d). Therefore, overall, 6 of the 23 newborns (26.1%; CI 95% 44.0 to 8.1%) showed ROP progression to stage 2 or 3 plus. Five of them belonged to the group with GA 23–25 wk. Three of these received treatment with laser photocoagulation, but in two newborns (three eyes) a progression to stage 4 ROP was recorded, vitrectomy was performed in two eyes of two newborns, and one eye progressed to stage 5 despite a rescue treatment with bevacizumab. The other three newborns were treated with bilateral intravitreal bevacizumab as the first choice, and none of them progressed to a more advanced stage. Interestingly, all these newborns showed a high incidence of comorbidities including more than one surgical operation.
Examples of three newborns enrolled at ROP stage 2 without plus (a, c, e) and treated with propranolol 0.1% eye micro-drops. In the first two patients the progression of ROP stopped (b, d), while in patient 3, stage 3 with plus developed and laser photocoagulation was performed (f).
Two twins (patients 14 and 15), who did not progress to the stage plus, showed a stable ROP at stage 2 for all 60 d of treatment. However, 4–5 d after discontinuing treatment, a rebound of the disease with a progression to stage 3 was observed in both twins. The treatment with propranolol eye micro-drops was resumed for another 15 days, and the ROP regressed. As a result, for the following eight patients the treatment limit was extended to 90 d.
Discussion
The serendipitous demonstration that propranolol promotes the regression of infantile hemangiomas (35), the most common vascular tumor in infancy sometimes associated with ROP (36,37), aroused interest in the involvement of the β-adrenergic system in hypoxia-induced angiogenic processes in humans (36).
The evident relationship between ROP progression and comorbidities characterized by strong clinical stress represents an indirect confirmation of the role of the adrenergic system. The high percentage (~40%) of ROP progression from stage 2 to stage 2 or 3 plus previously reported in our clinical setting may be related to the high number of outborn newborns transferred to our hospitals (all regional reference centers for neonatal surgical diseases) for surgery (22). In this study, more than 90% of the enrolled newborns underwent at least one surgical operation. Even though the association between ROP and surgical treatments has not yet been established, it is reasonable to assume that the stress related to surgical interventions could promote ROP progression.
As a consequence of many observations in the animal model, four pilot clinical trials performed in newborns with ROP stage 2 showed that propranolol administered orally protects newborns from ROP progression (22,24,25,26). Newborns treated with 1–2 mg/kg/d oral propranolol showed mean steady-state plasma concentrations of the drug ranging between 20 and 60 ng/ml, and a significantly reduced progression to stage 3 or stage 3 plus, compared with newborns receiving standard treatment (22). However, some serious adverse effects attributable to this drug have been reported. As a result, we wondered whether topical administration might be a safer strategy to ensure effective retinal concentrations of propranolol.
A recent study performed in the C57Bl/6J mouse OIR model demonstrated that propranolol eye-drops are able to reach the retina, reducing vascular endothelial growth factor and insulin-like growth factor I up-regulation in response to hypoxia, and preventing retinal neo-vascularization (27), indicating that topical eye application might represent an alternative delivery route to systemic administration, thus avoiding the risk of side effects. A more recent study performed in rabbits reported that the administration of propranolol 0.1% eye-drops induces retinal concentrations of this drug similar to those measured after 1 mg/kg/d oral administration, but with significantly lower plasma levels (28). These findings opened the perspective of possible topical treatment with propranolol in newborns with ROP.
This is the first trial that analyzes the therapeutic role of propranolol eye micro-drops in preterm newborns with ROP: the objective was to evaluate whether the topical delivery system could reduce ROP progression while maintaining plasmatic drug concentrations low enough to avoid adverse events.
In order to reduce its systemic absorption, the lacrimal sac at the medial canthus was compressed following the instillation of each microdrop as this blocks the passage of the drug via the nasolacrimal duct to the wide absorptive area of the nasal and pharyngeal mucosa. Moreover, several studies have demonstrated that by reducing the eye-drop volume, the pharmacodynamics effects are maintained, whereas the plasma drug concentration and systemic side effects decrease (38,39,40). In fact, the precorneal area can only contain a small volume of liquid solutions and ~80% of the volume of a standard drop rapidly reaches the lower conjunctival fornix and passes down the nasolacrimal duct (41), contributing to systemic side effects. As a result of these observations, we chose to administer propranolol eye microdrops to newborns enrolled in this study.
Plasma Propranolol Levels
The strategy to use topical administration of 0.1% eye micro-drops allowed us to obtain plasma concentrations of propranolol in our newborns that were significantly lower and more stable than those obtained in a previous study after the oral administration of 1 mg/kg/d ( Figure 2 ). The demonstration that the plasma levels of propranolol in our newborns were very similar to those measured in rabbits after the administration of the same drops (28), allows us to imagine that even in infants the drug’s concentration in the retina could be similar to that obtained with oral administration, as observed in rabbits (28). If so, the availability of a preparation that provides an adequate amount of the drug in the retina with low plasma concentrations could help to overcome the risks of adverse effects as described with the oral preparation (22). While the high incidence of adverse effects after oral propranolol excluded the possibility of testing higher doses of the drug, this study with eye micro-drops offers the possibility of increasing the retinal concentration of propranolol and probably also its efficacy, in view of the fact that its retinoprotective effect is dose-dependent in the animal model (10).
Safety
Similar to what was observed in the study with oral administration, biochemical, hematologic, hemodynamic, and respiratory parameters in newborns treated with propranolol 0.1% eye micro-drops were stable. No adverse effects and no increase in hospitalization were observed after topical administration of propranolol 0.1%. Considering the high prevalence of comorbidities in this study population, the optimal profile of safety and tolerability recorded with topical administration in this type of patient is even more reassuring. These micro-drops were also well tolerated locally, without any signs of topical injury. However, the number of patients treated was too small to make a definitive safety judgment.
Efficacy
As regards the efficacy of propranolol eye micro-drops, the objective to reduce the percentage of progression of ROP to stage 2 or 3 with plus disease to < 19% (half of our historical rate of ROP progression which is the same observed after oral treatment) was not reached after the first stage of the study. In fact, 4 out of 19 newborns showed a progression of ROP to stage 2 or 3 with plus and, therefore, the study was prematurely interrupted. Overall, the ratio of newborns in which ROP progressed to stage 2 or 3 with plus disease was 26%. Even though our ambitious objective was not achieved, the results were substantially similar to those obtained after oral administration of propranolol, but with no adverse effects and definitely low plasma propranolol levels (22). Therefore, this study suggests that topical administration of propranolol could be an effective strategy for counteracting ROP progression, even though some remarks should be made.
Study Limitations
First of all, the number of subjects treated is small and future studies are warranted to increase the sample size.
Second, there is no scientific evidence that topical propranolol gets into human vitreous and reaches the retina or what concentration is required to get there. Therefore, the optimal dosage and concentration of the eye-drops to use in preterm newborns is still uncertain. We prudentially chose a total dose of three 6 µl micro-drops in each eye three times a day (108 µl/d corresponding to 108 µg/d), based on the plasma and retinal propranolol concentrations obtained in the rabbit model (28). However, considering the optimal safety profile that we have demonstrated in preterm newborns, it is likely that this dosage could be increased without compromising the safety and tolerability.
Third, the optimal time to start propranolol treatment is not yet clear. In this study, treatment was started at an advanced stage of ROP (stage 2 without plus), a stage that is quite close to the threshold of ophthalmologic treatment. Half of the newborns who did not improve after propranolol rapidly deteriorated, and treatment with propranolol was limited to a few days. Therefore, starting the therapy more precociously could represent an additional advantage.
The main limitation of current studies in newborns is represented by the availability of antagonists active exclusively on β1 and β2-AR, while recent findings suggest that β3-ARs are also actively involved in hypoxia-induced retinal neo-vascularization. The evidence that propranolol (inactive in blocking β3-AR) failed to suppress retinal neovascularization or the up-regulation of growth factors in an OIR mouse model based on a different strain characterized by an increased expression of β3-AR mRNA (129S6 mice) supports this idea (14). Additionally, the finding that in this mouse strain retinal neovascularization is particularly aggressive (15), suggested that the different genetic background of the mice may have contributed to the different responses of the retina to hypoxia, and that β3-ARs, the up-regulation of which is dramatically more pronounced in 129S6 than in C57BL/6J mice during OIR development, could play a pivotal angiogenic role (17). The involvement of β3-ARs was clearly demonstrated in mouse retinal explants, where β3-ARs have been found to modulate hypoxia-induced vascular endothelial growth factor release through the activation of the nitric oxide signaling pathway (42). The role of β3-ARs is finally confirmed by the finding that selective β3-AR activation leads to the formation of retinal neovascular tufts in β1/2-AR knockout mice (13). In humans, the difference in genetic background has been proposed to explain why ROP progression to severe stages is less frequent in black than in Caucasian infants, even though the disease exhibits the same incidence rate in both populations. The protection in black infants seems to depend on a higher frequency of β-AR polymorphisms, and more specifically on a polymorphism of G protein-coupled receptor kinase 5, which desensitizes β-ARs, thus leading to resistance to noradrenergic stimulus and offering protection against ROP (43). Consequently, the possibility exists that not only in mice but also in humans, the variable therapeutic response to propranolol may depend on differences in genetic background such as a different expression level of retinal β3-ARs. Unfortunately, at present, there are no approved blockers for targeting β3-ARs in humans.
Another limitation of this research is represented by the study design, which does not require the presence of a control group, a group not receiving any treatment or receiving a placebo. The primary purpose of a clinical pilot study concerning a new therapeutic approach is to determine its possible toxicity and/or “biological activity against the disease under study to warrant more extensive development” (34). The possibility of rapidly understanding if a new therapeutic strategy is safe and probably effective is the main advantage of this study design. However, subsequent confirmation from a controlled study with a control group is essential.
Conclusion
This pilot study investigated for the first time the safety and efficacy of a new topical delivery system for the administration of propranolol in newborns with ROP. While propranolol 0.1% eye micro-drops seem to be well tolerated even in high-risk patients, such as preterm newborns with a high prevalence of comorbidities, they are not sufficiently effective. However, the number of newborns evaluated was small and further prospective studies are needed to obtain meaningful conclusions.
In this trial, a very low dosage of propranolol was employed and newborns were enrolled late, when the disease was already at an advanced stage and the entire growth factor cascade has already triggered the angiogenesis. The reassuring safety and tolerability profile of propranolol eye micro-drops together with the very low plasmatic levels, encourages further experimentation with the administering of a higher concentration of propranolol (0.2 %) to newborns at an earlier stage of the disease (ROP stage 1) (NCT02504944). In fact, it is likely that an earlier treatment with propranolol (in coincidence with the beginning of the proangiogenic factors up-regulation) could increase its effectiveness.
Statement of Financial Support
Funding Source: No external funding was secured for this study.
Disclosure
The authors have no financial relationships pertaining to this article. The authors confirm that there is no potential, perceived, or real conflict of interest. No author has a proprietary interest. L.F. wrote the first draft of the manuscript; no honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
References
Blencowe H, Lawn JE, Vazquez T, Fielder A, Gilbert C. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res 2013;74 Suppl 1:35–49.
Gilbert CE, Canovas R, Kocksch de Canovas R, Foster A. Causes of blindness and severe visual impairment in children in Chile. Dev Med Child Neurol 1994;36:326–33.
Gilbert C. Retinopathy of prematurity: a global perspective of the epidemics, population of babies at risk and implications for control. Early Hum Dev 2008;84:77–82.
Gilbert C, Fielder A, Gordillo L, et al.; International NO-ROP Group. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics 2005;115:e518–25.
Zepeda-Romero LC, Barrera-de-Leon JC, Camacho-Choza C, et al. Retinopathy of prematurity as a major cause of severe visual impairment and blindness in children in schools for the blind in Guadalajara city, Mexico. Br J Ophthalmol 2011;95:1502–5.
Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–96.
Scott A, Fruttiger M. Oxygen-induced retinopathy: a model for vascular pathology in the retina. Eye (Lond) 2010;24:416–21.
Smith LE, Wesolowski E, McLellan A, et al. Oxygen-induced retinopathy in the mouse. Invest Ophthalmol Vis Sci 1994;35:101–11.
Chen J, Smith LE. Retinopathy of prematurity. Angiogenesis 2007;10:133–40.
Ristori C, Filippi L, Dal Monte M, et al. Role of the adrenergic system in a mouse model of oxygen-induced retinopathy: antiangiogenic effects of beta-adrenoreceptor blockade. Invest Ophthalmol Vis Sci 2011;52:155–70.
Dal Monte M, Martini D, Latina V, Pavan B, Filippi L, Bagnoli P. Beta-adrenoreceptor agonism influences retinal responses to hypoxia in a model of retinopathy of prematurity. Invest Ophthalmol Vis Sci 2012;53:2181–92.
Martini D, Monte MD, Ristori C, et al. Antiangiogenic effects of β2-adrenergic receptor blockade in a mouse model of oxygen-induced retinopathy. J Neurochem 2011;119:1317–29.
Dal Monte M, Cammalleri M, Mattei E, Filippi L, Bagnoli P. Protective effects of β1/2 adrenergic receptor deletion in a model of oxygen-induced retinopathy. Invest Ophthalmol Vis Sci 2014;56:59–73.
Chen J, Joyal JS, Hatton CJ, et al. Propranolol inhibition of β-adrenergic receptor does not suppress pathologic neovascularization in oxygen-induced retinopathy. Invest Ophthalmol Vis Sci 2012;53:2968–77.
Chan CK, Pham LN, Zhou J, Spee C, Ryan SJ, Hinton DR. Differential expression of pro- and antiangiogenic factors in mouse strain-dependent hypoxia-induced retinal neovascularization. Lab Invest 2005;85:721–33.
Hoffmann C, Leitz MR, Oberdorf-Maass S, Lohse MJ, Klotz KN. Comparative pharmacology of human beta-adrenergic receptor subtypes–characterization of stably transfected receptors in CHO cells. Naunyn Schmiedebergs Arch Pharmacol 2004;369:151–9.
Filippi L, Dal Monte M, Bagnoli P. Different efficacy of propranolol in mice with oxygen-induced retinopathy: could differential effects of propranolol be related to differences in mouse strains? Invest Ophthalmol Vis Sci 2012;53:7421–3.
Wong KK, Potts JE, Etheridge SP, Sanatani S. Medications used to manage supraventricular tachycardia in the infant a North American survey. Pediatr Cardiol 2006;27:199–203.
Smith C, Thomsett M, Choong C, Rodda C, McIntyre HD, Cotterill AM. Congenital thyrotoxicosis in premature infants. Clin Endocrinol (Oxf) 2001;54:371–6.
Garin EH, Araya CE. Treatment of systemic hypertension in children and adolescents. Curr Opin Pediatr 2009;21:600–4.
Mahmoud AB, Tantawy AE, Kouatli AA, Baslaim GM. Propranolol: a new indication for an old drug in preventing postoperative junctional ectopic tachycardia after surgical repair of tetralogy of Fallot. Interact Cardiovasc Thorac Surg 2008;7:184–7.
Filippi L, Cavallaro G, Bagnoli P, et al. Oral propranolol for retinopathy of prematurity: risks, safety concerns, and perspectives. J Pediatr 2013;163:1570–1577.e6.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of the Retinopathy of Prematurity revisited. Arch Ophthalmol 2005; 123:991–9.
Makhoul IR, Peleg O, Miller B, et al. Oral propranolol vs placebo for retinopathy of prematurity: a pilot, randomised, double-blind prospective study. Arch Dis Child 2013;98:565–7.
Bancalari A, Schade R, Muñoz T, Lazcano C, Parada R, Peña R . Oral propranolol in early stages of retinopathy of prematurity. J Perinat Med 2016 Jul 1;44(5):499–503.
Korkmaz L, Baştuğ O, Ozdemir A, Korkut S, Karaca C, Akin MA, Gunes T, Kurtoglu S, Ozturk MA . The Efficacy of Propranolol in Retinopathy of Prematurity and its Correlation with the Platelet Mass Index. Curr Eye Res. 2016 Jun 3:1–10.
Dal Monte M, Casini G, la Marca G, Isacchi B, Filippi L, Bagnoli P. Eye drop propranolol administration promotes the recovery of oxygen-induced retinopathy in mice. Exp Eye Res 2013;111:27–35.
Padrini L, Isacchi B, Bilia AR, et al. Pharmacokinetics and local safety profile of propranolol eye drops in rabbits. Pediatr Res 2014;76:378–85.
Fierson WM ; American Academy of Pediatrics Section on Ophthalmology; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Association of Certified Orthoptists. Screening examination of premature infants for retinopathy of prematurity. Pediatrics 2013;131:189–95.
Good WV ; Early Treatment for Retinopathy of Prematurity Cooperative Group. Final results of the Early Treatment for Retinopathy of Prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc 2004;102:233–48; discussion 248–50.
Nuntnarumit P, Yang W, Bada-Ellzey HS. Blood pressure measurements in the newborn. Clin Perinatol 1999;26:981–96, x.
Della Bona ML, Malvagia S, Villanelli F, et al. A rapid liquid chromatography tandem mass spectrometry-based method for measuring propranolol on dried blood spots. J Pharm Biomed Anal 2013;78-79:34–8.
Filippi L, Cavallaro G, Fiorini P, et al. Propranolol concentrations after oral administration in term and preterm neonates. J Matern Fetal Neonatal Med 2013;26:833–40.
Simon R. Optimal two-stage designs for phase II clinical trials. Control Clin Trials 1989;10:1–10.
Léauté-Labrèze C, Dumas de la Roque E, Hubiche T, Boralevi F, Thambo JB, Taïeb A. Propranolol for severe hemangiomas of infancy. N Engl J Med 2008;358:2649–51.
Praveen V, Vidavalur R, Rosenkrantz TS, Hussain N. Infantile hemangiomas and retinopathy of prematurity: possible association. Pediatrics 2009;123:e484–9.
Filippi L, Dal Monte M, Casini G, Daniotti M, Sereni F, Bagnoli P. Infantile hemangiomas, retinopathy of prematurity and cancer: a common pathogenetic role of the β-adrenergic system. Med Res Rev 2015;35:619–52.
File RR, Patton TF. Topically applied pilocarpine. Human pupillary response as a function of drop size. Arch Ophthalmol 1980;98:112–5.
Elibol O, Alçelik T, Yüksel N, Caglar Y. The influence of drop size of cyclopentolate, phenylephrine and tropicamide on pupil dilatation and systemic side effects in infants. Acta Ophthalmol Scand 1997;75:178–80.
Kumar S, Karki R, Meena M, Prakash T, Rajeswari T, Goli D. Reduction in drop size of ophthalmic topical drop preparations and the impact of treatment. J Adv Pharm Technol Res 2011;2:192–4.
Shell JW. Pharmacokinetics of topically applied ophthalmic drugs. Surv Ophthalmol 1982;26:207–18.
Dal Monte M, Filippi L, Bagnoli P. Beta3-adrenergic receptors modulate vascular endothelial growth factor release in response to hypoxia through the nitric oxide pathway in mouse retinal explants. Naunyn Schmiedebergs Arch Pharmacol 2013;386:269–78.
Good WV, Hardy RJ, Wallace DK, et al. β-Blocking and racial variation in the severity of retinopathy of prematurity. Arch Ophthalmol 2012;130:117–8.
Acknowledgements
We are most grateful to the nursing staff of the Neonatal Intensive Care Units of the A. Meyer University Children’s Hospital, Florence, the University Hospital of Siena, and the Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, University of Milan, Italy, for their assistance in conducting this study. Trial Registration: Current Controlled Trials ISRCTN68126628; ClinicalTrials.gov Identifier NCT02014454; EudraCT Number 2013-002062-39.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Figures S1
(TIFF 2015 kb)
Supplementary Figures S2
(TIFF 1675 kb)
Supplementary Table S1
(DOC 52 kb)
Rights and permissions
About this article
Cite this article
Filippi, L., Cavallaro, G., Bagnoli, P. et al. Propranolol 0.1% eye micro-drops in newborns with retinopathy of prematurity: a pilot clinical trial. Pediatr Res 81, 307–314 (2017). https://doi.org/10.1038/pr.2016.230
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.230
This article is cited by
-
The efficacy and safety of inositol supplementation in preterm infants to prevent retinopathy of prematurity: a systematic review and meta-analysis
BMC Ophthalmology (2019)
-
Oral propranolol in prevention of severe retinopathy of prematurity: a systematic review and meta-analysis
Journal of Perinatology (2019)
-
Study protocol: safety and efficacy of propranolol 0.2% eye drops in newborns with a precocious stage of retinopathy of prematurity (DROP-ROP-0.2%): a multicenter, open-label, single arm, phase II trial
BMC Pediatrics (2017)