Abstract
Background:
Childhood infections are common and Bacillus Calmette-Guérin (BCG) vaccination at birth may prevent these via nonspecific effects.
Methods:
A randomized, clinical multicenter trial. All women planning to give birth (n = 16,521) at the three study sites were invited during the recruitment period. Participating children were randomized to receive BCG within 7 d of birth or to a no intervention control group. Parent-reported infections (events) were collected using telephone interviews at 3 and 13 mo. Data collectors were blinded to allocation.
Results:
The analyses included 4,224/4,262 (99%) and 4,192/4,262 (98%) children at 3 and 13 mo. From 0 to 3 mo, there were 291 events in the BCG group vs. 336 events in the control group, incidence rate ratio (IRR) = 0.87 (95% confidence interval (CI): 0.72 to 1.05). In this age group, the IRR was 0.62 (95% CI: 0.39 to 0.98) if the mother was BCG vaccinated. From 3 to 13 mo, there were 7,028 vs. 6,791 events, IRR = 1.02 (95% CI: 0.97 to 1.07).
Conclusion:
This study did not find a nonspecific public health benefit of BCG on parent-reported infections. BCG may have reduced the incidence of infections in children of BCG-vaccinated mothers during the first 3 mo.
Similar content being viewed by others
Main
The Bacillus Calmette-Guérin (BCG) vaccine is used to protect against tuberculosis and is one of the most widely used vaccines in the world. WHO recommends BCG as part of the childhood vaccination program if tuberculosis is prevalent (1). There is mounting clinical evidence that BCG has a positive nonspecific effect on nontuberculous mortality (2,3,4,5,6) and infectious diseases (7) in low-income countries, as well as an ecological study pointing to a positive effect on hospitalizations in a high-income country (8), resulting in a public health benefit that may extend beyond protection against tuberculosis. Several immunological mechanisms that might explain these effects have been proposed (9,10,11). It has not previously been examined in a randomized trial whether BCG has public health benefits on nontuberculous infectious disease in high-income countries. BCG is not part of the childhood vaccination program in Denmark. Therefore, it was possible to conduct The Danish Calmette Study—a randomized, clinical trial designed to examine whether BCG at birth could reduce the number of all-cause hospitalizations from birth to age 15 mo (12).
The present study reports on a prespecified secondary outcome of The Danish Calmette Study. The purpose was to examine if BCG at birth can reduce the incidence of parent-reported infectious diseases in the first year of life.
Results
Between October 2012 and November 2013, we enrolled and randomized 4,262 children, 2,129 to receive BCG and 2,133 to the control group. Randomization baseline characteristics have been presented elsewhere (13). Baseline characteristics were distributed evenly except non-Danish ethnicity and paternal smoking during pregnancy, both of which were more frequent in the control group. First follow-up was 99% (4,224/4,262) complete and second follow-up was 98% (4,192/4,262) complete. Table 1 summarizes follow-up characteristics. There were 627 infectious illness episodes and 2,173 GP visits from birth to first follow-up at 3 mo of age and 13,819 infectious illness episodes and 10,563 GP visits from first to second follow-up at 13 mo of age. Hence, the distribution of disease episodes and GP visits was significantly different in the first and the second period. In the youngest age group, there were 3.5 times more GP visits than episodes of infectious illness reported by the parents (2,173/627). In contrast, between 3 and 13 mo of age, there were 31% more infectious illness episodes than GP visits reported (13,819/10,563) (χ2 = 1,200, P < 0.001).
The exposure time was 11,151 mo from birth to first follow-up and 40,802 mo from first to second follow-up in the entire cohort. Significantly, more parents (46.3% = 973/2,102) in the BCG-group than in the control group (39.6% = 822/2074) had used a diary to aid memory of episodes of illness (χ2 = 19.36, P < 0.001), but there was no statistically significant difference in the number of events reported by users of a diary compared to nonusers (IRR: 0.95, 95% confidence interval (CI): 0.91 to 1.01, P = 0.08). There were fewer visits to the GP reported by users of a diary compared to nonusers (IRR 0.90, 95% CI: 0.85 to 0.95, P = 0.001).
Main Outcomes
There was no statistically significant difference in the number of infectious illnesses from birth to 3 mo or from 3 to 13 mo ( Table 2 ). The effect did not differ significantly between first and second follow-up (test for no interaction; P = 0.09).
Secondary Outcomes and Subgroups
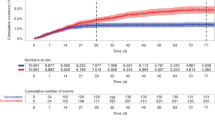
Comparing children randomized to BCG with control children, there was a difference in the number of visits to the GP at first follow-up at 3 mo of age, the IRR being 0.88 (95% CI: 0.79 to 0.98), but not at the second follow-up at 13 mo of age (IRR = 1.03, 95% CI: 0.97 to 1.09). Hence, the effect of BCG differed significantly between the two age groups (test for no interaction: P = 0.01). There was no statistically significant effect of BCG on the number of episodes in the different infectious disease categories ( Table 3 ). There were no differences in the BCG effect between premature and mature children or between boys and girls ( Figure 1 and Supplementary Table S1 online). In the analysis stratified by maternal BCG status, BCG was associated with reduced number of infectious illness episodes from 0 to 3 mo if the mother was BCG vaccinated, IRR = 0.62 (95% CI: 0.39 to 0.98), corresponding to a number needed to vaccinate of 14, but the effect was not seen at 13-mo follow-up (test for no interaction: P = 0.03) ( Figure 1 and Supplementary Table S1 online).
Effect of neonatal BCG on parent-reported infections and visits to the general practitioner from birth to 13 mo in subgroups. (a) Effect of neonatal BCG by prematurity. (b) Effect of neonatal BCG by child sex. (c) Effect of neonatal BCG by maternal BCG vaccination status. ▴: All, •: Term children (GA ≥ 37 wk), ▪: Premature children (GA < 37 wk), ○: Boys, □: Girls, х: Maternal BCG vaccination, ♦: No maternal BCG vaccination. BCG, Bacille Calmette-Guérin vaccine; GA, gestational age; GP, general Practitioner; IRR, incidence rate ratio.
Sensitivity Analyses
Sensitivity analyses excluding those children that were followed-up later than specified in the standard operating procedure at first and second follow-up, those that did not follow the allocation (per-protocol analysis) and those that received DTaP-IPV-Hib prior to first follow-up did not change the estimates significantly. Statistical analyses that accounted for twins (n = 152 children) and triplets (n = 3 children) did not change the estimates. Adjustment for the use of infectious illness-diary did not change the estimates (Supplementary Table S2 online), nor did a post-hoc analysis restricted to children where the parents had used an infectious disease diary (data not shown).
Discussion
BCG given at birth does not seem to reduce the number of parent reported episodes of infectious illness from birth to 13 mo of age in a high-income country. Consistent with what has been seen for hospital admissions among the children participating in the Danish Calmette Study where we observed a protective effect of BCG on hospitalization for infection from birth to 15 mo if the mother was BCG vaccinated too, a stratified analysis revealed an effect from 0 to 3 mo if the mother of the child was BCG vaccinated (IRR = 0.62).
This randomized trial is large, with almost complete follow-up and enough events to detect an effect on the primary outcome. Data collection in this study covered a subset of the most common childhood infectious diseases and some diseases were narrowly defined (such as diarrhea only being recorded if there was coincident loose stools and vomiting) and the investigators were blinded during data collection.
Our study has limitations, a major one being that parents could not be blinded. Some parents were disappointed when they were randomized to the control group (14). Therefore, we suspect lower attachment to the study data collection in this group, possibly resulting in under-reporting of events, thus attenuating the positive effect of BCG seen at first follow-up. However, adjusting the analysis for use of a diary did not modify the results (Supplementary Table S2 online). Furthermore, we asked the parents for number of episodes and thus we cannot establish whether BCG has an effect on the length of individual episodes. We observed a high incidence of visits to the GP compared to the actual number of reported infectious illness episodes, particularly so at the first follow-up. This may be explained by our choice of diseases and definitions of these possibly combined with a low threshold for parents of newborns to consult a GP in a country where health care is supplied free of charge and is readily available. Thus, visits to the GP may reflect parental concern and easy access more than severity of illness and actual need for treatment. However, the two measures of morbidity—infectious disease episodes and GP visits—gave essentially identical estimates for the effect of BCG in both age groups.
The Danish Calmette Study is the first major trial studying nonspecific effects of BCG in a high-income country. Previously, in Guinea-Bissau, BCG has been shown to have a positive nonspecific effect most pronounced during the first months after vaccination in low-birth-weight children (2), and it has also been shown that nonspecific effects of vaccines can be modulated by subsequent vaccines (2,15). Several clinical studies have suggested a transgenerational effect of maternal exposure to BCG or Mycobacterium tuberculosis that modulates the immune response to BCG in the newborn (16,17). In Guinea-Bissau, where the positive nonspecific effect of BCG has been most consistently found (2,3,4,5,6), BCG has been part of the childhood vaccination program for decades, thus most of the mothers in those studies would be BCG vaccinated or exposed to mycobacteria.
This study did not find a decreased risk of infectious illness in the first year of life among BCG-vaccinated children, but we did find a 38% reduction in the number of infectious illnesses up to 3 mo of age if the mother had received BCG ( Figure 1 and Supplementary Table S1 online), corresponding to a number needed to treat of 14. This is consistent with the another secondary outcome of The Danish Calmette Study, where fewer hospitalizations for infection were found if the mother was BCG vaccinated (13). If maternal BCG vaccination is a prerequisite for a nonspecific effect of BCG, a possible explanation for the lack of overall effect in this study could be that only 17.7% (740/4,184) of the mothers were BCG vaccinated.
This study does not support using BCG to prevent infectious illnesses in a high-income setting, even though our data indicates that there could be a positive effect if the mothers are covered by BCG. The beneficial effect disappeared after 3 mo of follow-up, possibly being offset by the vaccines given at age 3 mo and onwards. Hence, the present study may support previous studies in indicating that the sequence of vaccines is important for morbidity patterns (2,15,18). In the present trial, BCG was administered alone versus no vaccine. A randomized trial in Guinea-Bissau documented that oral polio vaccine coadministered with BCG versus BCG only had an additional beneficial nonspecific effect on infant survival (19), suggesting that the addition of other vaccines may affect the overall effect of BCG. Observational studies have also suggested that coadministration of BCG and inactivated diphtheria-tetanus-pertussis vaccine had marked beneficial nonspecific effects compared to receiving inactivated diphtheria-tetanus-pertussis vaccine after BCG (20,21). Hence, the present study may not predict what would happen in a high-income setting where another vaccine, e.g., hepatitis B vaccine, was also administered at birth.
Thus, in line with previous research on materno-fetal immunity to mycobacteria (16,17), The Danish Calmette Study indicates a positive nonspecific effect of BCG in infancy on number of infectious disease episodes and hospitalizations for infectious diseases among children whose mother was also BCG-vaccinated. It would be interesting to pursue if the nonspecific effect described in low-income settings is dependent on the BCG vaccination status of the mother and whether previous exposure to tuberculosis may similarly provide priming which enhances the benefit of BCG for the offspring. In any event, these observations, as well as previous observations on the benefit of being measles vaccinated in the presence of maternal antibodies (22), suggest that maternal immunity may influence the child’s response to vaccines. This could mean that maternal immunity has a larger role in priming the immune system of the newborns than has been previously recognized.
Conclusion
This study found no overall beneficial impact of BCG vaccination on morbidity up to 13 mo of age. Hence, there is no support for the use of BCG to reduce the burden of infectious diseases in high-income settings in which the mothers have not had BCG themselves.
Methods
The methods of The Danish Calmette Study are described in detail elsewhere (12). In brief, pregnant women planning to give birth at three Danish university hospitals from October 2012 to November 2013 received a letter in the second or third trimester with an invitation to participate in the study. Study staff telephoned the women to answer potential questions about the study and conduct a baseline interview with those who wished to participate. Within 7 d of birth, study staff randomized children to receive BCG (SSI Danish strain 1,331) at the standard dose of 0.05 ml intradermally on the left shoulder or to a no-intervention control group. Parents were not blinded to allocation since the local inflammatory reaction caused by BCG vaccination could not be mimicked. Randomization was stratified by prematurity (gestational age (GA) < or ≥ 37 wk) and children were allocated 1:1 in permuting blocks of 2-4-6 using an online system. Exclusion criteria were GA < 32 wk, birth weight < 1,000 g, critically ill child, no Danish-speaking parent, known immune deficiency, or maternal use of immune modulating drugs during pregnancy.
Follow-up for This Study
Following randomization, parents were asked to take notes of their child’s illness and were given a diary for this purpose. Follow-up at age 3 and 13 mo was chosen because previous studies have indicated that the nonspecific effects of BCG is altered by other vaccines (20). In Denmark, the first vaccines in the childhood vaccination program are diphtheria, tetanus, acellular pertussis, polio, Haemophilus influenzae type b (DTaP-IPV-Hib), and Streptococcus pneumonia conjugate (PCV) vaccine. The two vaccines are given at 3, 5, and 12 mo. Therefore, follow-up consisted of a period from birth to 3 mo of age in which the only vaccine given was BCG and a period from 3 to 13 mo where the children followed the vaccination program. Follow-up consisted of a structured telephone interview. Parents were asked at the beginning of the interview not to disclose if the child had received BCG to keep study staff blinded during data collection. At 3-mo follow-up, study staff asked parents the following questions: “How many visits have you had at your family doctor or at a doctor on call (collectively termed general practitioner (GP)) with your child due to suspected infectious illness?”, “How many episodes of the common cold has your child had?” (only episodes where the parents suspected fever were recorded), “How many pneumonias has your child had?” (only pneumonias that were diagnosed by a doctor were recorded), “How many episodes of fever with no apparent cause has your child had?” (only episodes with a temperature > 38 °C were recorded), “How many episodes of diarrhea has your child had?” (only episodes with coincident loose stools and vomiting were recorded), “How many episodes of acute otitis media has your child had?” (only episodes with pus flowing from the ear were recorded). At the 13-mo follow-up, the same questions were asked, adding “since the last interview” and a supplementary question was asked: “Have you taken notes of your child’s illness to aid your memory?”
The number of individual infectious illness episodes was summed as the total number of infectious illness episodes at 3 and 13 mo. BCG vaccination status of the mother was self-reported at the baseline interview.
Outcomes
The primary outcome of the present study was total number of infectious illness episodes from 0 to 3 mo and from 3 to 13 mo. Secondary outcomes were number of visits to the GP and number of episodes of each type of infectious diseases. Subgroup analyses of child sex and prematurity were planned because previous studies have suggested differential effects of BCG in these groups (2,22). We also prespecified a subgroup analysis of maternal BCG vaccination status due to a previous study concluding that nonspecific effects of the measles vaccine are more pronounced when given in the presence of maternal antibodies (23). All outcomes and analyses were prespecified in analysis plans, which were deposited with the data and safety monitoring board prior to unblinding of the data, except if otherwise stated.
Sample Size, Data Management, and Statistics
Sample size was determined by the primary outcome of The Danish Calmette Study—number of all-cause hospitalizations. With 3,972 children, a 20% reduction in all-cause hospitalization by 15 mo of age could be found with a power of 90% and a significance level of 0.05. We aimed to include 4,300 children. A large study of children’s health in Denmark showed that 18.5% of infants in Denmark have had an episode of infectious illness within the previous 14 d and 7.3% of parents have contacted their GP concerning their infant within the previous 14 d (24). Based on these figures, this study would be able to detect an incidence rate ratio (IRR) of 0.78 for parent-reported infectious illnesses with a power of 94% and an IRR of 0.68 for contacts to the GP with a power of 88% with a sample size of 4,300.
The standard operating procedure for the follow-up stated that it should be conducted between age 2 and 4 mo for the 3-mo follow-up and prior to 14 mo for the 13-mo follow-up. For children followed-up after the specified time slots, only episodes of illness that occurred up to the age of 4 mo (123 d) and up to the age of 14 mo (428 d) were recorded. In sensitivity analyses, children were excluded if follow-up did not take place within the timeframe specified, as were children who had received a DTaP-IPV-Hib and PCV vaccine prior to the 3-mo follow-up. Data were entered directly into an electronic case report form.
Secondary outcomes of the present study were subject to Holland correction (25), using the number of secondary outcome analyses as correction number. The number of infectious illnesses was analyzed using negative binomial regression. The number of months at risk from birth to first follow-up and from first to second follow-up was used as exposure time; results are presented as incidence rate ratios (IRR) with 95% CI. Number needed to treat was calculated as 1 divided by the absolute risk difference at follow-up. Ordered, non-normally distributed data were analyzed using Mann-Whitney U test and categorical data were analyzed using χ2. All analyses were performed using STATA 13.1 (StataCorp, College Station, TX).
Ethics
The Calmette Study was approved by the Committees on Biomedical Research Ethics (J.no. H-3-2010-087), the Danish Data Protection Board (J.no. 2009-41-4141), and the Danish Medicines Agency (J.no. 2612–4356. EudraCT 2010-021979-85. Protocol 2009–323) and was registered at www.clinicaltrials.gov with trial registration number NCT01694108. The trial was supervised by the Good Clinical Practice Units of the Capital Region and the Region of Southern Denmark. The study was monitored by an independent data and safety monitoring board. All parents gave written informed consent prior to randomization.
Statement of Financial Support
This work was supported by Copenhagen University Hospital Rigshospitalet; Copenhagen University Hospital Hvidovre; Lillebaelt Hospital – Kolding Sygehus and by the Danish National Research Foundation (DNRF108). J.K. received grants from Rigshospitalets Forskningsfond; Dagmar Marshall fonden; Else og Mogens Wedell Wedellsborgs fond and Christian Larsen og Dommer Ellen Larsens Fond. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Disclosure
None of the authors have any financial ties to the products used in this study. Vaccines were manufactured by Statens Serum Institute but were bought at regular market price for the study. Statens Serum Institute had no role in funding, conducting, or reporting the study.
References
World Health Organization. Position paper: BCG Vaccine. Wkly Epidemiol Rec 2004;79:27–48.
Aaby P, Roth A, Ravn H, et al. Randomized trial of BCG vaccination at birth to low-birth-weight children: beneficial nonspecific effects in the neonatal period? J Infect Dis 2011;204:245–52.
Roth A, Gustafson P, Nhaga A, et al. BCG vaccination scar associated with better childhood survival in Guinea-Bissau. Int J Epidemiol 2005;34:540–7.
Roth A, Sodemann M, Jensen H, et al. Tuberculin reaction, BCG scar, and lower female mortality. Epidemiology 2006;17:562–8.
Storgaard L, Rodrigues A, Martins C, et al. Development of BCG scar and subsequent morbidity and mortality in rural Guinea-Bissau. Clin Infect Dis 2015;61:950–9.
Kristensen I, Aaby P, Jensen H. Routine vaccinations and child survival: follow up study in Guinea-Bissau, West Africa. BMJ 2000;321:1435–8.
Stensballe LG, Nante E, Jensen IP, et al. Acute lower respiratory tract infections and respiratory syncytial virus in infants in Guinea-Bissau: a beneficial effect of BCG vaccination for girls community based case-control study. Vaccine 2005;23:1251–7.
de Castro MJ, Pardo-Seco J, Martinón-Torres F. Nonspecific (Heterologous) protection of neonatal BCG vaccination against hospitalization due to respiratory infection and sepsis. Clin Infect Dis 2015;60:1611–9.
Jensen KJ, Larsen N, Biering-Sørensen S, et al. Heterologous immunological effects of early BCG vaccination in low-birth-weight infants in Guinea-Bissau: a randomized-controlled trial. J Infect Dis 2015;211:956–67.
Kleinnijenhuis J, Quintin J, Preijers F, et al. Bacille Calmette-Guerin induces NOD2-dependent nonspecific protection from reinfection via epigenetic reprogramming of monocytes. Proc Natl Acad Sci USA 2012;109:17537–42.
Netea MG, Quintin J, van der Meer JW. Trained immunity: a memory for innate host defense. Cell Host Microbe 2011;9:355–61.
Thøstesen LM, Nissen TN, Kjærgaard J, et al. Bacillus Calmette-Guérin immunisation at birth and morbidity among Danish children: a prospective, randomised, clinical trial. Contemp Clin Trials 2015;42:213–8.
Stensballe LG, Sørup S, Aaby P, et al. BCG vaccination at birth and early childhood hospitalisation: a randomised clinical multicentre trial. Arch Dis Child 2016. DOI: 10.1136/archdischild-2016-310760 .
Meinich Petersen S, Zoffmann V, Kjærgaard J, Graff Stensballe L, Graff Steensballe L, Greisen G. Disappointment and adherence among parents of newborns allocated to the control group: a qualitative study of a randomized clinical trial. Trials 2014;15:126.
Aaby P, Jensen H, Samb B, et al. Differences in female-male mortality after high-titre measles vaccine and association with subsequent vaccination with diphtheria-tetanus-pertussis and inactivated poliovirus: reanalysis of West African studies. Lancet 2003;361:2183–8.
Mawa PA, Nkurunungi G, Egesa M, et al. The impact of maternal infection with Mycobacterium tuberculosis on the infant response to bacille Calmette-Guérin immunization. Philos Trans R Soc Lond B Biol Sci 2015;370:.
Elliott AM, Mawa PA, Webb EL, et al. Effects of maternal and infant co-infections, and of maternal immunisation, on the infant response to BCG and tetanus immunisation. Vaccine 2010;29:247–55.
Sørup S, Benn CS, Poulsen A, Krause TG, Aaby P, Ravn H. Live vaccine against measles, mumps, and rubella and the risk of hospital admissions for nontargeted infections. JAMA 2014;311:826–35.
Lund N, Andersen A, Hansen AS, et al. The effect of oral polio vaccine at birth on infant mortality: a randomized trial. Clin Infect Dis 2015;61:1504–11.
Aaby P, Ravn H, Roth A, et al. Early diphtheria-tetanus-pertussis vaccination associated with higher female mortality and no difference in male mortality in a cohort of low birthweight children: an observational study within a randomised trial. Arch Dis Child 2012;97:685–91.
Aaby P, Nielsen J, Benn CS, Trape JF. Sex-differential and non-specific effects of routine vaccinations in a rural area with low vaccination coverage: an observational study from Senegal. Trans R Soc Trop Med Hyg 2015;109:77–84.
Aaby P, Vessari H, Nielsen J, et al. Sex differential effects of routine immunizations and childhood survival in rural Malawi. Pediatr Infect Dis J 2006;25:721–7.
Aaby P, Martins CL, Garly ML, et al. Measles vaccination in the presence or absence of maternal measles antibody: impact on child survival. Clin Infect Dis 2014;59:484–92.
The Danish National Institute of Public Health. Danske børns sundhed og sygelighed, 2009. (http://www.si-folkesundhed.dk/upload/web_susy_b%C3%B8rn.pdf).
Newson RB. Frequentist q-values for multiple-test procedures. Stata J 2010;10:568–84.
Acknowledgements
We would like to thank all the study staff at the three study sites and the participating families in particular.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Tables
(DOC 81 kb)
PowerPoint slides
Rights and permissions
About this article
Cite this article
Kjærgaard, J., Birk, N., Nissen, T. et al. Nonspecific effect of BCG vaccination at birth on early childhood infections: a randomized, clinical multicenter trial. Pediatr Res 80, 681–685 (2016). https://doi.org/10.1038/pr.2016.142
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.142
This article is cited by
-
A systematic review of BCG vaccination policies among high-risk groups in low TB-burden countries: implications for vaccination strategy in Canadian indigenous communities
BMC Public Health (2019)
-
Bacillus Calmette-Guérin vaccination at birth and in vitro cytokine responses to non-specific stimulation. A randomized clinical trial
European Journal of Clinical Microbiology & Infectious Diseases (2018)
-
Bacillus Calmette-Guérin vaccination, thymic size, and thymic output in healthy newborns
Pediatric Research (2017)
-
Effects of Bacillus Calmette-Guérin (BCG) vaccination at birth on T and B lymphocyte subsets: Results from a clinical randomized trial
Scientific Reports (2017)