Abstract
Background:
Limited studies have evaluated the risk factors for congenital heart defects (CHDs) in China and compared them for different types of CHDs. This study examined risk factors between isolated and multiple CHDs as well as among CHDs subtypes in Guangdong, Southern China.
Methods:
This population-based case–control study included 4,034 pairs of case and control infants enrolled in the Guangdong Registry of CHD study, 2004–2013. Multivariate logistic regression was used to compute adjusted odds ratios (ORs) while simultaneously controlling for confounders.
Results:
Multiple maternal environmental exposures, including living in newly renovated rooms, residential proximity to main traffic, paternal smoking, and maternal occupation as manual worker, were significantly associated with CHDs with ORs ranging 1.30–9.43. Maternal perinatal diseases (including maternal fever, diabetes, influenza, and threatened abortion), maternal medication use (antibiotic use), advanced maternal age, low socioeconomic status, and paternal alcohol intake were also significantly associated with CHDs, with ORs ranging 1.60–3.96. Isolated CHDs and multiple defects have different profiles of risk factors, while subtype of CHD shares common risk factors.
Conclusion:
These results suggest that maternal environmental exposures/occupation and perinatal diseases/medication use were dominant risk factors associated with CHDs in Southern China. Isolated and multiple CHDs may have different etiologic factors.
Similar content being viewed by others
Introduction
Congenital heart defects (CHDs) are one of the most common abnormalities, with an estimated incidence of 6–12 per 1,000 live births globally. This defect remains the leading cause of birth defect-associated morbidity, mortality, and disability. It greatly impairs the life quality of sufferers and involves huge medical expenditures for the family and society (1). Therefore, it is important to better understand the etiological factors for these malformations, especially the modifiable ones, which may be a crucial step leading to optimal strategies for prevention.
Over the past decade, there have been major breakthroughs in the understanding of inherited causes of congenital heart disease, including the identification of specific genetic abnormalities for some types of malformations (2). Additionally, a growing body of epidemiological literature has shown that a multitude of noninherited modifiable risk factors were associated with an increased risk of CHDs, including maternal illnesses, maternal therapeutic and nontherapeutic drug exposures, environmental exposures, and paternal exposures (1). Some known risk factors include maternal rubella; phenylketonuria; pregestational diabetes; exposure to thalidomide, vitamin A congeners, or retinoids; and indomethacin tocolysis (1). On the other hand, periconceptional multivitamin or folic acid intake may reduce the risk of CHDs in the fetus (1).
However, large and comprehensive studies of CHDs were lacking in China. Due to the rapid industry and economic growth in Guangdong, China during the past few decades, living standards, physical environments, and lifestyles have undergone significant changes, which may lead to the emergence of novel risk factors for CHDs in this population. On the other hand, CHDs as a general category are heterogeneous and can be highly complex. Different risk factors may apply to isolated or multiple defects. Because a specific exposure is not expected to increase the risk for CHD in general, it is therefore important to create homogeneous groups (3), but few studies have assessed risk factors for these different groups of CHDs.
To address the research gaps using the data from the Guangdong Registry of Congenital Heart Disease (GRCHD) during the years 2004–2013, we assessed the risk factor spectrum of CHD subtypes in Guangdong, China. To the best extent possible, we differentiated CHD groups into isolated CHD and multiple defects, and specific subtype, to explore and compare the risk factors in these different homogeneous groups. Through these efforts, we aimed to better understanding the etiology for CHDs in Guangdong, China.
Results
From the original study population of 6,999 cases, which were included in GRCHD during 1 January 2004–31 December 2013, we excluded 45 cases with syndromes caused by gene mutations or chromosomal aberration as the current study focused on modifiable factors. We also excluded 45 nonsingleton cases (because nonsingletons tend to have more birth defects), 662 cases prenatally diagnosed with atrial septal defect (ASD, likely to disappear postnatally), and 369 preterm infants with patent ductus arteriosus (because preterm infants tend to have more patent ductus arteriosus) and 1,844 cases without matched controls. The final analysis included 4,034 cases and their corresponding 4,034 controls.
Among the eligible cases, a total of 3,856 isolated CHDs (96%) with only cardiac defect (3) and 178 multiple defects (4%) consisting of cardiac defects and extracardiac defects were identified. Distribution of maternal age and infant birth weight were significantly different between cases and controls ( Table 1 ). Among all the eligible cases, 9.5% were diagnosed prenatally at a median time of 27 gestational week, while 87.2% were diagnosed postnatally at a median of 5 d after birth. Interviews were conducted within 1 y after birth, with a median of 22 and 32 d in cases and controls, respectively ( Table 1 ). The participation rate is 76% for cases and 60% for controls.
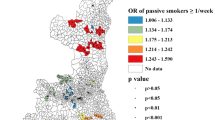
In Table 2 , multivariate analysis showed that maternal fever and paternal alcohol intake were risk factors for both isolated CHDs and multiple defects, with the odds ratios (ORs) much higher for multiple defects than for isolated CHDs. Other factors including maternal education less than high school level, previous pregnancies with still birth, living in newly renovated rooms, residential proximity to main traffic, maternal occupation as manual worker, and maternal diabetes also tended to be associated with these two types of defects, although they were not statistically significant for multiple defects due to small sample size. Advanced maternal age, low household income, chemical contact, paternal smoking, maternal occupation as service industry/housekeeper, influenza, threatened abortion, and antibiotics were specifically associated with isolated CHDs. Meanwhile, passive smoking was specifically associated with multiple defects. Among six environmental factors included in the regression model, five of them (chemical contact, paternal smoking, newly renovated rooms, residential proximity to traffic, and maternal occupation as manual worker/service industry/housekeeper) were statistically associated with isolated CHDs with ORs ranging from 1.30 to 9.43. Passive smoking was statistically associated with multiple defects with an OR of 7.95 (95% confidence interval (CI): 1.03, 61.39), while three other environmental factors (newly renovated rooms, proximity to main traffic, and maternal occupation as manual worker/scientist and technician) showed elevated ORs of multiple defects ranging from 1.71 to 6.18 but were not statistically significant due to very small sample size. Multiple maternal perinatal diseases and medication use were also associated with isolated CHDs (including factors of maternal fever, diabetes, influenza, threatened abortion, and antibiotic use) and multiple defects (including maternal fever), with ORs ranging from 1.60 to 3.96 in isolated CHDs, and being 46.88 in multiple defects.
We also examined whether multiple factors of maternal environmental exposure and perinatal diseases/medication showed a dose–response effect on the occurrence of isolated CHDs. As shown in Figure 1a , and for the five significant environmental factors associated with isolated CHDs (chemical contact, paternal smoking, living in newly renovated rooms, residential proximity to main traffic <50 m, and maternal occupation as manual worker), maternal exposure to any one of these factors tended to increase the risk of isolated heart defects with an average OR of 1.97 (95% CI: 1.68, 2.32), while exposure to two or more of these factors showed an average OR of 4.87 (95% CI: 3.59, 6.62). Trend test showing a dose–response effect is significant, i.e., the higher number of maternal environmental exposure, the higher risk of isolated CHDs. In Figure 1 b, for the five perinatal diseases/medication use factors that had statistically significant association with isolated CHDs (maternal fever, diabetes, influenza, threatened abortion, and antibiotic use), exposure to any one of these five factors increased the risk of isolated heart defects with an average OR of 2.64 (95% CI: 2.07, 3.36), while exposure to two or more factors increased risk with an average OR of 2.72 (95% CI: 1.66, 4.45). However, no significant dose–response association was detected between the number of perinatal diseases/medication use factors and the risk of isolated CHDs.
Association between the number of maternal exposure factors and the risk of isolated CHDs, Guangdong, China, 2004–2013. (a) Maternal environmental risk factors: chemical contact, paternal smoking, living in newly renovated rooms, residential proximity to main traffic <50 m, maternal occupation as manual worker. The association between the number of total environmental factors and isolated CHDs was assessed using multivariate analysis while simultaneously controlling for the other confounders. *OR is statistically significant compared to “0” exposure group; †OR is statistically significant compared to “1” exposure group. (b) Maternal diseases/medication use: maternal fever, diabetes, influenza, threatened abortion, and antibiotic use. The association between the number of maternal diseases/medication use and isolated CHDs was assessed using multivariate analysis while simultaneously controlling for the other confounders. *OR is statistically significant compared to “0” exposure factor. CHD, congenital heart defect; OR, odds ratio.
We further looked into the risk factors for CHDs by subtypes ( Table 3 ). Maternal chemical contact is the strongest risk factor for ventricular septal defect (VSD; OR: 11.71, 95% CI: 4.01, 34.24), ASD (OR: 9.98, 95% CI: 1.15, 86.81), and congenital pulmonary stenosis (OR: 18.01, P > 0.05). Other top risk factors significantly associated with VSD were antibiotic use (OR: 3.39, 95% CI: 1.23, 9.36), maternal fever (OR: 2.94, 95% CI: 1.36, 6.35), previous pregnancies with still birth (OR: 2.90, 95% CI: 1.98, 4.25), and living in newly renovated rooms (OR: 2.85, 95% CI: 1.41, 5.77). While many similar risk factors of VSD were found for ASD as well, the top five risk factors for ASD include chemical contact (OR: 9.98, 95% CI: 1.15, 86.81), diabetes (OR: 6.18, 95% CI: 1.82, 20.95), newly renovated rooms (OR: 4.64, 95% CI: 1.30, 16.60), paternal alcohol intake (OR: 3.39, 95% CI: 1.96, 5.84), and residential proximity to traffic <50 m (OR: 3.29, 95% CI: 2.01, 5.38). Pulmonary stenosis was significantly associated with maternal occupation as manual worker (OR: 6.58, 95% CI: 1.35, 32.07), household income <1,000 (OR: 5.51, 95% CI: 1.50, 20.21), proximity to heavy traffic (OR: 3.95, 95% CI: 1.00, 15.81), still birth history (OR: 3.89, 95% CI: 1.02–14.81), and less than high school education (OR: 3.46, 95% CI: 1.44, 8.29). Congenital transposition of great artery were significantly associated with paternal smoking, living in newly renovated rooms, residential proximity to main traffic, and threatened abortion with very wide CI due to low exposure cases.
Discussion
In the current study, we found that environmental exposures are the most important risk factors that were associated with all types of CHDs. Additionally, we found a significant dose–response effect, i.e., the higher number of maternal environmental exposures, the higher risk of isolated CHDs. Among the environmental factors assessed, all of them were significantly associated with two to three subtypes of CHDs and traffic exposure was significantly associated with all four subtypes of CHDs. Contacting with harmful chemicals including organic solvents and pesticides had the highest risk for CHDs with almost 9–11-folds of risk increase for different types of CHDs. This finding is consistent with previous compelling evidence on the associations between maternal exposure to organic solvents and cardiac defects (4,5,6). Specifically, the US National Birth Defects Prevention Study (NBDPS) found positive associations between occupational exposure to solvents and several types of simple isolated CHDs (5), and the Baltimore-Washington Infant Study documented maternal reports of potential exposure to pesticides being associated with CHDs (7). These studies revealed ORs ranging from 1.5 to 2.1 for exposures to chemicals such as solvent, dyes, pigments, and insecticides. Our study showed a greater magnitude of risk for harmful chemical contact, which may be attributed to higher environmental exposures in China than in the United States, different classification of CHDs or chemical exposures, or different populations from the previous studies. As Guangdong is a rapidly developing industrial province in China, various industrials including printing houses, shoe factories, electronics manufacturing, chemical plants, dyes and dyeing factories, tannery, etc. are pollution sources in Guangdong, especially the Pearl River Delta region. Mothers lived in this region may have more occupational or nonoccupational exposures to harmful chemicals than those in the United States.
Living in newly renovated rooms was also a strong risk factor in this study for all subtypes of CHD, with the ORs ranging from 2.85 to 22.70 borderline with large 95%. Our finding supported another report by Liu et al. (8) in China that demonstrated a significant association between maternal exposure to housing renovations with CHD in offspring (OR: 1.89, 95% CI: 1.29, 2.77), and there were similar risks for cardiac defects with or without extracardiac malformations (OR of 2.65 and 1.76, respectively). Our study displayed much higher ORs for all kinds of CHDs than those in the other study. The difference may stem from the different regions covered. The previous study recruited participants from four tertiary maternal and child hospitals (Guangdong, Fujian, Henan, and Hubei provinces) in China, while our study concentrated on Guangdong Province and has a much larger sample that could provide reliable evidence. In addition, Liu et al. (8) defined living in newly renovated rooms as the pregnant woman moving into a new house within 1 mo after decoration, while our study defined it within 6 mo after decoration. The increased risks for CHD occurrence from exposure to renovation activity may be due to the harmful substances being released from the decoration materials like benzene, trichloroethylene, formaldehyde, etc., which were reported to increase the prevalence of CHD in offspring of exposed mothers (8,9,10). Another consideration is that renovated house may be a marker for socioeconomic status (SES), because low SES family tended to use cheap and nonenvironment-friendly decoration materials, and they may not be well educated to know the hazards of renovated materials.
Our study also found that proximity to main traffic was a potential risk factor for isolated CHDs, VSD, ASD, pulmonary stenosis, and transposition of great artery. Prior studies in this area are very limited, and proximity to main traffic is a marker of exposure to air pollution (11). Our study appears to support two recent studies, conducted in southern California and in seven Texas counties, respectively, that reported possible effect of ambient air pollutants on any CHDs and some specific isolated CHDs (12,13). Additionally, Yorifuji et al. reported that living within 200 m of a major road increased the risk of adverse birth outcomes including low birth weight as well as preterm birth (14) and caused higher placenta/birth weight ratio (11).
The exact biological mechanism how maternal exposures to the above environmental risk factors on CHDs is unknown. One potential mechanism may be through oxidative stress. Emerging evidence showed that redox-sensitive signal transduction pathways are critical for developmental processes, including proliferation, differentiation, and apoptosis (15). Teratogens (organic solvent, pesticides, rodenticides, formaldehyde, heavy metal, and tobacco smoke) and other factors like air pollution may induce teratogenesis via inducing oxidative stress and then misregulation of normal pathway (11,14,15). In addition, air pollution could lead to inflammation, coagulation, impaired endothelial function, and hemodynamic responses that may impaired placental oxygen and nutrient transport function, thus interfere with the embryo organogenesis (16).
We also found that maternal perinatal diseases (including fever, diabetes, influenza, threatened abortion) and antibiotics use at first trimester were associated with CHDs. Among these factors, antibiotic use was observed to have the highest OR of ~4.0 for CHDs. Our findings supported the previous studies by Hernandez-Diaz et al. (17) and Czeizel et al. (18), which consistently demonstrated that maternal exposure to trimethoprim–sulfonamide treatment during the first trimester was associated with 2–3-folds of the risk of CHD. It has been suggested that trimethoprim–sulfonamide as folate antagonists works by inhibiting dihydrofolate reductase, with a similar mode of action to that of the recognized teratogenic drug methotrexate, is suspected of inducing malformations when given during the critical period (19,20). Maternal self-reported exposure to trimethoprim–sulfonamide is very low in this study (only two in cases and zero in controls), and a couple of mothers did not report or remember the exact name of the antibiotics. Therefore, the association of each type of antibiotics and CHDs need to be further assessed. Other studies have not shown a statistically significant association between the use of other types of antibiotics—including ampicillin/penicillin and maternal vaginal metronidazole—and CHD (21,22,23). Mechanisms for the effect of other antibiotics on birth defect are not clear. Besides direct effects of antibiotics on CHD, the underlying infection of urogenital tract or other area should also be taken into consideration when interpreting the finding for antibiotics. In China, frequent and inappropriate use of antibiotics in primary healthcare settings is a serious problem. Antibiotics were prescribed for 78.0% of colds and 93.5% of cases of acute bronchitis (24). In addition, people can purchase antibiotics over the counter without a prescription and had a high rate of self-medication (25). This implies that widely antibiotics use may have an important public health impact on the whole population in China, especially among pregnant women.
Maternal fever was found as a risk factor for various CHDs with a range of ORs from 1.83 to 3.91 (OR of 46.88 for multiple defects with a wide CI) in the current study. Our results are consistent with prior studies that suggest that maternal febrile illnesses during the first trimester of pregnancy may be associated with elevated risk for certain heart defects, including heart defects as a whole (OR: 1.8–2.9) (7,26,27), conotruncal defects (OR: 1.55) (28), VSD (OR: 1.8) (29), etc. The mechanism by which maternal febrile illnesses may result in malformations is unclear. One possibility is apoptosis, which is known to be involved in cardiac morphogenesis and can be altered by both fever and infection (30,31). Another possibility is the direct effect of the underlying infection causing fever, such as maternal rubella infection. However, we are usually unable to distinguish between the independent and joint effects between maternal fever and infection. In our study, an association was found between maternal fever as well as influenza with CHDs, but not for other viral infections.
Threatened abortion is another risk factor in our study population, for which prior literature is limited. In China, many pregnant women who have threatened abortion take medicine such as progesterone (32), Chinese patented drugs, or Chinese herbs (33) to prevent miscarriage. The current study has identified a trend (not statistically significant) of elevated risks for isolated CHDs and VSD relation to maternal use of Chinese herbs. Therefore, it is unclear whether the threatened abortion itself or the drugs used to prevent miscarriage disturbed the development of the heart.
Additionally, we found advanced maternal age, low maternal SES, including low household income and education and mother’s occupation as manual worker, and paternal alcohol intake were statistically associated with several types of CHDs, which are consistent with the findings of Miller et al. (34), Yang et al. (35), and Abel (36). Miller et al. (34) postulated that advanced maternal age may be associated with the use of assisted reproductive technology and increased incidence of maternal comorbidities such as diabetes, obesity, hypertension, and medication use, which may help explain the association between advanced maternal age and CHD (34). Yang et al. (35) stated that education, occupation, and income are three common measures of SES. Abel (36) reported paternal alcohol consumption has been associated with abnormalities in offspring such as increases in VSD and speculated that paternal exposure to risk factors may act directly through induction of male germ cell mutation or interference with epigenetic pathways.
When comparing the profile of risk factors by different types of CHD, we found that these risk factors differed significantly between isolated heart defects and multiple defects, which suggests that these factors may have organic specific effects, and be likely to affect the development of fetal heart via epigenetic mechanism for regulating gene transcription (37,38). On the other hand, most risk factors identified among subtypes of CHDs are common and exerted similar strength of effects, which implies that these factors might influence the developmental pathway for a part of the heart or a common pathway for several parts of the heart at the same time. Most risk factors were not significantly related to multiple defects which may be due to the small sample size in multiple defects (the 95% CIs were very large and overlapping for all factors for multiple defects). Future studies with larger sample size may be needed.
Among the few existing studies on this subject, this is the largest one attempting to explore the association of multiple potentially modifiable environmental, demographic, and clinical factors and congenital heart malformations in Guangdong, South of China. In addition, to our knowledge, ours is the first population-based study to assess the associations between various risk factors and different classification of CHDs.
However, one major concern is CHD’s heterogeneity by lumping all the CHDs together or even grouping them to isolated/multiple defects in analysis. To address this issue, we have examined the risk factors of more specific defects like isolated VSD, ASD, pulmonary stenosis, and transposition of great artery, in order to generate more “homogeneity.” Recall bias is always a concern for case–control studies, since interviews were conducted up to a year after the birth or termination of the child, and mother of a case may recall and report exposures more completely than mothers of control subjects. To minimize this bias, a pregnancy calendar was used in conjunction with specific questions, helping to remind mothers of major milestones of pregnancy, especially in the first trimester. A multilevel structured questionnaire and detail about the questions (e.g., timing, specific exposure) was also used to help remind mothers of specific exposures. Additionally, a control subject was always interviewed after his/her matched case, and the difference in the conception times of a case and matched control was no more than 3 mo. The cases and controls therefore had similar intervals between interviews and birth. Also, we matched the controls to cases by infant sex, time of conception (fluctuating within 3 mo), and parents’ residence to make them more comparable except for the potential risk factors studied.
Selection bias may also be a concern for case–control studies. However, in this study, the total response rate was ~70%, which lessens this concern. A major limitation is the lack of detailed information on frequency or dosage of chemical contact, passive smoking, antibiotic use, Chinese herbs use, and paternal alcohol intake and smoking, which limited our ability to assess these factors. However, we plan to collect this information in our new cohort. Another unavoidable problem is that some exposures are quite rare in the population, such as the rate of exposure to organic solvents and farm chemicals. These occurred in only 0.15% of the control babies and 1.23% of the entire study population. Also, since some chemical species or organic solvents are difficult to be named or separated by pregnant women, we combined small grouping of chemicals together, making these variables less specific, but easy to be understood by public to avoid underreporting. Even by doing so, the CI for OR for harmful chemical contact was still very broad in the study due to small sample size. These in turn may induce exposure misclassification. Living in newly renovated room may be a surrogate for environmental exposure and SES marker.
In conclusion, this study found that maternal chemical contact, living in newly renovated rooms, residential proximity to main traffic <50 m, paternal smoking, and maternal occupation as manual worker were significantly associated with CHDs in Guangdong population. Additionally, perinatal diseases/medication factors, including antibiotic use, maternal fever, diabetes, influenza, and threatened abortion, were also risk factors of CHDs. Also, advanced maternal age, low SES (low household income, education, and occupation), and paternal alcohol intake were associated with most CHDs subtypes. Isolated heart defects and multiple defects have different etiologic factors, but different subtypes of CHD share similar risk factors. Environmental factors seem to be the strongest risk factors.
Methods
Design and Population
This is a population-based matched case–control study. We identified live-born infants and stillborn fetuses (over 17 wk gestation) diagnosed with CHDs (1 January 2004–31 December 2013) using data from GRCHD, which is an ongoing population-based CHD surveillance system established in 2004. The GRCHD included 39 collaborative hospitals, covering 20 cities actively reporting birth defects and conducted surveys for risk factors among mothers who had been living in the monitored district of Guangdong Province for more than 6 mo before becoming pregnant. All the CHD cases were confirmed by B-mode echocardiography, cardiac catheterization, surgery, or autopsy.
Inclusion criteria. To minimize recall bias of exposure by mothers to the greatest extent, all cases and controls were recruited when they were younger than 1 y. Cases from miscarriages and terminations of pregnancy after prenatal diagnosis were also included.
Exclusion criteria. Cases with syndromes caused by gene mutations or chromosomal aberrations with preconception origin and nonsingleton cases were excluded from the study. ASD cases diagnosed prenatally, and preterm infants (<38 wk gestation) with patent ductus arteriosus as an isolated heart defect were also excluded because patent ductus arteriosus is likely to disappear postnatally.
Definition of Cases and Controls
The defects were coded using a modified code from the International Classification of Diseases (ICD), 10th Revision (Q20.000–Q28.000) and classified according to the criteria of US NBDPS (3). Isolated heart defects and multiple defect cases were distinguished depending on whether extracardiac anomalies were absent or present, respectively. Controls were randomly chosen singleton newborn infants without any malformation, born in the same hospital as the cases, and matched at the rate of 1:1 by infant sex, time of conception, and parents’ residence.
Data Sources
All forms of CHD cases were mandatory to be reported by obstetricians, ultrasound physicians, and pediatricians to the national registry system and GRCHD (in detailed information). Case reporters routinely collected information on demographics (maternal age, parity, gestational age, birth weight, maternal race/ethnicity, and infant sex) and clinical information (structural heart defects, chromosomal abnormalities, and syndromes) from medical files including records from hospital, ultrasound, surgery, autopsy, and genetic or chromosomal examination for CHDs and control babies. CHDs and extracardiac defects are coded by two trained cardiovascular epidemiologists.
Face-to-face interviews were conducted during the mother’s stay in inpatient or outpatient departments when the babies were younger than 1 y. A structured, standardized questionnaire obtained information during pregnancy on: (i) sociodemographic factors (maternal age, family income, maternal education); (ii) maternal pregnancy history (parity, family history of heart defects, previous pregnancies with still birth); (iii) maternal environmental factors (living near Pearl River, chemicals contact, passive smoking, paternal smoking, living in newly renovated rooms, residential proximity to traffic, pet contact) and occupation; (iv) maternal perinatal diseases and medication use during the first trimester (maternal perinatal diseases: fever, viral infection, diabetes, threatened abortions, stress, other infections, etc. Medication use during pregnancy includes antibiotics, contraceptive medicine, and Chinese herbs); and (v) paternal alcohol intake before pregnancy.
All cases from the complete network were screened and duplicates checked. If a case was diagnosed both prenatally and postnatally, we used the postnatal diagnosis. The questionnaires and clinical results for all the cases and controls were examined by the two experienced cardiovascular epidemiologists. Case–control matching was also double checked. For this study, only those cases that were reported within the first year after birth or pregnancy termination were selected.
Definition of Potential Risk Factors
Maternal age at birth was grouped as 30–34, 35–40, and >40 y by compared to <30 y as the reference. Household income of <1,000 yuan/mo/person was compared to ≥1,000 yuan (as the reference). Maternal education less than high school was compared to high school or above (reference group). Other variables were classified by a dichotomous yes or no response.
All exposures were asked if they occurred during the critical period, i.e., from 3 mo before pregnancy through the first trimester, as the defined exposure window of this study. Chemical contact was defined as occupational or long-term use of any of the harmful chemicals comprising any organic solvent or farm chemicals (including Herbicides, Pesticides, and Rodenticides). The mothers were given a list of general names and scientific names of possible hazardous chemicals and were asked to supplement ones that have not been listed in the questionnaire. Passive smoking was defined as maternal self-reported exposure to environmental tobacco smoke at home, workplace, or both. Living in newly renovated rooms means mother moving into a new house within 6 mo after decoration. Manual worker was defined as people working in handicraft industry, working by hand, or operating machine in manufactory. Unemployed means that mother lost job during the critical period. Maternal diabetes included pregestational and gestational, type I and type II diabetes. Paternal smoking was defined as smoking on average at least one cigarette per day. Threatened abortion means experiencing symptoms of miscarriage like vaginal bleeding from the first 20 wk of pregnancy to pregnancy end. Antibiotic use was defined as using any type of antibiotics at least 1 d. Alcohol intake means a reported alcohol intake of on average at least 50 ml/d without specifying wine.
Statistical Analysis Methods
A matched case–control analysis was performed to assess the potential risk factors of CHD by computing and comparing the exposure ratios overall and within different groups of CHD. Potential risk factors were first screened and chosen by bivariate analysis. Those variables significant in bivariate analyses (P < 0.05) were then put into a full model of multivariate logistic regression analysis. The adjusted ORs for different groups of CHD and their 95% CI were assessed using the full model while simultaneously controlling for other potential risk factors. Comparison of risk factors and their ORs were also conducted between isolated CHDs and multiple defects and different subtypes of CHDs. We used SAS-PC for computation (9.3 v, SAS Institute, Raleigh, NC).
Ethics Issue
GRCHD was granted authority to conduct CHD surveillance and risk factors investigation in Guangdong Province. The study was approved by the Guangdong General Hospital Human subjects committee. Informed consent was obtained from the parents of the study population.
Statement of Financial Support
This study was supported by the National Twelve-Fifth Scientific Research Project, China (Grant No. 2011BAI11B22) and National Basic Research Project of China (Grant No. 2010CB529504), Guangdong International Cooperative Project, China (No. 2014A050503048), Guangdong Province Science and Technology Planning Project of China (No. 2011B031900002 and No. 2012B032000014).
Disclosure
The authors declare that they have no conflicts of interest.
References
Donofrio MT, Moon-Grady AJ, Hornberger LK, et al.; American Heart Association Adults With Congenital Heart Disease Joint Committee of the Council on Cardiovascular Disease in the Young and Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and Council on Cardiovascular and Stroke Nursing. Diagnosis and treatment of fetal cardiac disease: a scientific statement from the American Heart Association. Circulation 2014;129:2183–242.
Jenkins KJ, Correa A, Feinstein JA, et al.; American Heart Association Council on Cardiovascular Disease in the Young. Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation 2007;115:2995–3014.
Botto LD, Lin AE, Riehle-Colarusso T, Malik S, Correa A ; National Birth Defects Prevention Study. Seeking causes: classifying and evaluating congenital heart defects in etiologic studies. Birth Defects Res A Clin Mol Teratol 2007;79:714–27.
Gorini F, Chiappa E, Gargani L, Picano E. Potential effects of environmental chemical contamination in congenital heart disease. Pediatr Cardiol 2014;35:559–68.
Gilboa SM, Desrosiers TA, Lawson C, et al.; National Birth Defects Prevention Study. Association between maternal occupational exposure to organic solvents and congenital heart defects, National Birth Defects Prevention Study, 1997-2002. Occup Environ Med 2012;69:628–35.
Shaw GM, Nelson V, Iovannisci DM, Finnell RH, Lammer EJ. Maternal occupational chemical exposures and biotransformation genotypes as risk factors for selected congenital anomalies. Am J Epidemiol 2003;157:475–84.
Ferencz C, Correa-Villasenor A, Loffredo CA, eds. Genetic and Environmental Risk Factors of Major Cardiovascular Malformations: The Baltimore-Washington Infant Study: 1981–1989. Armonk, NY: Futura Publishing Co., 1997.
Liu Z, Li X, Li N, et al. Association between maternal exposure to housing renovation and offspring with congenital heart disease: a multi-hospital case-control study. Environ Health 2013;12:25.
Drake VJ, Koprowski SL, Lough J, Hu N, Smith SM. Trichloroethylene exposure during cardiac valvuloseptal morphogenesis alters cushion formation and cardiac hemodynamics in the avian embryo. Environ Health Perspect 2006;114:842–7.
Watson RE, Jacobson CF, Williams AL, Howard WB, DeSesso JM. Trichloroethylene-contaminated drinking water and congenital heart defects: a critical analysis of the literature. Reprod Toxicol 2006;21:117–47.
Yorifuji T, Naruse H, Kashima S, et al. Residential proximity to major roads and placenta/birth weight ratio. Sci Total Environ 2012;414:98–102.
Ritz B, Yu F, Fruin S, Chapa G, Shaw GM, Harris JA. Ambient air pollution and risk of birth defects in Southern California. Am J Epidemiol 2002;155:17–25.
Gilboa SM, Mendola P, Olshan AF, et al. Relation between ambient air quality and selected birth defects, seven county study, Texas, 1997-2000. Am J Epidemiol 2005;162:238–52.
Yorifuji T, Naruse H, Kashima S, et al. Residential proximity to major roads and adverse birth outcomes: a hospital-based study. Environ Health 2013;12:34.
Jason MH. Oxidative stress as a mechanism of teratogenesis. Birth Defects Research (Part C) 2006;78:293–307.
Kannan S, Misra DP, Dvonch JT, Krishnakumar A. Exposures to airborne particulate matter and adverse perinatal outcomes: a biologically plausible mechanistic framework for exploring potential effect modification by nutrition. Environ Health Perspect 2006;114:1636–42.
Hernández-Díaz S, Werler MM, Walker AM, Mitchell AA. Folic acid antagonists during pregnancy and the risk of birth defects. N Engl J Med 2000;343:1608–14.
Czeizel AE, Rockenbauer M, Sørensen HT, Olsen J. The teratogenic risk of trimethoprim-sulfonamides: a population based case-control study. Reprod Toxicol 2001;15:637–46.
Andersen JT, Petersen M, Jimenez-Solem E, et al. Trimethoprim use prior to pregnancy and the risk of congenital malformation: a register-based nationwide cohort study. Obstet Gynecol Int 2013;2013:364526.
Feng Y, Wang S, Chen R, Tong X, Wu Z, Mo X. Maternal folic acid supplementation and the risk of congenital heart defects in offspring: a meta-analysis of epidemiological observational studies. Sci Rep 2015;5:8506.
Czeizel AE, Rockenbauer M, Olsen J, Sørensen HT. Oral phenoxymethylpenicillin treatment during pregnancy. Results of a population-based Hungarian case-control study. Arch Gynecol Obstet 2000;263:178–81.
Dencker BB, Larsen H, Jensen ES, Schønheyder HC, Nielsen GL, Sørensen HT. Birth outcome of 1886 pregnancies after exposure to phenoxymethylpenicillin in utero. Clin Microbiol Infect 2002;8:196–201.
Czeizel AE, Sørensen HT, Rockenbauer M, Olsen J. A population-based case-control teratologic study of nalidixic acid. Int J Gynaecol Obstet 2001;73:221–8.
Wang J, Wang P, Wang X, Zheng Y, Xiao Y. Use and prescription of antibiotics in primary health care settings in China. JAMA Intern Med 2014;174:1914–20.
Lv B, Zhou Z, Xu G, et al. Knowledge, attitudes and practices concerning self-medication with antibiotics among university students in western China. Trop Med Int Health 2014;19:769–79.
Botto LD, Panichello JD, Browne ML, et al.; National Birth Defects Prevention Study. Congenital heart defects after maternal fever. Am J Obstet Gynecol 2014;210:359.e1–359.e11.
Botto LD, Erickson JD, Mulinare J, Lynberg MC, Liu Y. Maternal fever, multivitamin use, and selected birth defects: evidence of interaction? Epidemiology 2002;13:485–8.
Adams MM, Mulinare J, Dooley K. Risk factors for conotruncal cardiac defects in Atlanta. J Am Coll Cardiol 1989;14:432–42.
Botto LD, Lynberg MC, Erickson JD. Congenital heart defects, maternal febrile illness, and multivitamin use: a population-based study. Epidemiology 2001;12:485–90.
Edwards MJ. Apoptosis, the heat shock response, hyperthermia, birth defects, disease and cancer. Where are the common links? Cell Stress Chaperones 1998;3:213–20.
Roulston A, Marcellus RC, Branton PE. Viruses and apoptosis. Annu Rev Microbiol 1999;53:577–628.
Yassaee F, Shekarriz-Foumani R, Afsari S, Fallahian M. The effect of progesterone suppositories on threatened abortion: a randomized clinical trial. J Reprod Infertil 2014;15:147–51.
Li L, Dou L, Leung PC, Wang CC. Chinese herbal medicines for threatened miscarriage. Cochrane Database Syst Rev 2012;5:CD008510.
Miller A, Riehle-Colarusso T, Siffel C, Frías JL, Correa A. Maternal age and prevalence of isolated congenital heart defects in an urban area of the United States. Am J Med Genet A 2011;155A:2137–45.
Yang J, Carmichael SL, Canfield M, Song J, Shaw GM ; National Birth Defects Prevention Study. Socioeconomic status in relation to selected birth defects in a large multicentered US case-control study. Am J Epidemiol 2008;167:145–54.
Abel E. Paternal contribution to fetal alcohol syndrome. Addict Biol 2004;9:127–33; discussion 135–6.
Zhang QJ, Liu ZP. Histone methylations in heart development, congenital and adult heart diseases. Epigenomics 2015;7:321–30.
Vallaster M, Vallaster CD, Wu SM. Epigenetic mechanisms in cardiac development and disease. Acta Biochim Biophys Sin (Shanghai) 2012;44:92–102.
Acknowledgements
We thank all the collaborated hospitals for their great efforts in screening/diagnosing CHD and interviewing the studied population (hospital names are listed in the Supplementary Data online).
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Data
(DOCX 18 kb)
PowerPoint slides
Rights and permissions
About this article
Cite this article
Ou, Y., Mai, J., Zhuang, J. et al. Risk factors of different congenital heart defects in Guangdong, China. Pediatr Res 79, 549–558 (2016). https://doi.org/10.1038/pr.2015.264
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2015.264
This article is cited by
-
Lower Socioeconomic Status is Associated with an Increased Incidence and Spectrum of Major Congenital Heart Disease and Associated Extracardiac Pathology
Pediatric Cardiology (2024)
-
Maternal periconceptional environmental exposure and offspring with congenital heart disease: a case–control study in Guangzhou, China
BMC Pregnancy and Childbirth (2023)
-
Associations between ambient heat exposure early in pregnancy and risk of congenital heart defects: a large population-based study
Environmental Science and Pollution Research (2022)
-
Maternal exposure to life events during pregnancy and congenital heart disease in offspring: a case-control study in a Chinese population
BMC Pregnancy and Childbirth (2021)
-
Neighbourhood maternal socioeconomic status indicators and risk of congenital heart disease
BMC Pregnancy and Childbirth (2021)