Abstract
Background:
Surfactant replacement therapy is the gold standard treatment of neonatal respiratory distress (RDS). Nebulization is a noninvasive mode of surfactant administration. We administered Poractant alfa (Curosurf) via a vibrating perforated membrane nebulizer (eFlow Neonatal Nebulizer) to spontaneously breathing preterm lambs during binasal continuous positive pressure ventilation (CPAP).
Methods:
Sixteen preterm lambs were operatively delivered at a gestational age of 133 ± 1 d (term ~150 d), and connected to CPAP applied via customized nasal prongs. Nebulization was performed (i) with saline or (ii) with surfactant for 3 h in humidified or (iii) nonhumidified air, and with surfactant (iv) for 60 min or (v) for 30 min. We measured arterial oxygenation, lung gas volumes and surfactant pool size and deposition.
Results:
Nebulization of surfactant in humidified air for 3 h improved oxygenation and lung function, and surfactant was preferentially distributed to the lower lung lobes. Shorter nebulization times and 3 h nebulization in dry air did not show these effects. Nebulized surfactant reached all lung lobes, however the increase of surfactant pool size missed statistical significance.
Conclusion:
Positive effects of surfactant nebulization to spontaneously breathing preterm lambs depend on treatment duration, surfactant dose, air humidity, and surfactant distribution within the lung.
Similar content being viewed by others
Main
A major cornerstone of therapy of respiratory distress syndrome (RDS) in preterm neonates has been the introduction of surfactant replacement therapy (1). Surfactant replacement improves gas exchange and decreases mortality (2,3), and proved to be efficient in the prevention (4) and in the therapy of neonatal RDS (5). Surfactant is delivered to the lung of intubated and mechanically ventilated babies as a bolus via an endotracheal tube in most instances. However, endotracheal intubation is a physiologically stressful procedure (6). Bolus administration of surfactant holds the risk of acute airway obstruction with consecutive hypoxia and bradycardia (7). Newer techniques focus on less invasive surfactant administration (LISA), combining bolus surfactant therapy with continuous positive airway pressure (CPAP) by utilizing a small tube inserted into the trachea (8,9,10). However, this can only be performed by very skilled personnel, and still requires laryngoscopy and potentially a Magill forceps.
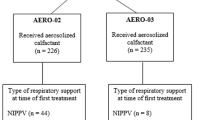
In the search for an alternative way to administer surfactant to the lung as gentle and noninvasive as possible, nebulization is a historic, but still innovative approach (11,12). Until now, there have been four clinical studies on nebulized surfactant as rescue therapy (13,14,15,16). These studies confirmed the safety and feasibility of the method. However, only one showed an immediate positive effect on oxygen delivery to treated infants (16). In addition, a clinical study recently presented by Minocchieri on the Pediatric Academic Societies Meeting 2013 reported a reduced need for intubation in preterm infants with RDS receiving CPAP plus nebulized surfactant in the first hours of life.
In order to study nebulization as a noninvasive technique, various animal models were established. Positive effects of nebulized surfactant on ventilatory parameters like lung compliance and oxygenation have been described in animal models using tracheostomized and ventilated premature lambs (17). Furthermore, distribution of nebulized surfactant to the lung was more homogenous compared to bolus surfactant in a rabbit model (18).
In our study, we tested a customized vibrating perforated membrane nebulizer (eFlow Neonatal Nebulizer System) for delivery of a widely used animal derived surfactant (Poractant alfa) (19) in premature lambs receiving binasal CPAP. We hypothesized that the combination of binasal CPAP and nebulized surfactant would result in improvement of oxygenation and lung function. We further hypothesized that nebulization would increase surfactant pool size in a dose-dependent manner, and that surfactant nebulization would result in homogenous distribution of surfactant to different lung lobes irrespective of different technical parameters like dose, treatment duration and air humidity.
Results
Nebulization of Surfactant Versus Saline
Three hours nebulization of surfactant in humidified air resulted in a significantly higher arterial partial pressure of oxygen (PaO2) at the end of the experiment compared to saline nebulization (P < 0.05) ( Figure 1 ). Lung gas volumes were significantly higher in the group treated with surfactant in humidified air compared to control animals (P < 0.05) ( Figure 2 ). The average total amount of surfactant nebulized in this group was 861 mg/kg body weight.
Arterial partial pressure of oxygen (PaO2) was significantly higher in animals nebulized 3 h with surfactant (squares) compared to saline (circles) at the end of the experiment (mean ± SEM, *P < 0.05).
Lung gas volumes corrected for body weight (ml/kg) were significantly higher in animals nebulized 3 h with surfactant (squares) compared to saline (circles), (mean ± SEM, *P < 0.05).
In animals nebulized with surfactant in nonhumidified air for 3 h, PaO2 at the end of the experiment was significantly lower than in the group treated with nebulized surfactant in humidified air (P < 0.05) ( Table 1 ), while there was no difference to control (P = 0.467). Lung gas volumes showed no significant improvement after 3 h nebulization of surfactant in nonhumidified air ( Table 1 ). The total amount of surfactant nebulized in this group was 978 mg/kg body weight, which was not different from animals nebulized with surfactant for 3 h and humidified air. In all experimental groups, we observed mild hypercapnia at the end of the experiment ( Table 1 ).
Effect of Dose and Duration of Surfactant Treatment on Deposition of Nebulized Surfactant
Animals nebulized with surfactant for 60 min did not show significant improvements of PaO2 or lung gas volumes compared to control ( Table 1 ). Animals in this group were nebulized with an average of 437 mg/kg body weight surfactant in total.
Animals nebulized with surfactant for 30 min also did not show significant improvements of PaO2 or lung gas volumes compared to control ( Table 1 ), and was stopped at n = 2. Animals in this group were nebulized with an average of 229 mg/kg BW body weight surfactant in total.
The total amount of surfactant nebulized in both groups was significantly lower compared to animals nebulized with surfactant for 3 h, although the average amount of surfactant nebulized per minute was higher with decreasing nebulization times, i.e., 0.18, 0.26, and 0.33 ml/min in the “3h”, “60min”, and “30min” group, respectively.
Disaturated Phospholipids in the Lung
Surfactant nebulization for 3 h and 60 min increased DSPL pool size compared to saline nebulization 2.9- and 3.7-fold, respectively, however this effect was not statistically significant (P = 0.057 and P = 0.057 vs. control, respectively, Figure 3 ). DSPL pool size did not significantly differ between different surfactant nebulization groups ( Figure 3 ).
DSPL pool size recovered from BALF relative to body weight was increased by surfactant nebulization (mean ± SEM), however missing statistical significance compared to saline nebulization (P = 0.057 “3h” vs. “saline” and p=0.057 “60min” vs. “saline”, respectively).
Surfactant Distribution to the Lung
In all groups nebulized with surfactant, surfactant was distributed to each lung lobe ( Figure 4 ). In the “3h” group, there was a significant difference in distribution between all lobes, with a preference for the lower lobes compared to the whole lung. Surfactant distribution to different lung lobes in the other treatment groups did not show significant differences ( Figure 4 ). Surfactant distribution to the stomach was low in all nebulized animals ( Table 1 ).
Surfactant distribution to different lung lobes relative to the whole lung, measured by Sm2O3 levels (LLL, left lower lobe; LUL, left upper lobe; RLL, right lower lobe; RML, right middle lobe; RUL, right upper lobe; *P < 0.05).
Discussion
In our study, nebulization of natural surfactant in humidified air for 3 h improved physiological parameters like oxygenation and lung function in spontaneously breathing preterm lambs. This is in line with previous experimental findings, showing that nebulization of synthetic surfactant using CPAP increased lung compliance in anaesthetized lambs receiving CPAP (20) and both lung compliance and oxygenation in lavaged rabbits (21), and a clinical study on nebulized surfactant which reported an improvement of the (A/a) O2 gradient compared to control (16).
We used a preterm sheep model, which included two major advantages: First, the similarity in anatomy and size allowed the use of equipment which is originally used in humans. Secondly, maturation of the lung closely resembles that of humans (22). Preterm lambs at this age have a sufficient respiratory drive, allowing the use of CPAP. We found positive physiological effects of surfactant nebulization using binasal CPAP provided by prongs. In contrary, previous animal studies which showed positive effects of nebulized natural surfactant on lung function have mainly focused on tracheostomized, intubated, and ventilated sheep (17,23) or rabbits (18,24). Our data indicate that nebulized surfactant reached the lung and was deposited in all lung lobes. Positive treatment effects of 3 h surfactant nebulization may arise from both increased surfactant pool size and the pattern of surfactant distribution to different lung lobes. According to previous data, we would have expected that the upper lobes of both sides were preferred. In tracheostomized animals, the greatest recovery of surfactant both after nebulization and bolus application of surfactant was observed in the right upper lobe (17,25). The upper lobes develop faster than the remaining lobes (22), and are therefore supposed to show advanced surfactant production compared to the lower lobes. In our study, the preferred distribution to the lower, less developed lung lobes might therefore have contributed to the positive effect of surfactant nebulization. This preference might also result from spontaneous breathing during CPAP support, as surfactant bolus administration during CPAP resulted in preferential distribution to lower lobes compared to intubation in a previous study from our group (26).
However, we observed that the nebulized amount of surfactant by the device had to be very high for a clinical effect. In order to reduce the amount of surfactant nebulized and to compare the effects of lower doses in our setting, we shortened nebulization times. However, lower doses of nebulized surfactant did not result in significant improvements of oxygenation and lung function, despite an increase in surfactant pool size comparable to the 3 h group. Furthermore, we observed a nonlinear rate of surfactant nebulization over time. We hypothesize that this nonlinear surfactant delivery resulted from the fact that all animals underwent NIPPV in the first 15 min, which meant a higher percentage of NIPPV during nebulization in the 60 and 30 min group. We also could not reproduce the preferential distribution to the lower lung lobes in the shorter experiments. These findings indicate that in addition to surfactant pool size, the distribution pattern of surfactant within the lung influences treatment benefits from surfactant nebulization.
Surprisingly, we also found that nebulization with dry air instead of humidified air, which is a common situation when CPAP is applied during transition in the delivery room, did not result in significant improvement of physiological parameters, although the amount of surfactant used for treatment did not differ from animals nebulized with surfactant in humidified air. This was unexpected because nonconditioning of inspired gas did not result in abnormal gas exchange or lung function in a previous study in intubated preterm lambs ventilated for 3 h (27). However, in our study, animals nebulized with dry air showed highest surfactant pools in the right upper lobe, a finding which has been previously described in tracheostomized animals (17,25). These findings support the importance of the surfactant distribution pattern within the lung for therapeutic benefit. However, the interactions between surfactant dosing, treatment duration, and air humidity remain complex. Further studies are needed to elucidate the influence of air humidity on surfactant distribution, surfactant clearance, and surfactant droplet formation in spontaneously breathing animals.
Beside these parameters, pharmacological and technical aspects influence effects of surfactant nebulization. Different surfactants might vary in their suitability for nebulization, which is reflected by the great quantity of different preparations of surfactant that have been tested in both animal and clinical studies (12). In our study, we used Poractant alfa, an animal-derived surfactant which proved to be advantageous compared to different surfactant preparations regarding rapid onset of action, less need for redosing, and higher survival free of BPD in preterm infants (28), and regarding mortality (29) after bolus administration. Recently, an artificial surfactant aerosolized in a piglet model of acute lung injury resulted in improved gas exchange (30). We have previously shown that artificial surfactant with two protein analogs was more resistant to inactivation when given as bolus (31). However, physiological differences between the acute lung injury model and our preterm RDS model have to be taken into account when comparing different surfactant preparations. In addition, different nebulization techniques showed differences in their suitability for surfactant nebulization (32), and different surface active substances affected nebulization depending on the nebulizer (33). The nebulizer we used has been reported to be suitable for nebulization of Poractant alfa, and surfactant characteristics were similar before and after nebulization (34).
Our study is limited by the fact that we found endogenous surfactant also in control animals. We believe that endogenous surfactant production was induced by maternal steroid treatment given prenatally for maturation of the animals (35). However, in our opinion, this setting best reflects the clinical situation, as prenatal corticosteroid treatment for women at risk of preterm birth is the gold standard (36). In addition, we refrained from using animals of younger gestational age to maintain a sufficient intrinsic drive for breathing without additional drugs like caffeine, which might have had additive effects on endogenous surfactant production (37).
Our study might also be limited by the use of binasal prongs for CPAP, which reached about 2 cm into the nostrils. Although the amount of surfactant measured in the stomach was surprisingly low, we might underestimate surfactant losses into the mouth, within the nose and in the esophageal groove, as well as additional dilution by saliva and gastric secretion. However, in our opinion, binasal CPAP using prongs best reflects the clinical situation and has proven to be beneficial in a clinical setting (38). Furthermore, the combination of CPAP and nebulization resulted in blood gas values acceptable within the limits of permissive hypercapnia, and are comparable to values of lambs receiving CPAP alone (39). Additionally, we did not observe complications such as pneumothorax during CPAP and nebulization, further indicating the safety of the method.
In conclusion, our model allowed surfactant nebulization in a near-clinical setup using binasal CPAP in spontaneously breathing premature lambs. In combination with a customized nebulizer, surfactant was distributed to the lung of the animals and improved physiological parameters. However, the interaction between surfactant dose, treatment duration, air humidity, and local surfactant distribution remains complex. By using translational models to identify pharmacological and technical factors influencing surfactant distribution and treatment effects, nebulization might allow surfactant therapy in the least invasive and most sophisticated way.
Methods
Animals and Delivery Protocol
Animal experiments were approved by the Institutional Animal Ethics Committee of Maastricht University. Sixteen preterm lambs were operatively delivered from time-mated Texel ewes at a gestational age of 133 ± 1 d (term ~150 d gestational age), at which lung maturation resembles ~30–32 wk of gestation in humans (22). One day before the experiment, the ewe received an intramuscular injection with 12 mg betamethasone (Celestone Chronodose, Schering-Plough, North Ryde, New South Wales, Australia) to induce fetal lung maturation (35).
Caesarean section was performed through midline incision under spinal and local subcutaneous analgesia with 2% lidocaine. The fetus was delivered head first, and an arterial catheter was placed in the umbilical artery through a modified EXIT procedure (26), allowing monitoring of arterial blood pressure (ABP) and heart rate (HR), blood-gas analysis, and parenteral nutrition.
After cord clamping, the preterm lambs were weighed (ICI6000S balance, Sartorius, Göttingen, Germany). Each lamb was brought to an open, heated incubator (IW930 Series CosyCot Infant Warmer, Fisher & Paykel Healthcare, Auckland, New Zealand) maintaining a body temperature of 38 °C. Body temperature was monitored by placing a rectal temperature probe.
Directly after transferring the lambs to the open incubator, custom made bi-nasal prongs were fitted and the spontaneously breathing lambs were connected to noninvasive intermittent positive pressure ventilation (NIPPV) for 15 min using an infant ventilator (Babylog 8000, Draeger, Luebeck, Germany). Initial settings were as follows: FiO2 = 1, PEEP 8 cm H2O, PIP 30 cm H2O, frequency 60/min, I:E 1:2. Fifteen minutes after birth, the ventilation was switched to CPAP with a PEEP of 8 cm H2O for the remaining of the experiment. The ventilation circuit was equipped with a standard heated humidifier (MR700, Fisher & Paykel Healthcare) to condition the inflowing gas with humidity.
Poractant alfa (Curosurf, Chiesi Pharmaceuticals, Parma, Italy) was labeled with samarium oxide (Sm2O3) in a 1:1,000 ratio before the experiment to track relative surfactant deposition to different lung lobes and to the stomach (26).
Nebulization was performed using a customized vibrating membrane nebulizer (eFlow Neonatal Nebulizer System, PARI Pharma, Munich, Germany), which was placed between the prongs and the connection to the ventilator circuit. It was designed to generate a particle size that was optimized to target the small airways (mass median diameter 2.6–3.3 µm with saline and mass median aerodynamic diameter of nebulized Curosurf of 2.2–3.0 µm according to manufacturer). Nebulization was started immediately after the connection to the ventilator. For each animal, a new nebulizer was used, and the total amount of nebulized surfactant was documented. The average amount of surfactant nebulized per minute was calculated by dividing the total amount of surfactant by duration of nebulization.
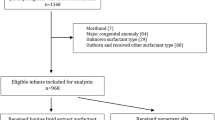
Lambs were randomly assigned to the following five treatment groups: (i) saline nebulization for 3 h (“saline”), (ii) surfactant nebulization for 3 h (“3h”), (iii) surfactant nebulization for 3 h without humidification (“3h dry”), (iv) surfactant nebulization for 60 min (“60min”), and (v) 30 min (“30min”) with humidified air ( Table 2 ). Treatment duration was based on previous lamb studies on less invasive surfactant administration by our group (26).
During the experiment, blood gas analyses were performed on arterial blood at birth (t = 0 min) and regularly after birth at t = 15 min, t = 45 min, t = 75 min, t = 105 min, t = 135 min, and t = 180 min, respectively.
Autopsy
At the end of the experiment, lambs were euthanized by an intravenous injection of 10 ml pentobarbital. Lambs were disconnected from ventilation and the thorax was opened. An endotracheal tube was inserted in the trachea and the lung was inflated to a maximum pressure of 40 cm H20. Deflation gas volumes were recorded and adjusted for body weight as described before (40). The lung was removed from the chest and weighed, and divided into its lobes. Again, each lung lobe was weighed. Additionally, gastric fluid was obtained for measurement of surfactant.
Disaturated Phospholipid (DSPL) Measurements
Lung lobes were isolated and lavaged separately with NaCl 0.9%. For DSPL measurements, 2 ml aliquots were used, while the remaining bronchoalveolar lavage fluid (BALF) was stored together with the belonging lobe. BALF samples were centrifuged for 10 min at 300×g and 4 °C. One milliliter of the supernatant BALF was evaporated overnight at 60 °C under continuous nitrogen gas flow. The dry BALF was dissolved in a mixture of carbon tetrachloride and osmium tetroxide and disaturated phospholipids were isolated by means of alumina column chromatography according to Mason et al. (41). DSPL were dissolved in chloroform and quantified by photometry according to Stewart with some minor modifications as described by Been et al. (42,43). DSPL concentration was correlated to BALF volumes and DSPL pool size of the whole lung was calculated and adjusted for body weight.
Samarium Oxide Measurements
The lung lobes were separately stored together with the belonging BALF fluid and deep-frozen at −20 °C for 24 h, followed by storage in a −80 °C freezer. For analysis, the lung samples were freeze-dried and ashed. Afterwards they were dissolved in a combination of nitric acid and hydrochloric acid, diluted in water. To allow quantification of samarium oxide, measurements were performed by inductively coupled plasma mass spectrometry (ICP-MS) (44). Samarium oxide was measured in stomach fluid samples accordingly. For each animal treated with surfactant, Samarium oxide concentration in the individual lobes was calculated by taking into account the BAL aliquot used for lipid measurement, and was normalized to samarium oxide concentration in the whole lung.
Data Analysis
Results of arterial partial pressure of oxygen (PaO2) measurements and lung gas volumes were given as means ± SEM and compared using one-way ANOVA. Groups of interest were compared using t-test. DSPL and samarium oxide measurement results were given as mean ± SEM and were compared using nonparametric testing (Mann–Whitney test). Groups of interest were compared by Kruskall–Wallis test.
Statistical analysis was performed by IBM SPSS version 20; graphs were drawn with GraphPad Prism v5.0. Significance was accepted at P < 0.05.
Statement of Financial Support
This study was funded by Chiesi Farmaceutici SpA (Parma, Italy), which is the employer of authors Roberta Razzetti and Federico Bianco. The animal derived surfactant Poractant alfa (Curosurf, 80 mg/ml) was also supplied by Chiesi Farmaceutici SpA. The nebulization devices (eFlow Neonatal Nebulizer) were supplied by PARI Pharma GmbH (Munich, Germany), which is the employer of authors Carola Fuchs and Markus Tservistas. There are no further patents, products in development, or marketed products to declare.
References
Wirbelauer J, Speer CP. The role of surfactant treatment in preterm infants and term newborns with acute respiratory distress syndrome. J Perinatol 2009;29 Suppl 2:S18–22.
Jobe AH, Ikegami M. Surfactant metabolism. Clin Perinatol 1993;20:683–96.
Mercier CE, Soll RF. Clinical trials of natural surfactant extract in respiratory distress syndrome. Clin Perinatol 1993;20:711–35.
Soll RF, Morley CJ. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev 2001:CD000510.
Seger N, Soll R. Animal derived surfactant extract for treatment of respiratory distress syndrome. Cochrane Database Syst Rev 2009:CD007836.
Marshall TA, Deeder R, Pai S, Berkowitz GP, Austin TL. Physiologic changes associated with endotracheal intubation in preterm infants. Crit Care Med 1984;12:501–3.
Tarawneh A, Kaczmarek J, Bottino MN, Sant’anna GM. Severe airway obstruction during surfactant administration using a standardized protocol: a prospective, observational study. J Perinatol 2012;32:270–5.
Dargaville PA, Aiyappan A, Cornelius A, Williams C, De Paoli AG. Preliminary evaluation of a new technique of minimally invasive surfactant therapy. Arch Dis Child Fetal Neonatal Ed 2011;96:F243–8.
Göpel W, Kribs A, Ziegler A, et al.; German Neonatal Network. Avoidance of mechanical ventilation by surfactant treatment of spontaneously breathing preterm infants (AMV): an open-label, randomised, controlled trial. Lancet 2011;378:1627–34.
Kribs A, Pillekamp F, Hünseler C, Vierzig A, Roth B. Early administration of surfactant in spontaneous breathing with nCPAP: feasibility and outcome in extremely premature infants (postmenstrual age </=27 weeks). Paediatr Anaesth 2007;17:364–9.
Robillard E, Alarie Y, Dagenais-Perusse P, Baril E, Guilbeault A. Microaerosol administration of synthetic beta-gamma-dipalmitoyl-L-alpha-lecithin in the respiratory distress syndome: a preliminary report. Can Med Assoc J 1964;90:55–7.
Abdel-Latif ME, Osborn DA. Nebulised surfactant in preterm infants with or at risk of respiratory distress syndrome. Cochrane Database Syst Rev 2012;10:CD008310.
Berggren E, Liljedahl M, Winbladh B, et al. Pilot study of nebulized surfactant therapy for neonatal respiratory distress syndrome. Acta Paediatr 2000;89:460–4.
Arroe M, Pedersen-Bjergaard L, Albertsen P, et al. Inhalation of aerosolized surfactant (Exosurf (R)) to neonates treated with nasal continuous positive airway pressure. Prenat Neonat Med 1998;3:346–352.
Finer NN, Merritt TA, Bernstein G, Job L, Mazela J, Segal R. An open label, pilot study of Aerosurf® combined with nCPAP to prevent RDS in preterm neonates. J Aerosol Med Pulm Drug Deliv 2010;23:303–9.
Jorch G, Hartl H, Roth B, et al. Surfactant aerosol treatment of respiratory distress syndrome in spontaneously breathing premature infants. Pediatr Pulmonol 1997;24:222–4.
Lewis JF, Ikegami M, Jobe AH, Tabor B. Aerosolized surfactant treatment of preterm lambs. J Appl Physiol (1985) 1991;70:869–76.
Dijk PH, Heikamp A, Bambang Oetomo S. Surfactant nebulisation: lung function, surfactant distribution and pulmonary blood flow distribution in lung lavaged rabbits. Intensive Care Med 1997;23:1070–6.
van Kaam AH, De Jaegere AP, Borensztajn D, Rimensberger PC ; Neovent Study Group. Surfactant replacement therapy in preterm infants: a European survey. Neonatology 2011;100:71–7.
Wolfson MR, Wu J, Hubert TL, et al. Dose-response to aerosolized KL4 surfactant in the spontaneously breathing CPAP-supported preterm lamb. Pediatr Res 2011;70:751.
Walther FJ, Hernández-Juviel JM, Waring AJ. Aerosol delivery of synthetic lung surfactant. PeerJ 2014;2:e403.
Pringle KC. Human fetal lung development and related animal models. Clin Obstet Gynecol 1986;29:502–13.
Rey-Santano C, Mielgo VE, Andres L, Ruiz-del-Yerro E, Valls-i-Soler A, Murgia X. Acute and sustained effects of aerosolized vs. bolus surfactant therapy in premature lambs with respiratory distress syndrome. Pediatr Res 2013;73:639–46.
Wagner MH, Amthauer H, Sonntag J, Drenk F, Eichstädt HW, Obladen M. Endotracheal surfactant atomization: an alternative to bolus instillation? Crit Care Med 2000;28:2540–4.
Brain JD, Knudson DE, Sorokin SP, Davis MA. Pulmonary distribution of particles given by intratracheal instillation or by aerosol inhalation. Environ Res 1976;11:13–33.
Niemarkt HJ, Kuypers E, Jellema R, et al. Effects of less-invasive surfactant administration on oxygenation, pulmonary surfactant distribution, and lung compliance in spontaneously breathing preterm lambs. Pediatr Res 2014;76:166–70.
Pillow JJ, Hillman NH, Polglase GR, et al. Oxygen, temperature and humidity of inspired gases and their influences on airway and lung tissue in near-term lambs. Intensive Care Med 2009;35:2157–63.
Dizdar EA, Sari FN, Aydemir C, et al. A randomized, controlled trial of poractant alfa versus beractant in the treatment of preterm infants with respiratory distress syndrome. Am J Perinatol 2012;29:95–100.
Ramanathan R, Bhatia JJ, Sekar K, Ernst FR. Mortality in preterm infants with respiratory distress syndrome treated with poractant alfa, calfactant or beractant: a retrospective study. J Perinatol 2013;33:119–25.
Lampland AL, Wolfson MR, Mazela J, et al. Aerosolized KL4 surfactant improves short-term survival and gas exchange in spontaneously breathing newborn pigs with hydrochloric acid-induced acute lung injury. Pediatr Pulmonol 2014;49:482–9.
Seehase M, Collins JJ, Kuypers E, et al. New surfactant with SP-B and C analogs gives survival benefit after inactivation in preterm lambs. PLoS One 2012;7:e47631.
Pillow JJ, Minocchieri S. Innovation in surfactant therapy II: surfactant administration by aerosolization. Neonatology 2012;101:337–44.
Arzhavitina A, Steckel H. Surface active drugs significantly alter the drug output rate from medical nebulizers. Int J Pharm 2010;384:128–36.
Minocchieri S, Knoch S, Schoel WM, Ochs M, Nelle M. Nebulizing poractant alfa versus conventional instillation: Ultrastructural appearance and preservation of surface activity. Pediatr Pulmonol 2014;49:348–56.
Jobe AH, Moss TJ, Nitsos I, Ikegami M, Kallapur SG, Newnham JP. Betamethasone for lung maturation: testing dose and formulation in fetal sheep. Am J Obstet Gynecol 2007;197:523.e1–6.
Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2006:CD004454.
Fehrholz M, Hütten M, Kramer BW, Speer CP, Kunzmann S. Amplification of steroid-mediated SP-B expression by physiological levels of caffeine. Am J Physiol Lung Cell Mol Physiol 2014;306:L101–9.
Pillow JJ. Tidal volume, recruitment and compliance in HFOV: same principles, different frequency. Eur Respir J 2012;40:291–3.
Mulrooney N, Champion Z, Moss TJ, Nitsos I, Ikegami M, Jobe AH. Surfactant and physiologic responses of preterm lambs to continuous positive airway pressure. Am J Respir Crit Care Med 2005;171:488–93.
Jobe AH, Newnham JP, Willet KE, et al. Endotoxin-induced lung maturation in preterm lambs is not mediated by cortisol. Am J Respir Crit Care Med 2000;162:1656–61.
Mason RJ, Nellenbogen J, Clements JA. Isolation of disaturated phosphatidylcholine with osmium tetroxide. J Lipid Res 1976;17:281–4.
Been JV, Zoer B, Kloosterboer N, et al. Pulmonary vascular endothelial growth factor expression and disaturated phospholipid content in a chicken model of hypoxia-induced fetal growth restriction. Neonatology 2010;97:183–9.
Stewart JC. Colorimetric determination of phospholipids with ammonium ferrothiocyanate. Anal Biochem 1980;104:10–4.
Rahmel DK, Pohlmann G, Iwatschenko P, et al. The non-intubated, spontaneously breathing, continuous positive airway pressure (CPAP) ventilated pre-term lamb: a unique animal model. Reprod Toxicol 2012;34:204–15.
Acknowledgements
The authors thank Nico Kloosterboer for excellent technical assistance and Dennis Kruk, Jennifer Collins and Monique Willems for their valuable support in the experimental handling of the animals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hütten, M., Kuypers, E., Ophelders, D. et al. Nebulization of Poractant alfa via a vibrating membrane nebulizer in spontaneously breathing preterm lambs with binasal continuous positive pressure ventilation. Pediatr Res 78, 664–669 (2015). https://doi.org/10.1038/pr.2015.165
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2015.165
This article is cited by
-
Development of a High-Dose Infant Air-Jet Dry Powder Inhaler (DPI) with Passive Cyclic Loading of the Formulation
Pharmaceutical Research (2022)
-
Does surfactant nebulization prevent early intubation in preterm infants? A protocol for a systematic review and meta-analysis
Systematic Reviews (2021)
-
Aerosol drug delivery to spontaneously-breathing preterm neonates: lessons learned
Respiratory Research (2021)
-
A novel delivery system for supraglottic atomization allows increased lung deposition rates of pulmonary surfactant in newborn piglets
Pediatric Research (2020)
-
Surfactant replacement therapy: from biological basis to current clinical practice
Pediatric Research (2020)