Abstract
Background:
Bilirubin binding capacity (BBC) defines the dynamic relationship between an infant’s level of unbound or “free” bilirubin and his/her ability to “tolerate” increasing bilirubin loads. BBC is not synonymous with albumin (Alb) levels because Alb binding of bilirubin is confounded by a variety of molecular, biologic, and metabolic factors.
Methods:
We utilized a novel modification of a previously developed hematofluorometric method to directly assay BBC in whole blood from preterm and term neonates and then combined these data with an archived database. Total bilirubin (TB) was also measured, and multiple regression modeling was used to determine whether BBC in combination with TB measurements can assess an infant’s risk for developing bilirubin-induced neurotoxicity.
Results:
TB and BBC levels ranged from 0.7–22.8 to 6.3–47.5 mg/dl, respectively. Gestational age (GA) correlated with BBC (r = 0.54; P < 0.0002) with a slope of 0.93 mg/dl/wk by logistic regression. Our calculations demonstrate that recently recommended GA-modulated TB thresholds for phototherapy and exchange transfusion correspond to 45 and 67% saturation of our observed regression line, respectively.
Conclusion:
We speculate that the spread of BBC levels around the regression line (±5.8 mg/dl) suggests that individualized BBC assays would provide a robust approach to gauge risk of bilirubin neurotoxicity compared with TB and GA.
Similar content being viewed by others
Main
Bilirubin binding capacity (BBC) is a determinative measure of a neonate’s ability to cope with an excessive bilirubin load (e.g., due to increased bilirubin production from hemolysis) that may be impacted by a variety of biologic factors, including disordered or insufficient bilirubin binding to albumin (Alb) (1,2). The long-standing belief that total serum/plasma bilirubin (TB), by itself, does not reliably predict an infant’s risk for developing bilirubin-induced neurological dysfunction (BIND) or kernicterus has been recently reconfirmed (2,3,4,5). The traditional reliance on the TB level alone as a clinical measure of both bilirubin exposure and risk for neurotoxicity may result in overuse of phototherapy or delayed phototherapy in cases where exposure risk is underestimated. It is recommended to use risk factors, including prematurity, hemolysis, sepsis, acidosis, and hypoalbuminemia, to modulate assessment of risk of neurotoxicity at TB levels adjusted for age-in-hours (2,6,7,8). However, neither serum Alb levels nor the molar ratio of TB to Alb has been predictive of bilirubin neurotoxicity (4,6,7,8). BBC, when directly measured by various methods, is generally lower than that expected from the Alb level, especially in preterm and sick infants in whom the ratio of capacity to Alb is highly variable (9,10). Thus, the Alb level is only a rough estimate of an infant’s BBC. The neuroprotective role of serum Alb, the bilirubin transport protein, was demonstrated in vitro years ago (11). Seminal demonstration that the antibiotic sulfisoxazole was the cause of acute bilirubin encephalopathy even at low TB values highlighted the insidious effects of compounds that can compete for the primary Alb-binding site for bilirubin and led to the development of assays for measuring reserve albumin binding capacity (RABC) (8,12,13). However, none of these methods for RABC proved amenable for routine clinical use. While an assay of serum/plasma unbound or “free” bilirubin (UB) to predict the risk of BIND has been employed for many years by researchers (8), it generally remains a research tool. The role of UB as a unique clinical biomarker of BIND has not been fully elucidated (2,4,8). However, sufficient bench data has accumulated to suggest that dynamic UB is “buffered” by an infant’s BBC (4). This dynamic relationship between the volatile UB and BBC that fluctuates with increasing bilirubin loads is analogous to rapidly changing carbon dioxide tension that is buffered by serum bicarbonate.
The direct measurement of BBC is feasible and amenable to routine use as has been reported on studies using hematofluorometry (13,14,15,16,17). A hematofluorometric device has been recently modified for bedside, point-of-care application, and we investigated its clinical utility. In addition, we merged data from an archived database collected by the same methodology, from an earlier partially reported study (18), in order to: (i) delineate the relationship between BBC and gestational age (GA); (ii) determine GA-specific normative values for BBC; and (iii) apply the GA-based consensus intervention thresholds for phototherapy and exchange transfusion (7), as per (i), together with TB/BBC and UB-based thresholds as reported from multiple studies over the years, to suggest a novel algorithm for assessing an infant’s risk for developing BIND.
Results
TB, BBC, and UB (calculated) were measured in 480 blood specimens from a total of 331 term and preterm infants, both healthy and sick. Two different versions of the hematofluorometric instrument were used for the three different cohorts and over a 35-y span. The intrinsic simplicity of the method and sample preparation and the identical protocol for calibration of the instruments provided part of the rationale to combine the data.
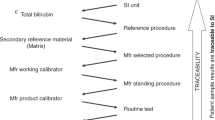
The relationship between BBC and GA (in completed weeks) is shown for the combined dataset in Figure 1 . The slope of the linear regression (r = 0.54) is 0.93 mg/dl/wk. The regression lines for the individual relationships of the three subcohorts, constrained to the same intercept as the regression line for the combined population, have nearly identical slopes (P = 0.52): Cleveland: 0.94 mg/dl/wk; Hangzhou: 0.92 mg/dl/wk; and Stanford: 0.93 mg/dl/wk. On this basis, we rationalized the combining of the data from the three cohorts. While there is no a priori expectation of a linear relation of BBC and GA, no sensible functional fit to the data gives a better correlation coefficient than the linear function. Interpolations of the recent consensus recommendations for threshold values for phototherapy and exchange transfusion as a function of GA (7) fit lines corresponding to 45 and 67% of the BBC vs. GA regression line ( Figure 1 ).
Correlation of bilirubin binding capacity (mg/dl) to gestational age (weeks). The regression line (solid) has a slope of 0.93 mg/dl/wk; r = 0.54; P < 0.001. The dashed and dotted lines, at 67 and 45% of the capacity line, represent best fit lines to the interpolated recommended serum/plasma total bilirubin (TB) threshold values for exchange transfusion and phototherapy (7), respectively. The circles represent data points.
The average BBC values for infants with and without respiratory distress syndrome (RDS) in the Cleveland cohort showed a significant fall (P < 0.002) in the BBC from infants with no RDS (N = 111), 25.5 ± 5.7 mg/dl, to those with mild RDS and treated with supplemental oxygen only (N = 20), 20.8 ± 4.8, and to those with severe RDS needing assisted ventilation (N = 27), 18.3 ± 5.9. However, the average GA also declined with the respiratory status: 34.6, 32.7, and 30.5 wk, respectively, making these BBC values consistent with the BBC vs. GA line of Figure 1 . We also observed that the average BBCs for infants with (N = 24) and without (N = 71) septicemia in the Hangzhou cohort are statistically the same, 27.7 ± 3.7 and 27.1 ± 4.8 mg/dl, respectively.
Alb, BBC, and GA
Serum Alb and GA correlated linearly (r = 0.69; P < 0.002) for the combined cohorts with Alb increasing by 0.11 g/dl/wk. The ratio of BBC to Alb also increased with GA (r = 0.34; slope = 0.11 mg/g/wk). The average BBC/Alb ratios were 7.3 ± 0.9, 7.8 ± 1.0, and 8.1 ± 0.7 mg/g for the Cleveland, Stanford, and Hangzhou cohorts, respectively.
Serial BBC and Age From Birth
BBC data was collected daily for several days for some of the infants in the Cleveland cohort. The average daily BBC for a small subgroup (N = 11) who were not transfused and for whom BBC were assayed from postnatal age 1–7 d was found to vary by <1 mg/dl: 20.9 ± 0.6 mg/dl.
A Novel Display of Binding Parameters
The parameters UB/TB and TB/BBC have been recommended indicators of binding status (see Discussion). Figure 2 shows plots of calculated values of UB/TB vs. TB/BBC (expressed as % saturation, i.e., 100 × (TB/BBC)) for different values of BBC in increments of 5 mg/dl. The values of UB were calculated from values TB and BBC assuming the predominance of the primary Alb-binding site. (For the calculations here, a single value of the Alb–bilirubin association constant of 108 l/mol was used. However, our measured clinical UB/TB ratios (see below) do reflect any difference in the effective binding constant because the value of BBC by hematofluorometry intrinsically reflects the binding constant.)
Calculated ratios of unbound bilirubin (UB, nmol/l)/total bilirubin (TB, mg/dl) as a function of the % saturation of the bilirubin binding capacity (BBC) or TB/BBC for different values of BBC in 5 mg/dl increments, represented by different symbols, from 10 (diamond symbol), 15 (square symbol), 20 (triangle symbol), 25 (multiplication sign), 30 (solid dot), 35 (plus sign), and 40 (minus sign) mg/dl. Calculations are based on the simple binding equation and an association constant of 108 l/mol. The vertical demarcators are at 45 and 67% of saturation, and the horizontal demarcators are at UB/TB = 1.0 and 1.8.
Discussion
Our data reveals a maturational effect on both the Alb level and BBC for each week of GA. The increase in the Alb level of neonates with increasing GA observed in this study confirms two previous reports (9,10). The approximated mean GA-specific BBC in both of those studies are also in quantitative agreement with the observations reported here, e.g., BBC =13.5–17 and 17–22 mg/dl at 26 and 31 wk, respectively. The slopes of the reported regression lines for the otherwise healthy infants, about 1 mg/dl/wk, are about the same as observed here (0.93 mg/dl/wk). While there is no evident a priori reason for a linear relationship between BBC and GA, the linear correlation is high (r = 0.54), consistent with the previous reports. That the correlation is not as good as that of Alb with GA is consistent with the variation observed in the relationship of BBC with Alb. That the BBC/Alb ratio increases with GA (and with birth weight) also confirms previous reports (9,10,15) with the reason for this increase yet unexplained. A low Alb level and a high bilirubin/Alb ratio are recommended risk factors for BIND in recognition that binding status is a concern in the management of newborn jaundice (2,6,7,8). However, the variation in the BBC/Alb among infants has been pointed out as the reason for caution in the use of the Alb level and bilirubin/Alb molar ratio as quantitative indicators of binding status in BIND risk assessment (2,4,6,7,8). Thus, a direct measure of BBC should be advantageous.
Risk of bilirubin neurotoxicity in the preterm infant has been attributed to both GA and concurrent illness. Reasons why prematurity increases risk for BIND include deficient BBC and the possibility that the less mature brain is more susceptible to bilirubin toxicity. In response to the need for more specific guidelines for therapy threshold for preterm infants in the United States, a group of recognized experts provided consensus-based recommendations for thresholds of TB at which phototherapy and exchange transfusion should be considered (7). The recommended threshold values rise linearly with GA at about 1 mg/dl/wk. It is, therefore, of interest that the previously observed linear correlation of BBC with increasing GA (9,10) is confirmed in this study that includes very diverse cohorts. It is of further interest that the increase in BBC with GA (slope of the regression line) is about 1 mg/dl/wk, in concert with both previous observations (9,10) and the consensus recommendations (7). Furthermore, the regression line BBC values at specific GAs are also in good agreement with the previous studies. The consensus-based TB thresholds for phototherapy and exchange transfusion are about 45 and 67%, respectively, of the BBC regression line.
The consistency of the BBC vs. GA data for our three cohorts as well as that from two previous reports (9,10) points to the regression line of Figure 1 as a reasonable, albeit early, definition of the normal values of BBC for GA.
How concurrent illnesses, such as RDS and sepsis, are risk factors for BIND (6,7,8) and how they can measurably increase the risk of bilirubin neurotoxicity has been subjective. It is shown in this study as well as in previous reports that the BBC is lower in sick compared with well babies (9,10). Lower mean BBCs is observed in the Cleveland cohort as the severity of RDS increases. However, the mean GA with increasing degree of RDS also decreases and can account entirely for the decrease in BBC. No significant differences were found in the mean BBC of the mostly term infants with and without sepsis in the Hangzhou cohort.
Assuming the GA-dependent consensus-based TB thresholds for intervention reflect the GA-dependent BBC and that the regression line of Figure 1 represents a reasonable, albeit preliminary, norm, it is instructive to compare the consensus thresholds with previously reported levels of UB indications of risk for BIND and bilirubin encephalopathy. Table 1 lists the values of UB for consideration of exchange transfusion (21 nmol/l) and phototherapy (8 nmol/l) calculated from the (consensus TB)/(regression line BBC), expressed at % saturation of BBC, using the single site binding model and K = 108 l/mol. (This value for K is derived from the slope of the regression line (r = 0.87) of comparisons of UB values of neonate samples using the peroxidase method and hematofluorometry (13,18)). The other UB levels (peroxidase method) and their relations with clinical observations are taken from various reported studies and reviews (19,20,21,22,23). Given the rapid acceleration of the increase of UB as TB approaches BBC (4) and the unknown agreement of the UB assays from different places, times, and infant populations, the uniformity of threshold UB levels in Table 1 is both remarkable and comforting. Taking UB ≥ 20 and TB/BBC ≥ 0.67 as indicative of high risk for BIND and bilirubin encephalopathy is consistent with the expert consensus TB thresholds by GA. While it would seem reasonable to utilize such individualized binding status data as the basis for initiating phototherapy and/or exchange transfusion, substituting such for existing guidelines is not warranted until further prospective studies relating binding status to outcome are performed. As pointed out by McDonagh and Maisels (24), a renewed availability of hematofluorometry should facilitate such studies.
Ahlfors et al. (1,4,20) make the case that the UB/TB ratio, which reflects both the RABC and the binding affinity (UB/TB = 1/(K × RABC), should be a better indicator of risk for BIND than either UB or TB alone because the UB/TB should better reflect the extravascular bilirubin load. The UB/TB ratio is also indicative of the rate of rise of UB for an incremental rise in TB. Furthermore, Ahlfors et al. (1) presents the case that the TB/Alb ratio is better than TB alone as an indicator of risk and further points out that the TB/BBC ratio may be more appropriate since BBC and Alb are very often not equivalent especially in higher risk preterm infants. If it is possible to obtain both the TB and BBC and a calculated UB, as can be done by hematofluorometry, then one might consider expressing binding status based on both the UB/TB and TB/BBC ratios.
Plotting BBC and TB data in this way ( Figure 2 ) provides a comprehensive view of the binding status, clearly showing that the change in UB as the TB rises is a sensitive function of the TB relative to the BBC. For example, for BBC = 10 mg/dl, increasing TB from 5 to 6 mg/dl brings UB from 10 to 15 nmol/l, while for BBC = 30, increasing TB from 15 to 16 mg/dl brings UB from 10 to only 11 nmol/l. While the TB/BBC ratio reflects the fraction of the binding capacity unavailable, UB/TB reflects the absolute value of the reserve capacity. Taken together, these two views of the binding status underscore the key importance of the binding capacity and better reflect the extravascular bilirubin load.
Figure 3 attempts to translate the UB/TB vs. TB/BBC plot to risk categories, with vertical lines placed at the TB/BBC values representing the GA-based consensus thresholds, 45 and 67%. As demarcators for UB/TB, horizontal lines are placed at UB/TB = 1.0 and 1.8, cutoff values reported by Ahlfors et al. (20) for findings of normal and abnormal auditory brainstem response, respectively. It is instructive to view the TB and BBC data for the study cohorts plotted as UB/TB vs. % saturation of binding. By inference, we provide labels denoting risk of BIND for regions of the plot defined by the demarcators discussed above. No outcome data was collected nor was systematic neurological testing, such as hearing or MRI examination, undertaken. We plan such in a follow-up study. More than 70% of the infants in this study eventually received phototherapy. That phototherapy may be significantly overprescribed is indicated by the large fraction of data points in the “Observe” region.
An inferential display of actual study ratios of unbound bilirubin (UB, nmol/l)/total bilirubin (TB, mg/dl) and the % saturation of the bilirubin binding capacity (BBC) or TB/BBC, as displayed in Figure 2 to define theoretical risk of developing bilirubin-induced neurologic dysfunction in this study cohort (see text for details).
Understanding how the relative values of TB, BBC, and UB relate to the extravascular burden of bilirubin, and assuming that the greater risk for BIND in lower GA infants, as expressed in the consensus TB thresholds, is in major part related to lower BBC, it seems clear that having an accurate individualized BBC, in addition to TB, would aid in management decisions for jaundiced newborns. Without the BBC (or a direct measure of UB), it is difficult to adequately interpret, for example, a TB of, say 5 mg/dl, in a preterm neonate. That the BBC appears to be reasonably constant over the first week after birth (average expected rise of 1 mg/dl) further suggests that BBC can be used as an adjunct to guide clinical management. A major obstacle in preventing such use of binding data has been the lack of available and practical methodologies. Hematofluorometry may offer a solution since it provides TB, BBC, and a calculated UB, is exceptionally simple to use, requires no special reagents, uses <100 µl of blood, and does not require separation of serum and red blood cells. The methodology should be amenable to point-of-care use.
Methods
This prospective observational multicenter study was conducted in the Newborn Nurseries of the Lucile Packard Children’s Hospital (Stanford, CA) and The Children’s Hospital of Zhejiang University School of Medicine (Hangzhou, China). In addition, these data were supplemented with unpublished archived data collected as an earlier observational research study. All infants were eligible for enrollment if they were managed exclusively in the neonatal intensive care unit after informed parental consent. The Institutional Research Review Boards from all institutions approved the clinical protocol.
Subjects and Patient Population
The current prospective study at Lucile Packard Children’s Hospital at Stanford University enrolled 80 neonates who were born at or transferred to Stanford during 2012 to 2013. The term and preterm cohorts were enrolled randomly from hospitalized neonates following parental consent for collection of an additional 100 µl of blood (separate heparinized tube) at the time blood was drawn (heel stick) for routine bilirubin testing. Ninety-three term or near-term neonates that were transferred to or admitted to The Children’s Hospital of Zhejiang University School of Medicine (Hangzhou, China) were also enrolled. A portion (200 µl) of the blood drawn by venipuncture as a routine practice at admission was transferred to a heparinized tube. The archived data was obtained with consent of the study’s Principal Investigator, Dr Avroy A. Fanaroff, at the Rainbow Babies and Children’s Hospital, Case Western Reserve University (Cleveland, OH). As part of routine bilirubin testing, heparinized whole blood specimens were drawn by heel stick or via umbilical catheter from 158 randomly identified infants during 1978 to 1979 (18).
The population included both term and preterm infants. The clinical status of the babies varied from otherwise healthy babies with jaundice to preterm infants with RDS. Infants with direct bilirubin values >1.5 mg/dl were excluded. A total 307 blood samples were obtained and tested by hematofluorometer assays. Clinical data was compiled from hospital records and were stored as paper research records. This database was converted to electronic records for this study and re-evaluated for complete and validated entries. Table 2 lists the demographics and a selection of patient characteristics.
BBC Determinations
Hematofluorometric assay of BBC relies on the physical property of bilirubin to fluoresce when it is bound to its primary site on Alb (17). It has been well demonstrated that addition of sufficient bilirubin, in a readily soluble form, to a blood sample produces a fluorescence signal indicative of the true BBC (13,15,16,18). Fluorescence from a blood sample without added bilirubin is indicative of the already present bilirubin bound to Alb (or TB). Hematofluorometry is “front-face” fluorometry required by the extreme absorbance of whole blood. The advantage of this method is that the sample, as a drop atop a glass slide, only needs to be thick enough to absorb all the exciting light and therefore independent of its volume. Thus, to have sufficient thickness of ~20 µm, only 20 µl of blood is required. The hematocrit or Hb content of the sample is measured in order to correct for the fluorescence intensity and to reference the TB and BBC values to the plasma volume.
The hematofluorometer is equipped with a stable internal fluorescence standard that maintains calibration. The hematofluorometers used at Stanford and Hangzhou were supplied by Aviv Biomedical (Lakewood NJ). The hematofluorometer used at Cleveland was provided by Bell Labs (Murray Hill, NJ). Instruments were calibrated using bilirubin-laden adult blood and employed the identical stable internal fluorescent reference material.
Hb and Serum Alb Determinations
Hematocrits for samples at Rainbow Babies Hospital were determined by centrifugation of blood in microhematocrit tubes. At both Stanford and Hangzhou, Hb was determined using a Hemocue 201+ Analyzer (Angelhohm, Sweden). At all three centers, serum Alb levels were determined using the standard bromocresol green colorimetric assay (25).
UB Calculation
UB was calculated from hematofluorometer BBC and TB values using the law of mass action, UB = TB/(K × RABC), where K is the binding constant and RABC is the binding reserve (BBC − TB) (4,13,14). UB calculated from hematofluorometry data has been shown previously (13,16) to track extremely well with UB determined using the peroxidase method. The value of K that coincides the two methods is between 0.7 × 108 and 1 × 108 l/mol.
Statistical Analyses
t-Tests, ANOVAs, and standard regression analyses were performed using Excel and deemed significant when P ≤ 0.05.
Statement of Financial Support
This study was supported by the US National Institutes of Health SBIR 5R44EB015924-03, the Kaplan-Goldstein Family Foundation (USA), the Mary L. Johnson Research Fund (USA), and the Christopher Hess Research Fund (USA). No commercial financial assistance was received in support of this study.
Disclosure
None of the authors have any financial interests to disclose.
References
Ahlfors CE . Criteria for exchange transfusion in jaundiced newborns. Pediatrics 1994;93:488–94.
Watchko JF, Tiribelli C . Bilirubin-induced neurologic damage–mechanisms and management approaches. N Engl J Med 2013;369:2021–30.
Ahlfors CE . Predicting bilirubin neurotoxicity in jaundiced newborns. Curr Opin Pediatr 2010;22:129–33.
Ahlfors CE, Wennberg RP, Ostrow JD, Tiribelli C . Unbound (free) bilirubin: improving the paradigm for evaluating neonatal jaundice. Clin Chem 2009;55:1288–99.
Gamaleldin R, Iskander I, Seoud I, et al. Risk factors for neurotoxicity in newborns with severe neonatal hyperbilirubinemia. Pediatrics 2011;128:e925–31.
American Academy of Pediatrics. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114:297–316.
Maisels MJ, Watchko JF, Bhutani VK, Stevenson DK . An approach to the management of hyperbilirubinemia in the preterm infant less than 35 weeks of gestation. J Perinatol 2012;32:660–4.
Wennberg RP, Ahlfors CE, Bhutani VK, Johnson LH, Shapiro SM . Toward understanding kernicterus: a challenge to improve the management of jaundiced newborns. Pediatrics 2006;117:474–85.
Bender GJ, Cashore WJ, Oh W . Ontogeny of bilirubin-binding capacity and the effect of clinical status in premature infants born at less than 1300 grams. Pediatrics 2007;120:1067–73.
Cashore WJ, Horwich A, Karotkin EH, Oh W . Influence of gestational age and clinical status on bilirubin-binding capacity in newborn infants. Sephadex G-25 gel filtration technique. Am J Dis Child 1977;131:898–901.
Odell GB . Influence of binding on the toxicity of bilirubin. Ann NY Acad Sci 1973;226:225–37.
Harris RC, Lucey JF, Maclean JR . Kernicterus in premature infants associated with low concentrations of bilirubin in the plasma. Pediatrics 1958;21:875–84.
Wells R, Hammond K, Lamola AA, Blumberg WE . Relationships of bilirubin binding parameters. Clin Chem 1982;28:432–9.
Amin SB, Lamola AA . Newborn jaundice technologies: unbound bilirubin and bilirubin binding capacity in neonates. Semin Perinatol 2011;35:134–40.
Brown AK, Eisinger J, Blumberg WE, Flores J, Boyle G, Lamola AA . A rapid fluorometric method for determining bilirubin levels and binding in the blood of neonates: comparisons with a diazo method and with 2-(4’-hydroxybenzene)azobenzoic acid dye binding. Pediatrics 1980;65:767–76.
Cashore WJ, Oh W, Blumberg WE, Eisinger J, Lamola AA . Rapid fluorometric assay of bilirubin and bilirubin binding capacity in blood of jaundiced neonates: comparisons with other methods. Pediatrics 1980;66:411–6.
Lamola AA, Eisinger J, Blumberg WE, Patel SC, Flores J . Flurorometric study of the partition of bilirubin among blood components: basis for rapid microassays of bilirubin and bilirubin binding capacity in whole blood. Anal Biochem 1979;100:25–42.
Lamola AA, Fanaroff AA . Bilirubin fluorescence and prevention of kernicterus. Diagn Med 1984;7:9–12.
Ahlfors CE . Unbound bilirubin associated with kernicterus: a historical approach. J Pediatr 2000;137:540–4.
Ahlfors CE, Amin SB, Parker AE . Unbound bilirubin predicts abnormal automated auditory brainstem response in a diverse newborn population. J Perinatol 2009;29:305–9.
Amin SB, Ahlfors C, Orlando MS, Dalzell LE, Merle KS, Guillet R . Bilirubin and serial auditory brainstem responses in premature infants. Pediatrics 2001;107:664–70.
Funato M, Tamai H, Shimada S, Nakamura H . Vigintiphobia, unbound bilirubin, and auditory brainstem responses. Pediatrics 1994;93:50–3.
Nakamura H, Takada S, Shimabuku R, Matsuo M, Matsuo T, Negishi H . Auditory nerve and brainstem responses in newborn infants with hyperbilirubinemia. Pediatrics 1985;75:703–8.
McDonagh AF, Maisels MJ . Bilirubin unbound: déjà vu all over again? Pediatrics 2006;117:523–5.
Doumas BT, Watson WA, Biggs HG . Albumin standards and the measurement of serum albumin with bromcresol green. Clin Chim Acta 1971;31:87–96.
Cashore WJ, Oh W . Unbound bilirubin and kernicterus in low-birth-weight infants. Pediatrics 1982;69:481–5.
Ritter DA, Kenny JD, Norton HJ, Rudolph AJ . A prospective study of free bilirubin and other risk factors in the development of kernicterus in premature infants. Pediatrics 1982;69:260–6.
Acknowledgements
Aviv Biomedical, Inc, Lakewood, NJ, supplied the point-of-care hematofluorometers. We thank Avroy A. Fanaroff for sharing the 1978 Cleveland data and Shanmukha Srinivas for his help in consenting patients at Stanford University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lamola, A., Bhutani, V., Du, L. et al. Neonatal bilirubin binding capacity discerns risk of neurological dysfunction. Pediatr Res 77, 334–339 (2015). https://doi.org/10.1038/pr.2014.191
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2014.191
This article is cited by
-
A multi-center evaluation of a device for measurement of bilirubin binding capacity in neonates: the effects of gestational age, Intralipid exposure and illness severity
Journal of Perinatology (2019)
-
Bilirubin binding in jaundiced newborns: from bench to bedside?
Pediatric Research (2018)