Abstract
Background:
Beckwith–Wiedemann syndrome (BWS) and hemihyperplasia (HH) are overgrowth conditions with predisposition to hepatoblastoma for which early diagnosis patients undergo cancer screening based on determination of the tumor marker α-fetoprotein (αFP). Repeated blood draws are a burden for patients with consequent compliance issues and poor adherence to surveillance protocol. We sought to analyze feasibility and reliability of αFP dosage using an analytical micromethod based on blood dried on filter paper (DBS).
Methods:
Overall 143 coupled αFP determinations on plasma and DBS collected simultaneously were performed, of which 31 were in patients with hepatoblastoma predisposition syndromes and 112 were in controls. The plasma αFP dosage method was adapted to DBS adsorbed on paper matrix for newborn screening.
Results:
There was strong correlation between plasmatic and DBS αFP (r2 = 0.999, P < 0.001). Cohen’s k coefficient for correlation was 0.96 for diagnostic cut-off of 10 U/ml (P < 0.001), commonly employed in clinical practice. The measurements on plasma and DBS were highly overlapping and consistent.
Conclusion:
The DBS method allowed to dose αFP reliably and consistently for the concentrations commonly employed in clinical settings for the screening of hepatoblastoma, opening new scenarios about conducting cancer screening in overgrowth syndromes.
Similar content being viewed by others
Main
Beckwith–Wiedemann syndrome (BWS, OMIM 130650) is the most common overgrowth disorder, with an estimated prevalence of 1:10,500 live births (1). Besides neonatal macrosomia, BWS is characterized by several malformations (abdominal wall defects, macroglossia, renal anomalies, organomegaly, hemihyperplasia (HH), and hyperinsulinemia) and embryonal tumors predisposition (2,3) caused by abnormal methylation of two imprinting centers on chromosome 11p15.5 (2,3,4,5). Isolated HH (OMIM 235000) is considered the mild end of BWS as it displays the same epigenetic anomalies (6,7) and entails the same oncologic risk. Hepatoblastoma is one of the commonest embryonal tumor developing in BWS/HH, occurring in 1.1–2.7% of cases (6,8,9,10). BWS/HH are perhaps the most relevant risk factors for hepatoblastoma as the relative risk among BWS children is 2,280 times that of the healthy population (9,11). Hepatoblastoma is typical of the first 5 y of age and secretes the serum tumor marker α-fetoprotein (αFP) in more than 95% of cases (10,12,13). αFP is a globulin produced during pregnancy by the yolk sac and fetal hepatocytes. The latter, which decrease in number during the first months of life, also sustain its transient production during the early postnatal period. αFP serum concentration reaches a peak of 3,000,000 U/ml at 14 wk of gestation and then declines exponentially, reaching a stable plasmatic concentration <10 U/ml by the age of 8–12 mo (14). Increased plasma αFP is encountered in a variety of physiologic and pathologic conditions and is employed in clinical practice for the diagnosis and follow-up of several tumors (15), besides hepatoblastoma.
As the survival of patients with hepatoblastoma is highly dependent on its early detection and treatment (10,13,16,17), BWS/HH patients are advised to periodically undergo abdominal ultrasonographies and plasma αFP determinations at 2–3-mo time intervals from birth to the first 5 y of age (6,17,18). Evidence suggests that BWS/HH patients would benefit from even closer αFP measurements because hepatoblastoma usually grows rapidly (17). This issue is particularly relevant in a subset of high-risk patients (19,20) such as those with severe phenotypes, HH, and organ enlargement (2,3,21,22,23). However, the psychological burden of the closely repeated blood draws can reduce the compliance and complicate the follow-up (6).
This preliminary report explores the feasibility and assesses the reliability of a screening program for hepatoblastoma based on αFP determination on dried capillary blood spot (DBS) in patients with BWS/HH.
Results
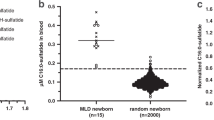
A correlation was present between αFP measurements on plasma and DBS at linear regression (r2 = 0.999, P < 0.001, Figure 1 ). Results using the two methods were highly consistent and overlapped across the wide range of αFP concentrations (0.3 to 97,198.0 U/ml in plasma and from 0.1 to 97,889.0 U/ml on DBS) depending on the age of patients. Two cases displayed αFP > 10 U/ml after 12th month of life: a 16 mo old control female with a αFP of 11.3 U/ml on plasma and 7.6 U/ml on DBS (1 mo later recheck: 7.9 U/ml on plasma) and a 14 mo old BWS female with αFP concentrations of 16.4 U/ml on plasma and 12.4 U/ml on DBS (subsequent recheck 2 mo later: 11.2 U/ml on plasma). Both plasmatic and DBS αFP measurements were consistent with the plasmatic αFP reference values provided by Blohm et al. ( Figure 2 ): clearly, patients with BWS/HH tended to have elevated αFP concentrations or in the upper part of the reference range displaying a slower decrease in αFP concentrations during the first months of life when compared to controls (15,24,25).
Correlation between α-fetoprotein (αFP) concentrations measured with the same kit on plasma and dried blood spot (DBS). The gray-shaded area represents normal αFP concentrations in children aged >2 y and adults (10 U/ml).
α-Fetoprotein (αFP) trajectory during the first year of life during which it physiologically decreases from 105 to 10 U/ml, measured in both plasma (triangles, panel a) and dried blood spot (circles, panel b). The gray-shaded area represents the αFP reference values according to Blohm et al. (25). Filled symbols refer to affected patients; empty symbols refer to controls. Note the high degree of overlap between plasmatic and dried blood spot determinations.
With a αFP threshold of >10 U/ml, agreement between the two methods was 141/143 (98.6%) with 110 measurements <10 U/ml and 31 >10 U/ml: Cohen’s k was 0.96, standard error 0.028 (95% CI: 0.90–1.01). In two cases, αFP was >10 U/ml in plasma (10.7 and 11.3 U/ml) and <10 U/ml on DBS (4.1 and 7.6 U/ml). There were no cases with αFP DBS measurement >10 U/ml and <10 U/ml on plasma.
The Bland–Altman plot analyzes the correlation between the two different assays for αFP measurement. The absolute difference between the two measurements is plotted against their average across the wide range of αFP concentrations (represented in five separate scales for power-10 magnitudes in Figure 3 ). Overall, the mean of the difference in individual values obtained by the two methods (▵) was −0.8 ± 86.0 (median: −1.40, range from −599.0 to 689.0). The inspection of the Bland-Altman scatter-plot (▵ plotted against the average between plasma and DBS measurements) revealed a systematic proportional positive bias in the DBS assay compared to plasma measurement with a loose upward slope of the regression line (▵ = 0.0065 × average−6.24, r2 = 0.388, P < 0.001). The bias was absent for αFP values <100 U/ml (r2 = 0.03, p = not significant).
The Bland–Altman plot analyzes the agreement between the two different assays for α-fetoprotein (αFP) measurement: the absolute difference between the two measurements is plotted against their average all across the wide range of αFP concentrations represented in five separate scales of αFP concentration for graphical reasons: a) αFP from 0 to 10 U/ml; b) from 10 to 100 U/ml; c) from 100 to 1,000 U/ml; d) from 1,000 U/ml to 10,000 U/ml; e) >10,000 U/ml. There was a systematic proportional positive bias in the dried blood spot (DBS) assay compared to plasma measurement. The bias was absent for αFP values <100 U/ml. In the panel, the maximum absolute and percent differences between αFP on DBS and plasma (▵) are reported.
Discussion
Given the considerable burden of repeated and frequent blood draws for hepatoblastoma screening in children with cancer predisposition syndromes, we sought to study the feasibility of employing a DBS-based technique for plasmatic αFP measurement. This approach has already been attempted in other situations: as a second tier test for tyrosinemia newborn screening (26), as a screening for fetal neural tube defects and trisomy 21 in pregnancy (27,28,29), and for liver adenocarcinoma mass screening in adults (30). In this study, we adapted the method for αFP plasmatic measurement to blood dried on standard newborn screening filter paper and studied its reliability by comparing it with the traditional method, in both blood of patients with hepatoblastoma predisposition syndromes and controls.
Our results provide strong support to the feasibility of hepatoblastoma screening programs based on DBS, with a performance comparable to that using the plasmatic measurement. In the pediatric setting, the interpretation of αFP is complicated by the wide range and rapid variation of the physiologic plasmatic concentration in the first year of life (31,32), by physiologically higher levels in the preterm baby (14), and by the constitutionally higher and slowly decreasing concentrations in BWS/HH (33). Also, in our determinations, BWS/HH cases have constitutively higher levels of αFP, confirming what already observed on plasmatic determinations (33). Most importantly, the proposed method was suitable for the age range considered, making it applicable in both newborns and children, despite the huge physiologic fluctuations of αFP concentrations ranging from a magnitude of 105 U/ml in the newborn to <10 U/ml after the first year of age. This appears crucial given that hepatoblastoma onset likelihood is maximum in the first year of life and progressively decreases until 5 y of age.
The employment of a cut-off of >10 U/ml after 12 mo of age is used to identify as “positive” the determination and proceed with subsequent second-step medical investigations (very close recheck, abdominal ultrasound, and computed tomography). On the other hand, given the wide normality range of the αFP during the first year of life, the surveillance of patients in this age range is mostly based on the determination of consecutive αFP measurements, considered normal if progressively declining. Therefore, the differences between plasmatic and DBS values we observed likely have little impact since αFP initially decreases with an approximate 10-fold magnitude every month in the first semester. Even taking into account the largest variation we observed in our series between the gold standard and the DBS method, none of the cases of hepatoblastoma in BWS/HH documented in literature (17,19) would have been missed employing the DBS method.
The precision and simplicity of this method makes the routine measurement of αFP more practical. Blood sample collection by heel stick suffices for this simple, efficient, and low-cost determination of αFP concentration. The advantages of DBS collected on filter paper over serum samples obtained by venipuncture mostly consist in an easier and less invasive specimen collection, increased efficiency and low-cost. These aspects are crucial to warrant patients’ and parents’ compliance to the tumor surveillance program and possibly allow a closer follow-up schedule. Likely, these results may allow an increase in compliance to the tumor surveillance programs considerably reducing the psychological and practical burden of repeated blood drawn which may be well substituted by blood sample collection by heel stick—perhaps easily collectable also at home—with consequent direct and indirect costs reduction. Most importantly, the DBS method allows closer (and presumably more effective) determinations of αFP in patients with very high risk for hepatoblastoma. The current hepatoblastoma surveillance program in these syndromes relies on a 2–3 mo plasmatic αFP determination which is an acceptable schedule to allow early diagnosis of hepatoblastoma. Presumably, some of these rapidly growing neoplasms will be detected earlier with closer αFP measurements, especially in the subset of patients with genetic or phenotypic characteristics associated with very high risk for tumor development (17,19,20). As observed in adults, screening for hepatocarcinoma cirrhotic patients by serum αFP measurement resulted in increased survival rates (34). Moreover, the constant monthly rise in serum αFP was a more sensitive marker that transversal determinations with cut-offs, usually performed every 3–6 mo (35). Presumably, this also applies to the BWS/HH-related hepatoblastoma setting. An additional advantage of αFP determination on DBS is that samples can be rechecked on the same filter paper when necessary (i.e., in case of slight elevations in αFP levels, which is a frequent clinical situation in the follow-up of patients with cancer predisposition syndromes). Obviously, tumor surveillance can give false-positive results leading to unnecessary interventions and investigations (36). A close repeat in αFP measurement on DBS may be less invasive for patients and more cost-effective for health-care system. Finally, DBS test could be performed at home and the card posted to the laboratory in a suitable envelope, further reducing the overall costs at all levels.
Further efforts are necessary before introducing the DBS method in clinical practice. First, further studies are needed for the assessment of the consistency of the method in the longitudinal observation of patients. Second, the creation of appropriate reference values for all the ages for the DBS method is necessary, possibly taking into account a correction for gestational ages as many of the overgrowth syndromes give rise to pregnancy complications resulting in prematurity. Finally, the method should be validated for tumor recognition, and precise sensitivity and specificity should be calculated. Other potential relevant applications of the method are scattered all over several pediatric situations: the screening and follow-up of other conditions with increased risk of hepatocarcinoma (13) or other αFP-secreting tumors or genetic conditions with raised αFP, and the follow-up of patients treated or under-treatment for hepatoblastoma. This study opens new perspectives on the modalities of the cancer screening procedures employed in the follow-up of overgrowth-cancer predisposition syndromes in pediatric genetics.
Methods
Contemporaneous plasmatic and DBS αFP determinations were performed in 143 children born from at-term pregnancies (mean age: 5.6 ± 5.4 y, range: 0.1–16.1, 72 males). Of these, 31 had syndromes with increased risk of hepatoblastoma under cancer screening: 21 were affected by BWS, 8 by HH, and 2 had macrocephaly-capillary malformation syndrome, an overlapping overgrowth-cancer predisposition condition. A hundred and twelve children served as controls: 27 were healthy children, the remaining underwent blood tests for suspected conditions known to have no effect on plasmatic αFP concentration (25 suspected or well compensated thyroid disorders, 36 with recently healed infection, 16 serum lipids screening, 15 phenylketonuria, 11 suspected iron deficient anemia, 7 suspected precocious puberty). In all cases, the suspected diagnosis was excluded after the tests. Informed consent was obtained from parents and the study was approved by the Institutional Review Board of the University of Torino (Italy).
A serum tube was filled with blood obtained by venipuncture and simultaneously a DBS was collected by heel-stick or by spotting single blood drops from a syringe directly onto standard filter paper employed for neonatal mass screening. The DBS specimens were dried at room temperature and routinely stored in plastic bags at 4 °C.
The serum αFP measurement kit (AutoDELFIA hAFP, Perkin Elmer, Waltham, MA) was adapted to the DBS-based technique through a calibration curve obtained from the addition of red blood cells to the kit internal standard solutions and subsequent spotting on standard neonatal mass screening filter paper. αFP measurement was performed employing a 3 mm-diameter spotted filter paper punch containing ~1.3 μl of adsorbed blood then eluted at room temperature for 1 h at high speed and half an hour at low speed with 200 μl of Tris-HCl pH 7.8 buffer supplied with the kit. The DBS and the buffer were removed with the aid of a vacuum pump, then processed according to the instructions. The reaction was determined by fluorometric quantification by a fluorometer reading retarded Europium fluorescence (VICTOR X or EnVision Multilabel Plate Reader, PerkinElmer).
Data were archived and analyzed with SPSS 5.0 (IBM, Armonk, NY) and GraphPad Prism 5.0 (GraphPad Software, La Jolla, CA). Discrete quantitative data were recorded as the mean ± SD and analyzed for normal distribution with the Shapiro–Wilk test. Correlations were tested with the Pearson or Sperman methods, for parametric and nonparametric variables, respectively. The agreement between the two tests was assessed taking into account the concordance occurring by chance by employing Cohen’s kappa (k) coefficient and considering the αFP threshold of >10 U/ml, as commonly employed in clinical practice (6,23). The results of the DBS and the plasmatic methods for αFP measurement were further validated by the Bland–Altman plot statistical approach.
Statement of Financial Support
The study was supported by the grant sponsor by MIUR (Italian Ministry for Education, University and Research) PRIN 2009-MBHZPR to G.B.F.
Disclosure
The authors declare no conflict of interest.
References
Mussa A, Russo S, De Crescenzo A, et al. Prevalence of Beckwith-Wiedemann syndrome in North West of Italy. Am J Med Genet A 2013;161:2481–6.
Choufani S, Shuman C, Weksberg R . Beckwith-Wiedemann syndrome. Am J Med Genet C Semin Med Genet 2010;154C:343–54.
Shuman C, Beckwith JB, Smith AC, Weksberg R . Beckwith-Wiedemann syndrome. In: Pagon RA et al (eds.). GeneReviews. Seattle, WA: University of Washington, 1993–2013:2000.
Riccio A, Sparago A, Verde G, et al. Inherited and Sporadic Epimutations at the IGF2-H19 locus in Beckwith-Wiedemann syndrome and Wilms’ tumor. Endocr Dev 2009;14:1–9.
Chiesa N, De Crescenzo A, Mishra K, et al. The KCNQ1OT1 imprinting control region and non-coding RNA: new properties derived from the study of Beckwith-Wiedemann syndrome and Silver-Russell syndrome cases. Hum Mol Genet 2012;21:10–25.
Zarate YA, Mena R, Martin LJ, Steele P, Tinkle BT, Hopkin RJ . Experience with hemihyperplasia and Beckwith-Wiedemann syndrome surveillance protocol. Am J Med Genet A 2009;149A:1691–7.
Bliek J, Maas S, Alders M, Merks JH, Mannens M . Epigenotype, phenotype, and tumors in patients with isolated hemihyperplasia. J Pediatr 2008;153:95–100.
Rump P, Zeegers MP, van Essen AJ . Tumor risk in Beckwith-Wiedemann syndrome: A review and meta-analysis. Am J Med Genet A 2005;136:95–104.
DeBaun MR, Tucker MA . Risk of cancer during the first four years of life in children from The Beckwith-Wiedemann Syndrome Registry. J Pediatr 1998;132(3 Pt 1):398–400.
Rougemont AL, McLin VA, Toso C, Wildhaber BE . Adult hepatoblastoma: learning from children. J Hepatol 2012;56:1392–403.
Spector LG, Birch J . The epidemiology of hepatoblastoma. Pediatr Blood Cancer 2012;59:776–9.
Herzog CE, Andrassy RJ, Eftekhari F . Childhood cancers: hepatoblastoma. Oncologist 2000;5:445–53.
Litten JB, Tomlinson GE . Liver tumors in children. Oncologist 2008;13:812–20.
Blair JI, Carachi R, Gupta R, Sim FG, McAllister EJ, Weston R . Plasma alpha fetoprotein reference ranges in infancy: effect of prematurity. Arch Dis Child 1987;62:362–9.
Schneider DT, Calaminus G, Göbel U . Diagnostic value of alpha 1-fetoprotein and beta-human chorionic gonadotropin in infancy and childhood. Pediatr Hematol Oncol 2001;18:11–26.
Emre S, Umman V, Rodriguez-Davalos M . Current concepts in pediatric liver tumors. Pediatr Transplant 2012;16:549–63.
Clericuzio CL, Chen E, McNeil DE, et al. Serum alpha-fetoprotein screening for hepatoblastoma in children with Beckwith-Wiedemann syndrome or isolated hemihyperplasia. J Pediatr 2003;143:270–2.
Lapunzina P . Risk of tumorigenesis in overgrowth syndromes: a comprehensive review. Am J Med Genet C Semin Med Genet 2005;137C:53–71.
Mussa A, Ferrero GB, Ceoloni B, et al. Neonatal hepatoblastoma in a newborn with severe phenotype of Beckwith-Wiedemann syndrome. Eur J Pediatr 2011;170:1407–11.
Smith AC, Shuman C, Chitayat D, et al. Severe presentation of Beckwith-Wiedemann syndrome associated with high levels of constitutional paternal uniparental disomy for chromosome 11p15. Am J Med Genet A 2007;143A:3010–5.
Mussa A, Peruzzi L, Chiesa N, et al. Nephrological findings and genotype-phenotype correlation in Beckwith-Wiedemann syndrome. Pediatr Nephrol 2012;27:397–406.
Goldman M, Smith A, Shuman C, et al. Renal abnormalities in beckwith-wiedemann syndrome are associated with 11p15.5 uniparental disomy. J Am Soc Nephrol 2002;13:2077–84.
Hamada Y, Takada K, Fukunaga S, Hioki K . Hepatoblastoma associated with Beckwith-Wiedemann syndrome and hemihypertrophy. Pediatr Surg Int 2003;19:112–4.
Corapçıoğlu F, Türker G, Aydoğan A, Sarper N, Duman C, Arısoy AE . Serum alpha fetoprotein levels in healthy full-term neonates and infants. Marmara Med J 2004;17:1–7.
Blohm ME, Vesterling-Hörner D, Calaminus G, Göbel U . Alpha 1-fetoprotein (AFP) reference values in infants up to 2 years of age. Pediatr Hematol Oncol 1998;15:135–42.
Grenier A, Bélanger L, Laberge C . alpha1-Fetoprotein measurement in blood spotted on paper: discriminating test for hereditary tyrosinemia in neonatal mass screening. Clin Chem 1976;22:1001–4.
Vieira Neto E, Carvalho EC, Fonseca A . Adaptation of alpha-fetoprotein and intact human chorionic gonadotropin fluoroimmunometric assays to dried blood spots. Clin Chim Acta 2005;360:151–9.
Macri JN, Anderson RW, Krantz DA, Larsen JW, Buchanan PD . Prenatal maternal dried blood screening with alpha-fetoprotein and free beta-human chorionic gonadotropin for open neural tube defect and Down syndrome. Am J Obstet Gynecol 1996;174:566–72.
Wong PY, Mee AV, Doran TA . Studies of an alpha-fetoprotein assay using dry blood-spot samples to be used for the detection of fetal neural tube defects. Clin Biochem 1982;15:170–2.
Wu JC, Lee SD, Hsiao KJ, et al. Mass screening of primary hepatocellular carcinoma by alpha-fetoprotein in a rural area of Taiwan–a dried blood spot method. Liver 1988;8:100–4.
Mizejewski GJ, Bellisario R, Beblowski DW, Carter TP . Commercial radioimmunoassay kit for measurement of alpha-fetoprotein adapted for use with dried blood specimens from newborns. Clin Chem 1982;28:1207–10.
Mizejewski GJ, Carter TP, Beblowski DW, Bellisario R . Measurement of serum alpha-fetoprotein in early infancy: utilization of dried blood specimens. Pediatr Res 1983;17:47–50.
Everman DB, Shuman C, Dzolganovski B, O’riordan MA, Weksberg R, Robin NH . Serum alpha-fetoprotein levels in Beckwith-Wiedemann syndrome. J Pediatr 2000;137:123–7.
El-Serag HB, Kramer JR, Chen GJ, Duan Z, Richardson PA, Davila JA . Effectiveness of AFP and ultrasound tests on hepatocellular carcinoma mortality in HCV-infected patients in the USA. Gut 2011;60:992–7.
Arrieta O, Cacho B, Morales-Espinosa D, Ruelas-Villavicencio A, Flores-Estrada D, Hernández-Pedro N . The progressive elevation of alpha fetoprotein for the diagnosis of hepatocellular carcinoma in patients with liver cirrhosis. BMC Cancer 2007;7:28.
Tan TY, Amor DJ . Tumour surveillance in Beckwith-Wiedemann syndrome and hemihyperplasia: a critical review of the evidence and suggested guidelines for local practice. J Paediatr Child Health 2006;42:486–90.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mussa, A., Pagliardini, S., Pagliardini, V. et al. α-Fetoprotein assay on dried blood spot for hepatoblastoma screening in children with overgrowth-cancer predisposition syndromes. Pediatr Res 76, 544–548 (2014). https://doi.org/10.1038/pr.2014.126
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2014.126
This article is cited by
-
Tumor Screening in Beckwith‐Wiedemann Syndrome: Parental Perspectives
Journal of Genetic Counseling (2018)
-
Clinical and molecular diagnosis, screening and management of Beckwith–Wiedemann syndrome: an international consensus statement
Nature Reviews Endocrinology (2018)
-
(Epi)genotype–phenotype correlations in Beckwith–Wiedemann syndrome
European Journal of Human Genetics (2016)