Abstract
Background:
Sustained inflation (SI) at birth facilitates establishment of functional residual capacity (FRC) in the preterm lung, but the ideal lung recruitment strategy is unclear. We have compared the effect of SI and a stepwise positive end-expiratory pressure (PEEP; SEP) strategy in a preterm model.
Methods:
127 d gestation lambs received either 20-s SI (n = 9) or 2 cmH2O stepwise PEEP increases to 20 cmH2O every 10 inflations, and then decreases to 6 cmH2O (n = 10). Ventilation continued for 70 min, with surfactant administered at 10 min. Alveolar–arterial oxygen gradient (AaDO2), compliance (Cdyn), end-expiratory thoracic volume (EEVRIP; respiratory inductive plethysmography), and EEV and Cdyn in the gravity-dependent and nondependent hemithoraces (electrical impedance tomography) were measured throughout. Early mRNA markers of lung injury were analyzed using quantitative real-time PCR.
Results:
From 15 min of life, AaDO2 was lower in SEP group (P < 0.005; two-way ANOVA). SEP resulted in higher and more homogeneous Cdyn (P < 0.0001). Mean (SD) EEVRIP at 5 min was 18 (9) ml/kg and 6 (5) ml/kg following SEP and SI, respectively (P = 0.021; Bonferroni posttest); this difference was due to a greater nondependent hemithorax EEV. There was no difference in markers of lung injury.
Conclusion:
An SEP at birth improved gas exchange, lung mechanics, and EEV, without increasing lung injury, compared to the SI strategy used.
Similar content being viewed by others
Main
The respiratory transition from fetal to ex utero life involves rapidly aerating the fluid-filled lung to establish a functional residual capacity (FRC) (1). In premature infants, this process often requires augmentation with positive pressure ventilation (PPV). How best to apply respiratory support at birth in this population vulnerable to lung and brain injury is unclear and complicated by the rapid changes in lung mechanics during respiratory transition. The initial movement of the air/liquid interface requires a relatively long respiratory system time constant. Once aeration is established, the low compliance state of the surfactant-deficient premature lung results in short time constants.
The role of positive end-expiratory pressure (PEEP) during resuscitation at birth is well established (2,3,4) and advocated in international resuscitation guidelines (5). If applied adequately, PEEP maintains FRC and reduces lung injury caused by atelectasis (4). More recently, a sustained inflation (SI) at birth, to accommodate the long time constants during liquid to air transition, has been advocated as a strategy for augmenting aeration and FRC (2,6,7) and improving pulmonary and cerebral blood flow (8). In premature rabbits, a SI of 20 s followed by PPV with PEEP improved FRC (6) compared to PEEP or SI alone. The characteristics of an optimal SI remain unclear. Both pressure and application time influence subsequent aeration during a SI (6,9). An inadequate inflating pressure or duration will not aerate the lung (2), while inappropriate high inflating pressures at birth can cause lung injury (10,11). During resuscitation, clinicians have few tools to guide the administration of a SI, hampering widespread use.
In the already aerated lung, recruitment strategies that target the point of maximum curvature on the deflation limb of the quasistatic pressure–volume relationship (12,13,14), via gradual stepwise increases and decreases in applied pressure result in greater and more homogenous recruitment, and improved oxygenation, than a SI alone (15). Such strategies generally use oxygenation to define the optimal applied pressure (13,14,16,17), an unreliable parameter at birth (18). Recently, indicators of lung mechanics have been shown to reliably define the point of maximum curvature and optimal pressure in human infants (19), with resultant improvement in compliance, carbon dioxide removal, and oxygenation. Alternatives to SI have not been examined during resuscitation of the newly born premature lung. The existing literature suggests that a stepwise PEEP strategy to aid aeration at birth and achieve lung recruitment may also overcome some of the practical issues of applying an optimal SI (15,16,19).
The aims of this study were to compare the effects of a SI and a stepwise PEEP strategy (SEP) using conventional mechanical ventilation applied at birth on gas exchange, regional and global end-expiratory volume and lung mechanics, and early indicators of lung injury in a preterm lamb model, and to determine the interaction between recruitment maneuver applied at birth and early exogenous surfactant therapy on these outcomes.
Results
There was no difference in birth weight and cord pH between the SEP (n = 10) and SI (n = 9) groups. Combined mean (SD) birth weight was 2.91 (0.34) kg and cord pH 7.31 (0.07). All animals completed the study, and there were no pneumothoraces in either group. There were seven female lambs in the SEP group and two in the SI group. Five lambs in SEP were first born compared with eight in SI. Overall, arterial partial pressure of carbon dioxide (Paco2) was kept within target range throughout the study, except at the time of the first arterial blood gas sample at 8 min in the SI group, where Paco2 was 62.1 (20.0) mmHg, and a mean (95% confidence interval (CI)) 13.1 (−0.8, 27.1) mmHg greater than SEP at that point (two-way ANOVA with Bonferroni posttest).
Figure 1 shows the positive inflating pressure (PIP), mean airway pressure (Paw), pressure amplitude at the airway opening (ΔP), delivered tidal volume (VT), and dynamic compliance (Cdyn) over the first 180 s from birth. During the first 20 s, the SEP group mean (SD) PIP was 45.9 (7.3) cmH2O compared to the 34.9 (1.7) cmH2O SI (P < 0.01; two-way ANOVA with Bonferroni posttest). The SEP group Paw during this period was 21.5 (3.0) cmH2O, and a mean (95% CI) 12.8 (7.5, 18.0) cmH2O lower than the SI Paw. Conversely, Paw was significantly higher in the SEP group between 50 and 120 s, and 170 s (all P < 0.05). ΔP and VT were significantly lower at 18 and 20 cmH2O, and during the final decremental PEEP steps (all P < 0.05). PIP was also significantly lower at the 6 cmH2O decremental step (P < 0.001).
(a) PIP, (b) ΔP, (c) Paw, (d) VT, and (e) Cdyn for the sustained inflation (closed diamonds) and SEP strategy (open circles) at 10 s intervals from birth to 180 s, and at 300 s of life. †P < 0.05 and *P < 0.0001 at corresponding time points (two-way ANOVA with Bonferroni posttest). All data are mean ± SD. Cdyn, compliance; ΔP, airway opening; Paw, airway pressure; PIP, positive inflating pressure; VT, tidal volume.
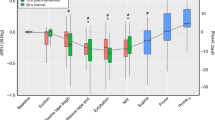
Figure 2a shows the alveolar–arterial oxygen gradient (AaDO2) data for both groups. Oxygenation was significantly better from 15 to 70 min in the SEP group compared to the SI group (all P < 0.05; Bonferroni posttest), with AaDO2 being mean (95% CI) 209 (46, 371) mmHg lower at 70 min of life.
(a) AaDO2, (b) change in EEVRIP, (c) VT, (d) Cdyn, (e) ΔP, and (f) ventral to dorsal hemithorax Cdyn ratio following sustained inflation (closed diamonds) and SEP strategy (open circles) at birth. Exogenous surfactant was administered at 10 min of life (dashed line). † Indicates a significant difference between data at corresponding time points (P values < 0.05, two-way ANOVA with Bonferroni posttest). * Indicates a significant difference between Cdyn ratio at 8 min of life in the SI group (P = 0.022, repeated-measures ANOVA with Tukey posttest). All data are mean ± SEM. AaDO2, alveolar–arterial oxygen gradient; Cdyn, compliance; EEV, end-expiratory thoracic volume; ΔP, airway opening; VT, tidal volume.
Figure 2b shows the global end-expiratory volume from birth (EEVRIP) data. At 5 min of life, the mean (SD) EEV was 6 (5) ml/kg compared with 18 (9) ml/kg following the SEP (P = 0.021; two-way ANOVA with Bonferroni posttest). Both groups continued to gain EEV such that statistical differences had disappeared by 8 min of life.
Required VT remained constant at ~7 ml/kg throughout the study in the SEP group but increased with time to a mean (SD) 8.5 (1.4) ml/kg by 70 min in the SI group ( Figure 2c ) and was statistically significant by 55 min (P < 0.01; Bonferroni posttests). Cdyn was greater at all time points in the SEP group ( Figure 2d ), as was ΔP ( Figure 2e ). Recruitment strategy significantly influenced Cdyn and ΔP (both P < 0.0001; two-way ANOVA). The PEEP that optimized Cdyn in the SEP occurred at 7.9 (1.1) cmH2O. After the initial recruitment period, Paw did not change significantly over time in each group and was higher in the SI group being, overall, a mean (SD) 19.9 (0.5) cmH2O compared with 18.3 (0.7) cmH2O in the SEP group (P < 0.001; Bonferroni posttest).
Prior to surfactant administration, the use of a SI resulted in less homogenous distribution of Cdyn than SEP ( Figure 2f ). At 8 min of life, the nondependant:dependant (V/D) ratio of relative Cdyn was a mean (95% CI) 0.25 (0.04, 0.46) higher in the SI group (Bonferroni posttest). Exogenous surfactant administration improved homogeneity of Cdyn in the SI group such that the V/D ratio from 45 min of life was lower compared with 8 min (P < 0.05; one-way ANOVA with Tukey posttest). There was no change in the distribution of Cdyn over time in the SEP group.
Overall, SEP resulted in greater recruitment of relative EEV in the nondependent hemithorax ( Figure 3a ) than SI at all time points. SEP was able to achieve an EEV approximating 1.1 of vital capacity in that region (ΔZ%VCroi) at all time points, although there was considerable intersubject variability, compared to 0.5 ΔZ%VCroi following a SI. This difference was significant prior to surfactant administration (P < 0.05; two-way ANOVA with Bonferroni posttest). Neither strategy was able to recruit relative EEV close to vital capacity in the dependent lung ( Figure 3b ). There was no difference in relative EEV following SI in the dependent and nondependent lung. Prior to surfactant administration, EEV in the nondependent lung was significantly higher than in the dependent lung in the SEP group (P < 0.05; two-way ANOVA with Bonferroni posttest).
Change in relative end-expiratory thoracic volume (ΔZ%VCroi) after sustained inflation (diamonds) and SEP strategy (circles) at birth in the nondependent (ventral; a) and dependent (dorsal; b) hemithoraces. Exogenous surfactant was administered at 10 min (dashed line). † Indicates a significant difference between data at corresponding time points (P values < 0.05, two-way ANOVA with Bonferroni posttest). * Indicates a significant difference between Z%VCroi in the dependant and nondependant hemithoraces in the SEP group at corresponding time points (P values < 0.05, two-way ANOVA with Bonferroni posttest). All data are mean ± SEM.
Lung Injury
There was no difference in connective tissue growth factor (CTGF), cysteine-rich 61 (CYR61), early growth response protein 1 (EGR1), and IL-1β, IL-6 and IL-8 mRNA between the two groups ( Table 1 ).
Discussion
In our model of the preterm surfactant-deficient lung, the use of a stepwise escalating/deescalating PEEP maneuver with volume-targeted ventilation (VTV) from birth resulted in better oxygenation, lung mechanics, and thoracic volumes, without increasing lung injury, compared with a 20-s SI followed by a similar PPV strategy. This is, to our knowledge, the first study to compare alternative recruitment approaches at birth. Previous studies being limited to strategies using SI and/or PEEP (2,6). Our study demonstrates that a SEP strategy was practical and maybe beneficial in supporting the preterm lung at birth.
The use of PEEP at birth is now widely accepted (5). PEEP maintains FRC and minimizes sheer forces (4), even without a preceding SI (2). The optimum PEEP to apply at birth remains unknown, and identifying it difficult, with detrimental results if inadequate or excessive (4). In our study, we used a PEEP of 6 cmH2O in the SI group, a clinically relevant value also based on previous literature in the preterm lamb model (20). The SEP group, which used a PEEP defined by the recipient’s response rather than the clinician, identified an optimal PEEP that was higher in most subjects. The 2 cmH2O greater PEEP, rather than the SEP maneuver, may account in part for the differences seen between the two strategies, particularly at a regional level, and future studies should compare SI and PPV at various PEEP levels against SEP. Despite this limitation, our findings highlight a clinical advantage of a SEP approach. A SI, due to its relative brevity, provides no direct feedback to the clinician as to subsequent PPV settings. In contrast, a SEP, by virtue of allowing time to evaluate physiological responses (14,19,21), provides clinical information during those critical first few minutes of life.
The use of an escalating/de-escalating PEEP strategy to recruit the lung and identify an optimal PEEP is not new (14,17,22). In the already aerated lung, these are often called open lung strategies (14), and aim to exploit hysteresis to map the quasistatic pressure–volume relationship of the lung and apply ventilation on the deflation limb at an optimal applied pressure (13,14). Reassuringly, our findings that oxygenation, lung volume, and lung mechanics are improved with this approach, are consistent with previous animal (23,24) and human (13,16,17) studies in aerated diseased lungs. It is on the deflation limb that the most homogenous regional aeration occurs (13,15) and can be maintained with a lower PEEP than needed to recruit the lung (24,25). This, and the longer time allowed for recruitment likely explains the benefits we observed with the SEP compared to the SI.
The use of Cdyn rather than oxygenation as a proxy of lung volume during the SEP strategy differentiates our study from previous open lung reports (13,19). There is a strong rationale for our approach beyond the limitations of peripheral oxygen saturation (SpO2) at birth (18). The relationship between lung mechanics and the pressure–volume relationship is well recognized (12,25), and recently, the ability to deliver an SEP using indicators of lung mechanics alone has been described by our group in humans receiving high-frequency oscillatory ventilation (19). This is the first report of a Cdyn-defined SEP strategy using conventional PPV. Cdyn and other mechanics parameters are now routinely available on modern ventilators and the use of VTV simplifies the delivery of SEP strategies such that the clinician need only adjusted PEEP. The largest imposition to using complex ventilation strategies in the delivery room environment is the lack of monitoring, despite increasing awareness of importance, and mask/endotracheal tube (ETT) leak (26). The use of modern ventilators, with reliable monitoring and adequate battery supply for transport, in the delivery room is becoming increasingly feasible and may improve resuscitation.
The SEP strategy involved transiently exposing the lung to a PEEP of 20 cmH2O, not a level we advocate in the human infant. Our rationale being that the PEEP required to obtain recruitment in our preterm lung model was unknown. Despite the transient high maximum PEEP and corresponding Paw, the overall Paw and ΔP exposure was lower in the SEP group compared with the SI group, and did not expose the lung to greater pneumothorax risk. Paradoxically, by virtue of the overall greater pressure needs, the SI group may have been at greater risk. It is possible that some subjects did not need a PEEP of 20 cmH2O to achieve recruitment, thus exposing them to transient overdistension and increased cardiovascular compromise (8,27). The open lung concept advocates a transient rerecruitment after obtaining the minimum PEEP, a PEEP that maybe associated with volume derecruitment. It is possible the transient rerecruitment to 20 cmH2O was not needed. These may have influenced the results as even brief period of injurious ventilation can initiate injury pathways (10,28). Future studies of SEP at birth should explore titrating both optimal and maximum PEEP to the Cdyn response.
The purpose of a SI at birth is to clear fetal liquid and to allow aeration using sufficient pressure and application time to overcome the high resistance and long time constant of the newly born respiratory system. Without direct imaging, it is impossible to verify whether optimal aeration was achieved in our study. Based on previous literature, 20 s at a high inflating pressure should be adequate in most subjects (6,9). Whether a longer SI, or the use of higher pressures, would have improved the SI outcome group is unclear. It is unlikely that SI of much longer than 20 s, or pressures above 40 cmH2O, will be accepted clinically at the current time.
During the first 20 s, the PIP was higher in the SEP group than the static 35 cmH2O SI. This may have exposed the SEP group to higher aerating pressures during the initial phase of lung liquid clearance. The SEP strategy provided 0.4-s dynamic inflations, resulting in a lower Paw compared to the SI distending pressure during the first 20 s. Previous literature suggests that the distending pressure is more important during aeration and recruitment than tidal PIP (2,6,20). Later, the SEP group was intentionally exposed to a higher PAW for 80 s; it is possible that this period achieved the subsequent benefits seen in the SEP groups (13,16,19). Future studies should include a group that receives PPV, with adequate PEEP but no early intentional recruitment maneuver.
Limitations
There are some additional limitations to our study. Despite randomization, there were differences in gender and parity that may have favored the SEP group. This study used an established lamb model of prematurity. This model is known to require higher pressures than human infants to adequately ventilate the lung. Our lambs were not exposed to antenatal corticosteroids. Whether the same differences would have been present if corticosteroids were administered warrants further investigation. Unlike preterm infants, spontaneous breathing was suppressed in the lambs and cuffed ETT were used, thus translating these findings into human infants should be done with caution. Airway leak remains a major problem with the implementation of any SI, PPV, and SEP strategy at birth. The limitations of electrical impedance tomography (EIT) and respiratory inductive plethysmography (RIP) to measure relative changes in volume have been well described previously (13,29,30) and are relevant to this study. RIP, in particular, is unable to distinguish between fluid and gas within the thorax. Despite these limitations, EIT remains the only validated bedside technique for measuring regional volume with clinical potential in early life (30).
Conclusion
In a preterm lamb model, the use of a stepwise PEEP strategy during PPV+VTV at birth was practical, tolerated and resulted in better oxygenation, lung mechanics and regional thoracic volume, and lower ventilator settings than a SI. These findings were not associated with increased lung injury and were sustained for at least an hour, highlighting the importance of considering respiratory therapy as a continuum that continues beyond the first critical inflations that achieve aeration. Alternative approaches to supporting the vulnerable preterm lung at birth warrant investigation.
Methods
All techniques and procedures were approved by the Animal Ethics Committee of the Murdoch Childrens Research Institute, Melbourne, Australia in accordance with National Health and Medical Research Committee guidelines.
Experimental Instrumentation
Caesarean section under general anesthesia was performed on date-mated ewes at 127–128 d of gestation (term ~145 d). On delivery of the fetal head, the carotid artery and external jugular vein were cannulated. The fetal trachea was intubated with a 4.0 mm cuffed ETT, and, as per previous reports using this model (8), fetal lung liquid passively drained for 15 s prior to clamping the ETT. The fetal thorax was then exteriorized and dried. Sixteen custom-built 23G, 3 cm long needle EIT electrodes were placed equidistant around the fetal chest at a level ~0.5 cm above the xiphisternum. The needles were secured using a 5 cm wide self-adherent bandage (Coban, 3M, St. Paul, MN), connected to a Goe-MF II EIT system (Carefusion, Hoechberg, Germany), and the quality of the electrode placement confirmed using the EIT proprietary software. Two RIP bands (Respibands, Sensormedics, Yorba Linda, CA) were secured around the chest, one parallel to the upper margin of the Coban bandage and the other immediately above the umbilicus. Following randomization to an assigned protocol, the lamb was delivered, weighed, and ventilated in a supine position.
Measurements
SpO2, heart rate, arterial blood pressure, and rectal temperature were recorded continuously from birth (HP48S; Hewlett Packard, Andover, MA). Proximal airway pressure (PAO) and flow were measured at the airway opening using a Florian respiratory mechanics monitor sampling at 200 Hz (Acutronic Medical Systems, Hirzel, Switzerland). Global lung volume (VLRIP) was measured with a DC-coupled RIP (Respitrace 200; NIMS, North Bay Village, FL) (31), sampling at 200 Hz using a method we have described previously (13,19). The RIP voltage outputs were zeroed to the signal immediately prior to starting ventilation and an uncalibrated change in volume derived from the sum of the chest and abdominal signals. Change in regional volume was measured using EIT sampling at 25 Hz (32,33,34).
Ventilation Strategies
The lambs were randomized to one of the two strategies from birth: (i) an initial SI, via the ETT, of 35 cmH2O for 20 s using a Neopuff Infant T-piece Infant Resuscitator (Fisher and Paykel Healthcare, Auckland, New Zealand), followed by 5 s at a PEEP of 6 cmH2O. The ETT was then clamped to prevent volume loss and PPV (SLE5000; SLE, South Croydon, UK) commenced in VTV mode at a PEEP of 6 cmH2O, inflation time 0.4 s, VTV 7 ml/kg (maximum PIP 50 cmH2O); or (ii) stepwise PEEP strategy (14), using PPV+VTV (7 ml/kg and maximum PIP 50 cmH2O). Commencing at a PEEP of 4 cmH2O, PEEP was increased by 2 cmH2O every 10 inflations until a PEEP of 20 cmH2O (maximum PEEP setting on ventilator). PEEP was then decreased every 10 inflations to a PEEP of 6 cmH2O. During this process, the Cdyn displayed by the ventilator was observed, and the PEEP that resulted in the highest Cdyn during the decremental phase documented. Then, the lung was rerecruited by transiently exposing the lung to 10 inflations at PEEP 20 cmH2O (13,14,16), and PPV placed at the PEEP that optimized Cdyn. All other PPV+VTV settings were as per SI group.
In both groups, exogenous surfactant (Curosurf 100 mg/kg; Chiesi, Parma, Italy) was administered into the trachea over 30–60 s at 10 min of life using an inline premeasured catheter. PPV was initially applied with a fraction of inspired oxygen (FIO2) of 0.21 in both groups and then titrated to maintain SpO2 of 88–94%. VTV was adjusted to maintain a Paco2 between 45 and 60 mmHg on arterial blood gas analysis measured at 8, 15, 25, 40, 55, and 70 min of life.
At 70 min of life, the animals were ventilated with 1.0 FIO2 for 3 min, after which the ETT was disconnected for 2 min to aid lung collapse. Then, a static in vivo supersyringe pressure–volume curve was performed to a maximum pressure of 40 cmH2O. Lambs were then humanely euthanized with pentobarbitone.
Data Acquisition and Analysis
PAO, flow, VLRIP, SpO2, heart rate, temperature, and arterial blood pressure were recorded at 1,000 Hz and digitized using a computerized data acquisition program (Powerlab and LabChart V7; AD Instruments, Sydney, Australia). These parameters and EIT, were continuously recorded for the first 15 min of life, then at 2 min intervals immediately prior to arterial blood gas analysis, and during the static pressure–volume curve. Data were analyzed continuously during and up to 1 min after completion of each recruitment maneuver, then the last 30 s of stable recordings at 5 min of life, and coinciding with arterial blood gas analysis were used. Applied PIP, PEEP, Paw, and ΔP were determined offline. Delivered VT and Cdyn were calculated from the flow and PAO data. The AaDO2 was calculated from the arterial blood gas parameters. Change in EEVRIP from birth was determined from the trough of the VLRIP signal. VLRIP voltage signals were calibrated to the known volumes from the static pressure–volume curve using the in-built multipoint linear calibration module in LabChart.
Relative impedance measured by EIT was analyzed offline (AUSPEX V1.6; Carefusion) using our previously described method (32,35,36). The EIT recordings were referenced to the signal immediately prior to ventilation to determine relative change in impedance (ΔZ) from birth. EEV was then determined from the trough of the impedance signals after applying a low-pass filter at 10 breaths per minute above the second harmonic of the respiratory signal (respiratory domain) (34,37,38). Relative change in EEV from birth was then determined in the nondependant (ventral) and dependant (dorsal) hemithoraces. To allow for intersubject comparison, the EIT data were normalized to vital capacity for each hemithorax. Vital capacity was defined as the impedance change with each hemithorax between 0 and 40 cmH2O during the static PV curve (Z%VCroi) (33,36).
Relative regional Cdyn was determined from the EIT signals within the nondependant and dependant hemithoraces using the method described by Dargaville et al. (33). The breath-by-breath tidal amplitude of the impedance signal in each region was determined and divided by the corresponding ΔP to determine a regional Cdyn in arbitary units. The V/D ratio of relative Cdyn was then determined for each inflation to allow comparison of the homogeneity of relative regional mechanics between subjects. A V/D ratio of 1.0 indicates that the Cdyn is the same in both lung fields, a value >1.0 indicates that Cdyn is better in the nondependant lung.
Lung Injury Analysis
Lung tissue samples were taken from the right lower lobe and immediately frozen in liquid nitrogen for quantitative real-time PCR analysis of early biomarkers of lung injury; CTGF, CYR61, EGR1, IL-1β, IL-6 and IL-8 mRNA as described previously (28). Quantitative real-time PCR results were analyzed using the 2−ΔΔCT method (28).
Statistical Analysis
Data were tested for normality and analyzed with a one-way ANOVA or two-way repeated measures ANOVA using time and ventilation strategy as factors and appropriate posttests. Statistical analysis was performed with GraphPad PRISM 4.02 (GraphPad Software, San Diego, CA) and a P < 0.05 considered significant.
Statement of Financial Support
This study is supported by a National Health and Medical Research Council Project Grant, Canberra, Australia (Grant ID 1009287) and the Victorian Government Operational Infrastructure Support Program. DGT is supported by a National Health and Medical Research Council Clinical Career Development Fellowship (Grant ID 1053889). PGD is supported by a National Health and Medical Research Council Program Grant (Grant ID 606789) and Practitioner Fellowship (Grant ID 556600).
Disclosure
None.
References
Hooper SB, Kitchen MJ, Wallace MJ, et al. Imaging lung aeration and lung liquid clearance at birth. FASEB J 2007;21:3329–37.
te Pas AB, Siew M, Wallace MJ, et al. Establishing functional residual capacity at birth: the effect of sustained inflation and positive end-expiratory pressure in a preterm rabbit model. Pediatr Res 2009;65:537–41.
Siew ML, Te Pas AB, Wallace MJ, et al. Positive end-expiratory pressure enhances development of a functional residual capacity in preterm rabbits ventilated from birth. J Appl Physiol 2009;106:1487–93.
Probyn ME, Hooper SB, Dargaville PA, McCallion N, Harding R, Morley CJ . Effects of tidal volume and positive end-expiratory pressure during resuscitation of very premature lambs. Acta Paediatr 2005;94:1764–70.
Perlman JM, Wyllie J, Kattwinkel J, et al.; Neonatal Resuscitation Chapter Collaborators. Neonatal resuscitation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Pediatrics 2010;126:e1319–44.
te Pas AB, Siew M, Wallace MJ, et al. Effect of sustained inflation length on establishing functional residual capacity at birth in ventilated premature rabbits. Pediatr Res 2009;66:295–300.
te Pas AB, Walther FJ . A randomized, controlled trial of delivery-room respiratory management in very preterm infants. Pediatrics 2007;120:322–9.
Polglase GR, Hooper SB, Gill AW, et al. Cardiovascular and pulmonary consequences of airway recruitment in preterm lambs. J Appl Physiol 2009;106:1347–55.
Walsh MC, Carlo WA . Sustained inflation during HFOV improves pulmonary mechanics and oxygenation. J Appl Physiol 1988;65:368–72.
Björklund LJ, Ingimarsson J, Curstedt T, et al. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res 1997;42:348–55.
Jobe AH, Kramer BW, Moss TJ, Newnham JP, Ikegami M . Decreased indicators of lung injury with continuous positive expiratory pressure in preterm lambs. Pediatr Res 2002;52:387–92.
Goddon S, Fujino Y, Hromi JM, Kacmarek RM . Optimal mean airway pressure during high-frequency oscillation: predicted by the pressure-volume curve. Anesthesiology 2001;94:862–9.
Tingay DG, Mills JF, Morley CJ, Pellicano A, Dargaville PA . The deflation limb of the pressure-volume relationship in infants during high-frequency ventilation. Am J Respir Crit Care Med 2006;173:414–20.
Lachmann B . Open up the lung and keep the lung open. Intensive Care Med 1992;18:319–21.
Pellicano A, Tingay DG, Mills JF, Fasulakis S, Morley CJ, Dargaville PA . Comparison of four methods of lung volume recruitment during high frequency oscillatory ventilation. Intensive Care Med 2009;35:1990–8.
De Jaegere A, van Veenendaal MB, Michiels A, van Kaam AH . Lung recruitment using oxygenation during open lung high-frequency ventilation in preterm infants. Am J Respir Crit Care Med 2006;174:639–45.
Rimensberger PC, Beghetti M, Hanquinet S, Berner M . First intention high-frequency oscillation with early lung volume optimization improves pulmonary outcome in very low birth weight infants with respiratory distress syndrome. Pediatrics 2000;105:1202–8.
Dawson JA, Kamlin CO, Vento M, et al. Defining the reference range for oxygen saturation for infants after birth. Pediatrics 2010;125:e1340–7.
Tingay DG, Mills JF, Morley CJ, Pellicano A, Dargaville PA . Indicators of optimal lung volume during high-frequency oscillatory ventilation in infants. Crit Care Med 2013;41:232–9.
Sobotka KS, Hooper SB, Allison BJ, et al. An initial sustained inflation improves the respiratory and cardiovascular transition at birth in preterm lambs. Pediatr Res 2011;70:56–60.
Miedema M, de Jongh FH, Frerichs I, van Veenendaal MB, van Kaam AH . The effect of airway pressure and oscillation amplitude on ventilation in pre-term infants. Eur Respir J 2012;40:479–84.
Froese AB . The incremental application of lung-protective high-frequency oscillatory ventilation. Am J Respir Crit Care Med 2002;166:786–7.
van Kaam AH, de Jaegere A, Haitsma JJ, Van Aalderen WM, Kok JH, Lachmann B . Positive pressure ventilation with the open lung concept optimizes gas exchange and reduces ventilator-induced lung injury in newborn piglets. Pediatr Res 2003;53:245–53.
Rimensberger PC, Cox PN, Frndova H, Bryan AC . The open lung during small tidal volume ventilation: concepts of recruitment and “optimal” positive end-expiratory pressure. Crit Care Med 1999;27:1946–52.
Rimensberger PC, Pache JC, McKerlie C, Frndova H, Cox PN . Lung recruitment and lung volume maintenance: a strategy for improving oxygenation and preventing lung injury during both conventional mechanical ventilation and high-frequency oscillation. Intensive Care Med 2000;26:745–55.
Schmölzer GM, Morley CJ, Wong C, et al. Respiratory function monitor guidance of mask ventilation in the delivery room: a feasibility study. J Pediatr 2012;160:377–381.e2.
Polglase GR, Morley CJ, Crossley KJ, et al. Positive end-expiratory pressure differentially alters pulmonary hemodynamics and oxygenation in ventilated, very premature lambs. J Appl Physiol 2005;99:1453–61.
Wallace MJ, Probyn ME, Zahra VA, et al. Early biomarkers and potential mediators of ventilation-induced lung injury in very preterm lambs. Respir Res 2009;10:19.
Wolf GK, Arnold JH . Noninvasive assessment of lung volume: respiratory inductance plethysmography and electrical impedance tomography. Crit Care Med 2005;33:Suppl 3:S163–9.
Leonhardt S, Lachmann B . Electrical impedance tomography: the holy grail of ventilation and perfusion monitoring? Intensive Care Med 2012;38:1917–29.
Markhorst DG, Jansen JR, van Vught AJ, van Genderingen HR . Breath-to-breath analysis of abdominal and rib cage motion in surfactant-depleted piglets during high-frequency oscillatory ventilation. Intensive Care Med 2005;31:424–30.
Tingay DG, Copnell B, Grant CA, Dargaville PA, Dunster KR, Schibler A . The effect of endotracheal suction on regional tidal ventilation and end-expiratory lung volume. Intensive Care Med 2010;36:888–96.
Dargaville PA, Rimensberger PC, Frerichs I . Regional tidal ventilation and compliance during a stepwise vital capacity manoeuvre. Intensive Care Med 2010;36:1953–61.
Frerichs I, Dargaville PA, van Genderingen H, Morel DR, Rimensberger PC . Lung volume recruitment after surfactant administration modifies spatial distribution of ventilation. Am J Respir Crit Care Med 2006;174:772–9.
Bhatia R, Schmölzer GM, Davis PG, Tingay DG . Electrical impedance tomography can rapidly detect small pneumothoraces in surfactant-depleted piglets. Intensive Care Med 2012;38:308–15.
Hepponstall JM, Tingay DG, Bhatia R, Loughnan PM, Copnell B . Effect of closed endotracheal tube suction method, catheter size, and post-suction recruitment during high-frequency jet ventilation in an animal model. Pediatr Pulmonol 2012;47:749–56.
Armstrong RK, Carlisle HR, Davis PG, Schibler A, Tingay DG . Distribution of tidal ventilation during volume-targeted ventilation is variable and influenced by age in the preterm lung. Intensive Care Med 2011;37:839–46.
Carlisle HR, Armstrong RK, Davis PG, Schibler A, Frerichs I, Tingay DG . Regional distribution of blood volume within the preterm infant thorax during synchronised mechanical ventilation. Intensive Care Med 2010;36:2101–8.
Acknowledgements
The authors wish to thank M Sourial and S Osterfield for their assistance in preparation of the ewe and lamb model.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tingay, D., Bhatia, R., Schmölzer, G. et al. Effect of sustained inflation vs. stepwise PEEP strategy at birth on gas exchange and lung mechanics in preterm lambs. Pediatr Res 75, 288–294 (2014). https://doi.org/10.1038/pr.2013.218
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2013.218
This article is cited by
-
Quantitative lung ultrasound detects dynamic changes in lung recruitment in the preterm lamb
Pediatric Research (2023)
-
Respiratory strategy at birth initiates distinct lung injury phenotypes in the preterm lamb lung
Respiratory Research (2022)
-
Higher CPAP levels improve functional residual capacity at birth in preterm rabbits
Pediatric Research (2022)
-
Feasibility of combining two individualized lung recruitment maneuvers at birth for very low gestational age infants: a retrospective cohort study
BMC Pediatrics (2020)
-
Plasma proteomics reveals gestational age-specific responses to mechanical ventilation and identifies the mechanistic pathways that initiate preterm lung injury
Scientific Reports (2018)