Abstract
Background:
Catch-up growth may predispose to obesity and metabolic sequelae. We sought to examine the trajectory and correlates of growth and catch up among extremely-low-birth-weight (ELBW) (<1 kg) adolescents.
Methods:
A cohort study of 148 neurologically normal ELBW children and 115 normal-birth-weight (NBW) controls born during the period 1992–1995 was conducted. Longitudinal measures of gender-specific growth of ELBW children from birth, in addition to growth and measures of obesity of ELBW and NBW children at 14 y, were evaluated.
Results:
Following neonatal growth failure, ELBW children had accelerated growth, but at 8 y, they still had lower weight and height z scores than NBW children. By 14 y, ELBW boys had caught up in growth to their NBW controls, but ELBW girls remained significantly smaller. ELBW children, however, did not differ from their controls in measures of obesity. In hierarchical multiple regression analyses, only maternal BMI and weight gain during infancy and childhood predicted the ELBW children’s 14-y weight z scores, BMI z scores, and abdominal circumference. Perinatal risk factors, including intrauterine growth, only predicted growth up to 20 mo.
Conclusion:
Maternal BMI and rate of growth, rather than perinatal factors, predict 14-y obesity among neurologically normal ELBW adolescents.
Similar content being viewed by others
Main
Preterm infants have traditionally suffered from neonatal growth failure due to inadequate nutrition and chronic complications of prematurity. The majority catch up in growth, although their growth attainment may be less than that of normal-birth-weight (NBW) children (1,2). The implications of this catch-up growth for long-term cardiovascular and metabolic health have been the subject of interest for many years (3,4) but have become more critical since childhood obesity became epidemic (5).
We recently reported on the increase in rates of obesity between ages 8 and 14 y among extremely-low-birth-weight (ELBW) children born during the period 1992–1995 (6). In the current report, we sought to examine the children’s gender-specific trajectory and correlates of growth and catch up from birth. We hypothesized that by age 14 y, the ELBW children would catch up to NBW controls in weight, height, and clinical measures of obesity, and that the predictors of growth would include socioenvironmental, perinatal, and neonatal risk factors.
Results
Descriptors of ELBW and NBW Children
ELBW boys and girls did not differ significantly from their respective NBW peers in maternal sociodemographic factors (socioeconomic status (SES)) with the exception that mothers of ELBW girls were older and had a higher mean family income than mothers of NBW girls. ELBW girls reported less physical activity than NBW girls. Age of puberty was similar between groups ( Table 1 ). Within the ELBW population, bronchopulmonary dysplasia (BPD, oxygen dependence at 36 wk) and sepsis were the most common neonatal complications. ELBW boys had higher rates of BPD and postnatal steroid therapy than girls.
Longitudinal Changes in Growth
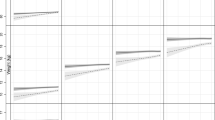
The mean weight z scores (ZWT), i.e., standard deviation scores of ELBW children at birth was −0.72 for boys and −0.96 for girls. Due to neonatal growth failure, by 40 wk, these values decreased to −1.97 among boys and −2.02 among girls, and by age 14 y, they increased to +0.07 and +0.14, respectively. Mean birth length or height z scores similarly decreased at 40 wk and then increased at 14 y ( Figure 1 and Supplementary Table S1 online). Among the ELBW children, catch-up growth (≥0.67 SD) occurred between all periods of study. Between ages 8 and 14 y, the increases in growth as measured by an increase in mean weight and height z scores per month or by catch-up growth were significantly greater for ELBW boys than for NBW boys, whereas this was not evident among girls ( Table 2 ). The growth of the children with measures from their biological mothers was similar to that of the children of mothers who did not have growth measures (data not shown).
Mean weight and height z scores ± SD of extremely-low-birth-weight (ELBW) boys and girls at birth, 40 wk (term), 8 and 20 mo, and 8 and 14 y, and mean weight and height z scores ± SD of normal-birth-weight (NBW) boys and girls at ages 8 and 14 y. (a) Weight measures and (b) height measures. Measures of ELBW boys are indicated by dots and solid lines, and measures of ELBW girls are indicated by squares and dashed lines. Measures of NBW boys are indicated by diamonds and solid lines, and measures of NBW girls are indicated by triangles and dashed lines.
Eight- and 14-y Growth of ELBW and NBW Children
Among both ELBW and NBW children, the height z score was lower than ZWT at both 8 and 14 y ( Table 3 ). At 8 y, ELBW boys and girls had significantly lower mean weight and height z scores than their NBW peers. At 14 y, although ELBW boys still had a lower weight and height than NBW boys, the differences were not significant. ELBW girls, however, remained significantly smaller than their peers. Nine of 15 girls who were overweight at 8 y became obese by 14 y with rates of obesity increasing from 12 to 21% (P = 0.049) compared with an increase of 18 to 19% among the NBW children. The mean BMI (weight/height2) z scores and rates of obesity did not differ significantly between ELBW and NBW boys or girls at 8 or 14 y nor did the mean 14-y abdominal circumference.
Longitudinal Correlates of Growth
The univariate perinatal and neonatal correlates of the weight and BMI z scores were significant up to 8 y, the majority only up to 20 mo. They included preeclampsia, birth weight z score, small-for-gestational-age (SGA) status, gestational age (GA), total number of neonatal complications, and duration of hyperalimentation (see Supplementary Tables S2 and S3 online). The predictors of the height z scores were similar (data not shown).
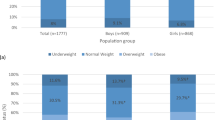
In the hierarchical multiple regression analyses ( Table 4 ), birth weight z score was positively, and duration of hyperalimentation was negatively, associated with ZWT at 40 wk. Birth weight z score, GA, and change in ZWT from 40 wk to 8 mo of conceptual age (CA), along with maternal BMI and the interaction of maternal BMI and gender, were associated with ZWT at 8 mo. Maternal BMI was positively associated with 8-mo ZWT in girls (β = 0.048 (95% confidence interval: 0.018–0.078); P = 0.002) but not in boys (β = 0.004 (95% confidence interval: −0.024 to 0.031); P = 0.80). This relationship also held at other ages as illustrated in a plot of ZWT vs. maternal BMI by gender at age 14 y ( Figure 2 ). Results of the regressions of ZWT at 20 mo were similar to those at 8 mo, except that GA was no longer a significant predictor. In the regression of ZWT at 8 y, maternal BMI along with changes in the child’s ZWT from 40 wk to 8 mo and from 8 mo to 8 y were all significant predictors. In addition, changes in ZWT during all three prior periods were significantly associated with ZWT at 14 y (all P values <0.001). After adjusting for variables included in the final model, neither age of puberty nor physical activity were significant predictors (data not shown). Hierarchical multiple regressions of the adolescent BMI z score and of abdominal circumference at 14 y were very similar to the results for the 14-y ZWT ( Table 5 ). Only 13 ELBW children of biological mothers were obese at 14 y, precluding multivariable logistic regression modeling of obesity.
Plots of weight z scores of extremely-low-birth-weight boys and girls at 14 y vs. maternal BMI by gender illustrating the interactive effect of gender and maternal BMI on the weight z score. Estimated regression coefficients of maternal BMI on weight z score were 0.1068 (95% confidence interval: 0.0633–0.1503) for girls and 0.0202 (−0.0279 to 0.0682) for boys. Measures of boys are indicated by dots and solid lines, and measures of girls are indicated by squares and dashed lines.
The findings were similar when SGA, defined either as weight <−2 SD or <10th percentile for GA, was used in place of ZWT at birth, with the exception that GA was no longer a significant predictor (see Supplementary Tables S4–S7 online).
Discussion
The results of this longitudinal study reveal that neurologically normal ELBW children demonstrated accelerated growth following neonatal growth failure. Although their weight and height z scores were still lower than those of NBW controls at age 8 y, by 14 y, these did not differ significantly among boys, whereas ELBW girls continued to have significantly lower weight and height z scores than their NBW peers. Both ELBW and NBW children had higher weight than height z scores. The rates of obesity, mean BMI z scores, and 14-y abdominal circumference of the ELBW children, although lower, did not differ significantly from those of their NBW peers. Multivariable analyses revealed that neither intrauterine growth, as measured by birth weight z score or SGA status, nor neonatal risk factors were associated with the child’s gain in weight after 20 mo of CA. The only factors that predicted 14-y measures of obesity were the child’s weight gain during each of the periods studied and maternal BMI which affected girls more than boys.
The only study of the adolescent growth of preterm children born in the 1990s pertains to 11-y-old <26-wk gestation Swedish children who remained smaller than controls, but similar to our findings, they did not differ in BMI (7). It is interesting that the obesity epidemic in the 1990s has been associated with an increase in the rates of obesity of both preterm and NBW children as compared with their rates of obesity reported in the 1980s (2,5,8).
Studies of predictors of growth among preterm children have pertained mainly to infancy and childhood. Correlates of reduced growth have included male gender, lower birth weight and gestation, SGA birth weight, and various neonatal complications (9,10,11,12,13,14). Similar to our results, Ehrenkranz et al. (14) found the duration of hyperalimentation to be inversely associated with growth, as sicker infants need hyperalimentation for longer periods. Smoking during pregnancy and postnatal steroid therapy were not significant predictors of growth in our univariate analyses, possibly due to the fact that the effects of postnatal steroids on growth may be transient (9) and that maternal smoking affects fetal growth only in term-born children (15). These factors were thus not included in our multivariable models. SES and ethnicity, known correlates of growth, were not significant predictors in our population. Self-reported physical activity was also not predictive, possibly related to the lesser physical activity of ELBW children (6).
Significant associations between parent and child growth have been reported in normal (16,17) and preterm populations (1,2,7,18,19), and similar to our findings, these were found to be greater in girls than those in boys (17). Multiple factors contribute to the effect of parental growth, including genetic, hormonal, and shared environmental and psychosocial characteristics.
Our finding that weight gain throughout infancy and childhood is associated with 14-y measures of obesity is in agreement with the literature that there is no specific critical period of child growth that predicts later obesity (20) or its cardiovascular and metabolic sequelae (21,22,23). Although the ELBW children attained similar rates of obesity as their peers, their catch-up growth is of concern, especially among girls whose rates of obesity increased significantly between 8 and 14 y, a finding also reported by Saigal et al. (2). Among preterm children, rapid growth is associated with insulin sensitivity and may be a risk factor for type 2 diabetes and cardiovascular risk (24,25).
This is the first report of the sequential correlates of growth of preterm children born in the 1990s. Strengths of the study include its longitudinal design, relatively good follow-up rate, and the many risk factors considered. The rates of obesity of our NBW children and their mothers were representative of national data (5,26). We also acknowledge several limitations. Our results may have been influenced by the lower follow-up rate of ELBW boys and that participant boys had less BPD, thus lower neonatal risk, than nonparticipant boys. Difficulty in stretching immature sick infants may have influenced the initial length z scores, which were much lower than those of weight at birth and at 40 wk. Had we included the neurologically abnormal children, neonatal risk factors such as postnatal steroid therapy and periventricular hemorrhage, which predispose to the development of cerebral palsy, may have been predictive of the growth outcomes. Multiple births were included in the study as they did not influence longitudinal growth, which was similar to that of singletons (data not presented). A further consideration is that early postnatal nutrition was less than currently advised (27) and that we lack detailed information on neonatal nutrition, including breast milk. However, current modes of neonatal nutrition have not eliminated childhood growth failure, and although beneficial for brain growth (28), may contribute to future metabolic risk (29). Maternal prepregnancy weight and paternal weight were also lacking, although the mother’s current weight should reflect her prepregnancy weight, and maternal effects on obesity are greater than paternal effects (17). The Center for Disease Control and Prevention norms are not representative of our urban, predominantly minority population, but we had a sociodemographically similar control population for comparison. We lacked measures of body composition and metabolic markers, but BMI, the measure we used, is associated with elevated body fat (30), and abdominal circumference is a proxy measure of abdominal fat mass (31).
The accelerated catch-up growth of the ELBW children and its potential associated with cardiovascular and metabolic risk (32) is concerning as it may add to their high rates of chronic problems and further increase health-care utilization (6). Possible intervention strategies include attempts to decrease maternal obesity and optimize diet to promote catch up in height without promoting overweight. The latter may be very difficult as the lower height than weight z scores that we have documented reflect the notion that growth in weight may end in overshooting and obesity, whereas growth in height may be limited by a “self-stat” mechanism (33). Physical activities should also be encouraged despite the respiratory and subtle neurologic difficulties of ELBW children.
Methods
ELBW Group
The birth cohort of 161 boys and 183 girls was admitted to Rainbow Babies and Children’s Hospital, Cleveland, Ohio between 1992 and 1995. Thirteen children were excluded because of congenital conditions (6). Of the remaining children, 101 (65%) boys and 137 (78%) girls survived, of whom 70 (69%) boys and 111 (81%) girls were followed to age 14 y. Sixteen boys and 15 girls with cerebral palsy were excluded because of the known poor growth of neurologically abnormal children and 2 boys did not have 14-y growth measures. The study population thus included 52 boys and 96 girls who had 14-y growth measures. They did not differ from the nonparticipant birth cohort with the exception that fewer boys participated (51% boys vs. 70% girls; P < 0.01) and that the participant boys had lower rates of BPD and a shorter neonatal hospitalization.
NBW Children
Sixty-five NBW boys and 111 NBW girls, of the same sex, race, school, and age within 3 mo, were recruited at 8 y, of whom 42 boys (65%) and 73 girls (65%) were followed to 14 y, all of whom had growth measures. They did not differ in SES from the nonparticipants with the exception that more mothers of boys were married.
Biological Mothers
Biological mothers represented 116 (78%) caregivers of ELBW children and 101 (88%) caregivers of NBW children of whom 105 (91%) and 96 (83%) of mothers, respectively, had growth measures. Mothers of the ELBW children with growth measures were significantly younger than those who did not have growth measures but did not differ in SES, perinatal risk factors, or their children’s neonatal risk factors. The mothers of ELBW children did not differ in weight, height, or BMI from those of NBW children (see Supplementary Table S8 online) and were also representative of national data for women aged 40–59 y (26).
Neonatal Care and Measures of Outcome
Neonatal care was according to practice during the 1990s. The majority of infants received parenteral nutrition (hyperalimentation) of <3 mg/kg of protein per day. Sociodemographic, perinatal, and neonatal data were documented at neonatal hospital discharge. Weight and length were measured at birth and then at 40 wk (term date as estimated from the last menstrual period and pregnancy ultrasound, when available); at 8 and 20 mo of CA; and at 8 and 14 y’ postnatal age. The children were measured according to standard procedures. The children were weighed unclothed but lightly clothed at 14 y. To correct for this clothing, we subtracted 1.0 kg for boys and 0.5 kg for girls. Length was measured supine with a tape measure at birth; with an infantometer at 40 wk, 8 and 20 mo of CA; and with a stadiometer after removing shoes at 8 and 20 y (Harpenden, Holtain, Crymych, UK). Maternal weight and height were similarly measured. The children’s abdominal circumference, a proxy for visceral fat, was measured at 14 y according to the National Health and Nutrition Survey (NHANES) procedure (34).
Weight z scores were computed at birth and 40 wk using standards which exclude infants delivered for maternal and fetal indications, many complicated with intrauterine growth failure (35). Length z scores at birth were computed according to Usher and McLean (36). At 8 and 20 mo of CA and at 8 and 14 y, weight and height z scores were computed from the Center for Disease Control and Prevention growth data (37). The Center for Disease Control and Prevention BMI norms (z scores) are only available from age 24 mo. We could thus only calculate the BMI z scores of the ELBW cohort at 8 and 14 y. BMI was thus computed at 8 and 14 y and obesity defined as BMI ≥95th percentile. Catch-up growth was defined as an increase in weight or height z score (SD) of >0.67 (i.e., crossing of percentiles) (38). Additional 14-y measures included the adolescent self-report of physical activity during the past 4 wk (39) and pubertal development (40).
The study was approved by the Institutional Review Board of University Hospitals Case Medical Center, Cleveland, Ohio. Written consent was obtained from parents and assent from children.
Data Analysis
Within the ELBW cohort, we examined gender-specific growth parameters at each age, changes in z scores between each age studied, and rates of catch-up growth. The 8- and 14-y growth measures of the ELBW and NBW children were compared using two-sample t-tests after adjusting for race and z SES.
Correlates of growth were considered only for children of biological mothers with growth measures (16). Pearson correlation coefficients calculated at each age studied included maternal education, race, and z SES, defined as a composite of the sample z score for maternal education and family income (6). Perinatal data included a history of smoking during pregnancy, preeclampsia, antenatal steroid therapy, birth weight z score, GA, SGA, considered both as birth weight <–2 SD and as <the 10th percentile for GA, and multiple birth. Neonatal risk factors included the rates of BPD, sepsis (positive blood culture), severe cerebral ultrasound abnormality, necrotizing enterocolitis, the total number of these neonatal complications, the duration of parenteral nutrition (hyperalimentation), the duration of hospitalization, and postnatal steroid therapy. Maternal growth correlates considered included weight, height, and BMI.
A hierarchical multiple regression approach was used to examine risk factors related to ZWT at 40 wk, 8 and 20 mo’ corrected age, and 8 and 14 y postnatal age. ZWT, rather than BMI, was used for these longitudinal analyses as the Center for Disease Control and Prevention norms for BMI are only available from age 24 mo (37). In the first and all stages, sociodemographic factors (z SES, race, and gender) and maternal BMI were forced into the models. In the first stage, interactions of gender with the other factors were tested. In the second stage, factors forced in or found to be statistically significant (P < 0.05) in the first stage were included, and perinatal factors associated with intrauterine and/or postnatal growth and the change in weight z score from birth to 40 wk were then examined using stepwise regression, retaining those factors significant at P < 0.05. Interactions of birth and perinatal factors with gender were also examined in stage 2 and included if found significant (P < 0.05). The third stage, carried out only when examining ZWT at 8 and 14 y, included terms retained in stages 1 and 2 and examined changes in ZWT from birth to 40 wk, 40 wk to 8 mo, 8 mo to 8 y, and 8 to 14 y (when examining ZWT at 14 y) using stepwise regression. Interactions of predictors found significant in stage 3 with gender were also examined. The maternal BMI × gender interaction was significant in modeling ZWT at 8 and 20 mo and 14 y and bordered on significance in modeling these scores at 8 y (P = 0.07); hence, this term was also included in the final 8-y model. Age of puberty and physical activity were each examined by testing whether they added significantly to the final model. A similar approach was used at 14 y to examine predictors of the child’s BMI z score, rates of obesity, and abdominal circumference. In addition, in separate analyses, we examined the effect of SGA birth rather than ZWT on the longitudinal growth. All the analyses included only subjects with no missing covariates and growth measured at all time points (n = 94 for ZWT and n = 95 for BMI z score).
Statement of Financial Support
This study was supported by grants R01 HD 39756, M01 RR000, and ULI RR024989 from the US National Institutes of Health (Bethesda, MD).
Disclosure
None of the authors have any conflicts of interest.
Additional Author Information
Dr Hack supervised the study, had full access to all of the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis. Drs Hack, Taylor, and Schluchter developed the study concept and design. Drs Hack and Andreias acquired the data. Drs Hack, Schluchter, Taylor, Cuttler, Andreias, and Ms Margevicius participated in the analysis, including statistical analysis, and interpretation of the data. Dr Hack drafted the first version of the manuscript, and all the coauthors participated in the critical revision of the manuscript and approve its submission for publication.
References
Hack M, Schluchter M, Cartar L, Rahman M, Cuttler L, Borawski E . Growth of very low birth weight infants to age 20 years. Pediatrics 2003;112(1 Pt 1):e30–8.
Saigal S, Stoskopf B, Streiner D, Paneth N, Pinelli J, Boyle M . Growth trajectories of extremely low birth weight infants from birth to young adulthood: a longitudinal, population-based study. Pediatr Res 2006;60:751–8.
Lucas A . Long-term programming effects of early nutrition – implications for the preterm infant. J Perinatol 2005;25:Suppl 2:S2–6.
Hales CN, Ozanne SE . The dangerous road of catch-up growth. J Physiol (Lond) 2003;547(Pt 1):5–10.
Ogden CL, Carroll MD, Kit BK, Flegal KM . Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA 2012;307:483–90.
Hack M, Schluchter M, Andreias L, et al. Change in prevalence of chronic conditions between childhood and adolescence among extremely low-birth-weight children. JAMA 2011;306:394–401.
Farooqi A, Hägglöf B, Sedin G, Gothefors L, Serenius F . Growth in 10- to 12-year-old children born at 23 to 25 weeks’ gestation in the 1990s: a Swedish national prospective follow-up study. Pediatrics 2006;118:e1452–65.
Ogden CL, Fryar CD, Carroll MD, Flegal KM . Mean body weight, height, and body mass index, United States 1960-2002. Adv Data 2004:347:1–17.
Bracewell MA, Hennessy EM, Wolke D, Marlow N . The EPICure study: growth and blood pressure at 6 years of age following extremely preterm birth. Arch Dis Child Fetal Neonatal Ed 2008;93:F108–14.
Dusick AM, Poindexter BB, Ehrenkranz RA, Lemons JA . Growth failure in the preterm infant: can we catch up? Semin Perinatol 2003;27:302–10.
Clark RH, Thomas P, Peabody J . Extrauterine growth restriction remains a serious problem in prematurely born neonates. Pediatrics 2003;111(5 Pt 1):986–90.
Rijken M, Wit JM, Le Cessie S, Veen S ; Leiden Follow-Up Project on Prematurity. The effect of perinatal risk factors on growth in very preterm infants at 2 years of age: the Leiden Follow-Up Project on Prematurity. Early Hum Dev 2007;83:527–34.
Cole CR, Hansen NI, Higgins RD, Ziegler TR, Stoll BJ ; Eunice Kennedy Shriver NICHD Neonatal Research Network. Very low birth weight preterm infants with surgical short bowel syndrome: incidence, morbidity and mortality, and growth outcomes at 18 to 22 months. Pediatrics 2008;122:e573–82.
Ehrenkranz RA, Younes N, Lemons JA, et al. Longitudinal growth of hospitalized very low birth weight infants. Pediatrics 1999;104(2 Pt 1):280–9.
Kayemba-Kay’s S, Ribrault A, Burguet A, et al. Maternal smoking during pregnancy and fetal growth. Effects in preterm infants of gestational age less than 33 weeks. Swiss Med Wkly 2010;140:w13139.
Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH . Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997;337:869–73.
Hesketh K, Wake M, Waters E, Carlin J, Crawford D . Stability of body mass index in Australian children: a prospective cohort study across the middle childhood years. Public Health Nutr 2004;7:303–9.
Casey PH, Bradley RH, Whiteside-Mansell L, Barrett K, Gossett JM, Simpson PM . Evolution of obesity in a low birth weight cohort. J Perinatol 2012;32:91–6.
Doyle LW, Faber B, Callanan C, Ford GW, Davis NM . Extremely low birth weight and body size in early adulthood. Arch Dis Child 2004;89:347–50.
Parsons TJ, Power C, Manor O . Fetal and early life growth and body mass index from birth to early adulthood in 1958 British cohort: longitudinal study. BMJ 2001;323:1331–5.
Barker DJ, Osmond C, Forsén TJ, Kajantie E, Eriksson JG . Trajectories of growth among children who have coronary events as adults. N Engl J Med 2005;353:1802–9.
Bhargava SK, Sachdev HS, Fall CH, et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med 2004;350:865–75.
Forsén T, Eriksson J, Tuomilehto J, Reunanen A, Osmond C, Barker D . The fetal and childhood growth of persons who develop type 2 diabetes. Ann Intern Med 2000;133:176–82.
Fewtrell MS, Doherty C, Cole TJ, Stafford M, Hales CN, Lucas A . Effects of size at birth, gestational age and early growth in preterm infants on glucose and insulin concentrations at 9-12 years. Diabetologia 2000;43:714–7.
Rotteveel J, van Weissenbruch MM, Twisk JW, Delemarre-Van de Waal HA . Infant and childhood growth patterns, insulin sensitivity, and blood pressure in prematurely born young adults. Pediatrics 2008;122:313–21.
Flegal KM, Carroll MD, Kit BK, Ogden CL . Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–7.
Hay WW Jr . Strategies for feeding the preterm infant. Neonatology 2008;94:245–54.
Poindexter BB, Langer JC, Dusick AM, Ehrenkranz RA ; National Institute of Child Health and Human Development Neonatal Research Network. Early provision of parenteral amino acids in extremely low birth weight infants: relation to growth and neurodevelopmental outcome. J Pediatr 2006;148:300–5.
Wiedmeier JE, Joss-Moore LA, Lane RH, Neu J . Early postnatal nutrition and programming of the preterm neonate. Nutr Rev 2011;69:76–82.
Freedman DS, Wang J, Thornton JC, et al. Classification of body fatness by body mass index-for-age categories among children. Arch Pediatr Adolesc Med 2009;163:805–11.
Klein S, Allison DB, Heymsfield SB, et al. Waist circumference and cardiometabolic risk: a consensus statement from Shaping America’s Health: Association for Weight Management and Obesity Prevention; NAASO, The Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Am J Clin Nutr 2007;85:1197–202.
Hovi P, Andersson S, Eriksson JG, et al. Glucose regulation in young adults with very low birth weight. N Engl J Med 2007;356:2053–63.
Kay’s SK, Hindmarsh PC . Catch-up growth: an overview. Pediatr Endocrinol Rev 2006;3:365–78.
Li C, Ford ES, Mokdad AH, Cook S . Recent trends in waist circumference and waist-height ratio among US children and adolescents. Pediatrics 2006;118:e1390–8.
Yudkin PL, Aboualfa M, Eyre JA, Redman CW, Wilkinson AR . New birthweight and head circumference centiles for gestational ages 24 to 42 weeks. Early Hum Dev 1987;15:45–52.
Usher R, McLean F . Intrauterine growth of live-born Caucasian infants at sea level: standards obtained from measurements in 7 dimensions of infants born between 25 and 44 weeks of gestation. J Pediatr 1969;74:901–10.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data 2000;314:1–27.
Ong KK, Ahmed ML, Emmett PM, Preece MA, Dunger DB . Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ 2000;320:967–71.
Starfield B, Riley AW, Green BF, et al. The adolescent child health and illness profile. A population-based measure of health. Med Care 1995;33:553–66.
Taylor SJ, Whincup PH, Hindmarsh PC, Lampe F, Odoki K, Cook DG . Performance of a new pubertal self-assessment questionnaire: a preliminary study. Paediatr Perinat Epidemiol 2001;15:88–94.
Acknowledgements
We thank Kathy Winter who coordinated the project and participated in the interview of the parents: Ellen Durand, MA, and Heather Marcinick, MA, research assistants, who tested the children, administered the questionnaires, and measured the subjects; Bonnie Tarantino, BA, who provided clerical assistance; and Bonnie Siner, RN, who provided editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Table S1
(DOC 97 kb)
Supplementary Table S2
(DOC 168 kb)
Supplementary Table S3
(DOC 166 kb)
Supplementary Table S4
(DOC 102 kb)
Supplementary Table S5
(DOC 100 kb)
Supplementary Table S6
(DOC 76 kb)
Supplementary Table S7
(DOC 77 kb)
Supplementary Table S8
(DOC 76 kb)
PowerPoint slides
Rights and permissions
About this article
Cite this article
Hack, M., Schluchter, M., Margevicius, S. et al. Trajectory and correlates of growth of extremely-low-birth-weight adolescents. Pediatr Res 75, 358–366 (2014). https://doi.org/10.1038/pr.2013.209
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2013.209
This article is cited by
-
Pre-pregnancy body mass index, gestational weight gain and postnatal growth in preterm infants
Journal of Perinatology (2021)
-
Growth patterns and body composition in former extremely low birth weight (ELBW) neonates until adulthood: a systematic review
European Journal of Pediatrics (2020)
-
Maternal obesity: a serious pediatric health crisis
Pediatric Research (2018)
-
Reading, Mathematics and Fine Motor Skills at 5 Years of Age in US Children who were Extremely Premature at Birth
Maternal and Child Health Journal (2017)