Abstract
Exposure to a strong T-helper 2 (Th2)-like environment during fetal development may promote allergy development. Increased cord blood (CB) levels of the Th2-associated chemokine CCL22 were associated with allergy development during the first 2 y of life. The aim of the present study was to determine whether CB Th1- and Th2-associated chemokine levels are associated with allergy development during the first 6 y of life, allowing assessment of respiratory allergic symptoms usually developing in this period. The CB levels of cytokines, chemokines, and total IgE were determined in 56 children of 20 women with allergic symptoms and 36 women without allergic symptoms. Total IgE and allergen-specific IgE antibody levels were quantified at 6, 12, 24 mo, and 6 y of age. Increased CB CCL22 levels were associated with development of allergic sensitization and asthma and increased CCL17 levels with development of allergic symptoms, including asthma. Sensitized children with allergic symptoms showed higher CB CCL17 and CCL22 levels and higher ratios between these Th2-associated chemokines and the Th1-associated chemokine CXCL10 than nonsensitized children without allergic symptoms. A pronounced Th2 deviation at birth, reflected by increased CB CCL17 and CCL22 levels, and increased CCL22/CXCL10 and CCL17/CXCL10 ratios might promote allergy development later in life.
Similar content being viewed by others
Main
Maternal allergy may be a more significant risk factor for development of allergic diseases in the offspring than paternal allergy (1,2). The immunological mechanisms behind this phenomenon are unknown, but indicate an impact of the maternal immunity on allergy development, besides the contribution of the genes. The maternal immunity during pregnancy and lactation might influence the neonatal immune development, and the T-helper 2 (Th2)-biased immunity of allergic mothers could possibly modulate the immune responses in their offsprings, to an IgE-favoring, Th2-like phenotype. In line with this, several studies have reported higher cord blood (CB) IgE levels in children of allergic mothers compared with children with paternal or no allergic history (1,3,4).
The discrepant immune response to allergens at birth, observed in children who develop allergic diseases later in life, might be related to exposure to a strong Th2 environment during gestation. For example, a decreased production of allergen-induced IFN-γ by CB mononuclear cells (CBMCs) is associated with allergy development (5,6). Furthermore, the Th1/Th2 balance in vivo has shown to be Th2-biased at birth in children who develop allergic disease later in life (7,8). Increased CB plasma levels of CCL22 were associated with questionnaire-reported wheezing during infancy (7) and development of sensitization and allergic disease during the first 2 y of life (8). Atopic dermatitis (AD) was the predominant symptom of allergic disease during the first 2 y of life in this cohort while the time period between 2 and 6 y of age allows other allergic symptoms, such as asthma and allergic rhinoconjunctivitis (ARC), to develop. Thus, it might not be sufficient to follow the study participants during early infancy only, when searching for predictive factors in CB.
Elevated serum levels of the IL-4- and IL-13-induced chemokines CCL11, CCL17, CCL18, and CCL22 (9–12) have previously been associated with allergic manifestations, in particular AD (13–15). The amplification of the allergic response is partly driven by CCL17 and CCL22 because they attract CCR4 receptor expressing Th2 lymphocytes, mast cells, dendritic cells, and natural killer T (NKT) lymphocytes to the site of inflammation (16). CCL11 binds selectively to the CCR3 receptor, which is expressed on Th2 lymphocytes, mast cells, basophils, and eosinophils (16). CCL18 binds to T lymphocytes (17) but its receptor is not yet known. The IFN-γ-induced chemokines CXCL10 and CXCL11 (18,19) on the other hand bind the CXCR3 receptor expressed on the surface of Th1 lymphocytes, NKT, and mast cells (16). Accordingly, CXCL10 and CXCL11 have been associated with Th1-like diseases like sarcoidosis (20) and Crohn′s disease (21).
Although chemokines have been used as markers for Th1/Th2 immunity in immune-mediated disorders such as allergic disease, little is known about the predictive value of circulating chemokines, before disease onset. Established allergic disease is characterized by a Th2-dominant immunity, but the timing of the development of this Th2 skewing is not known. As this Th2 skewing preceding allergic disease is believed to develop in very early life, we aimed to investigate whether Th1- and Th2-associated cytokine and chemokine levels at birth could serve as markers for future allergy development. To address this question, CB concentrations of the cytokines IL-4, IL-5, IL-9, IL-10, IL-12(p70), IL-13, IFN-γ, and the chemokines CXCL10, CXCL11, CCL11, CCL17, CCL18, and CCL22 were analyzed in relation to allergy development during the first 6 y of life.
METHODS
Study group.
Fifty-six children of 20 women with allergic symptoms and 36 women without allergic symptoms were included in the study (Fig. 1). Due to practical reasons, it was not possible to perform this study, with additional detailed follow-up of the mothers during pregnancy, with a larger number of participants. An experienced allergy research nurse interviewed the mothers regarding their allergic status. Seventeen mothers had ARC, four had asthma (of whom one also had ARC), and two had AD (both of them also had ARC).
Flow-chart of the study participants. Fifty-six women were included in the study. Twenty women reported allergic symptoms of whom 13 were also sensitized, whereas 36 women reported no allergic symptoms of whom 30 were nonsensitized. Nineteen of the 56 children reported allergic symptoms during the first 6 y of life and 27 children reported no symptoms of allergic disease. Ten children dropped out at various time points during childhood and 9 of the remaining 46 children choose to participate with questionnaires only at the 6-y follow-up (marked with Q in the figure). Of the 19 children with allergic symptoms, 11 were also sensitized and 15 of the 27 children without allergic symptoms were nonsensitized. The following numbers of CB samples were available from the analyzed groups, children with allergic symptoms n = 15, children without allergic symptoms n = 22, sensitized children with allergic symptoms n = 8, nonsensitized children without allergic symptoms n = 12. All symp, allergic symptoms; no all symp, no allergic symptoms; sens, sensitized; not sens, not sensitized.
Umbilical CB (n = 46) was collected at birth, and the plasma and serum samples were frozen and stored at −20°C. Maternal and neonatal characteristics are described in detail elsewhere (22).
The children were followed with questionnaires at 3, 6, 12, 18, 24 mo, and 6 y of age regarding environmental factors and allergic symptoms in the children. At 6 and 12 mo of age, a medical examination was performed by an experienced allergy research nurse and at 24 mo and 6 y by a pediatric allergologist. Blood samples were collected at the time of the clinical examinations. The plasma samples were frozen and stored at −20°C.
Three children did not attend the clinical examinations. All the other children (n = 53) attended the 6- and 12-mo examinations, 47 children to the 24-mo examination, and 37 children to the 6 y. Nine children choose to participate with questionnaires only at the 6 y follow-up.
The diagnosis of AD was established using the criteria suggested by Hanifin and Rajka (23), i.e. pruritic, chronic, or chronically relapsing noninfectious dermatitis with typical features and distribution. Asthma, at 6 y of age, was defined as one or more episodes of bronchial obstruction after 2 y of age, at least once verified by a physician. At 2 y of age, asthma was defined as three or more episodes of bronchial obstruction since birth, at least once verified by a physician or two episodes of bronchial obstruction combined with AD or food allergy. Five children were diagnosed with asthma between 0 and 2 y of age, with at least three bronchial obstruction episodes. All the three children diagnosed with asthma between 2 and 6 y of age had experienced more than one episode of bronchial obstruction during this time period. All eight asthmatic children used inhalant corticosteroids, intermittently or continuously. ARC was defined as rhinitis and conjunctivitis appearing at least twice after exposure of an inhalant allergen and not related to infection. Urticaria was defined as allergic if it appeared within 1 h after exposure to a particular allergen, at least at two separate occasions. Symptoms of food allergy were defined as vomiting and/or diarrhea on at least two separate occasions after intake of certain offending food. Oral allergy syndrome was defined as allergic if it appeared at least at two separate occasions after intake of certain offending food. Nineteen children reported allergic symptoms, as described in detail in Table 1. Twenty-seven children reported no symptoms of allergic disease (Fig. 1).
Skin prick tests (SPTs) were performed on the volar aspects of the forearms, with thawed egg white, fresh skimmed cow's milk (lipid concentration 0.5%; 6, 12, 24 mo, and 6 y), cat (12, 24 mo, and 6 y), and birch and timothy (24 mo and 6 y). All extracts were standardized allergen extracts from Allergologisk Laboratorium A/S, (ALK, Soluprick, Hørsholm, Denmark). Histamine hydrochloride (10 mg/mL) was used as positive control, and albumin diluent (ALK) was included as a negative control. The test was regarded as positive when the mean wheal diameter was at least 3 mm. Sixteen of the children had at least 1 positive SPT, 11 to egg, 5 to cat, 5 to timothy, 3 to milk, and 3 to birch. Twenty-five children were not sensitized according to SPT.
The total and allergen-specific IgE concentrations in plasma samples at 6, 12, 24 mo, and 6 y of age were analyzed by ImmunoCAP (Pharmacia Diagnostics, Uppsala, Sweden) according to the manufacturer's instructions. The total IgE levels were also quantified in the CB samples using ImmunoCAP Total IgE Low Range (Phadia, Uppsala, Sweden). The lower detection limit was 0.35 kU/L for the low-range assay and 2 kU/L for the conventional total IgE assay. Specific IgE antibodies directed to common food allergens (egg, milk, fish, wheat, peanut, and soybean) were measured at 6, 12, 24 mo, and 6 y of age with the PhadiatopInfant (Phadia) test. At 6 y of age, specific IgE antibodies to a mix of common inhalant allergens from birch, mugwort, timothy, cat, dog, horse, house dust mite (Dermatophagoides pteronyssinus and farinae), and Cladosporium were measured with the Phadiatop (Phadia) test. The cutoff for positivity was 0.35 kUA/L for the PhadiatopInfant and the Phadiatop test. Eighteen children were sensitized according to the PhadiatopInfant (n = 17) and the Phadiatop test (n = 11, of whom 10 were also sensitized according to the PhadiatopInfant test). Twenty-one children showed allergen-specific IgE levels below the cutoff for positivity.
Eleven of the 19 children with allergic symptoms were sensitized (according to SPT and/or circulating allergen-specific IgE antibodies). Eight of these sensitized children with allergic symptoms had AD, six of them also had asthma, and three of these six children also had urticaria, and one child had AD and urticaria. Three children had ARC of whom one child also had AD and one child had AD, asthma, and urticaria combined with ARC. One child had symptoms of food allergy and one child experienced obstructive discomfort after intake of certain offending food. Two of the three children with allergic symptoms who participated with questionnaires only at the 6-y follow-up are included in the group of sensitized children with allergic symptoms as well. These children visited the allergy clinic very often. The diagnosis of these two children were based on notes in the medical records and SPTs performed within the clinical practice. One child had AD at the age of 4 y, although without any sensitization. At 6 y of age, the AD had regressed and the child was sensitized to inhalant allergens (Phadiatop test). This child is included in the group of sensitized children and in the group of children with allergic symptoms but not in the group of sensitized children with allergic symptoms, because the allergic symptom and sensitization was completely unrelated to each other. Fifteen children were nonsensitized without allergic symptoms.
Determination of CB cytokine and chemokine concentrations.
The CB levels of IL-4, IL-5, IL-9, IL-10, IL-12(p70), IL-13, IFN-γ, CCL11, CXCL10, and CCL22 were quantified by a multiplex assay (Luminex100, Biosource, Nivelles, Belgium) using the Beadlyte Human Multi-Cytokine Beadmaster Kit (Upstate, CA), as described in detail elsewhere (8). All measurements were blinded to the clinical symptoms.
Determination of CB CCL17, CCL18, and CXCL11 concentrations by ELISA.
An in-house double-antibody sandwich ELISA (VersaMax, Molecular Devices, Sunnyvale, CA) was used for quantification of CB chemokines, as described in detail elsewhere (8).
Statistics.
Nonparametric tests, corrected for ties, were used. The correlations were analyzed with Spearman's rank order correlation coefficient test. Comparisons between unpaired groups were done with the Mann-Whitney U test. The calculations were made with the statistical package SPSS 15.0 for Windows (SPSS, Inc., Chicago, IL). Undetectable levels were given the value of half the cutoff.
Logistic regression was used to investigate if CB IgE, CXCL10, CCL17, and CCL22 predicted the cumulative occurrence of allergic symptoms, sensitization (SPT and/or presence of allergen-specific IgE antibodies), and allergic symptoms combined with sensitization during the first 6 y of life. The logistic regression was performed using Minitab 15 (Minitab, Inc., State College, PA).
Ethics.
The Regional Ethics Committee for Human Research at the University Hospital of Linköping approved the study. All families gave their informed consent.
RESULTS
Increased CB CCL22 levels, but not CCL17 levels, are associated with development of allergic sensitization later in life.
The CB levels of IL-4, IL-5, IL-9, IL-10, IL-12(p70), IL-13, IFN-γ, CXCL10, CXCL11, CCL11, CCL17, CCL18, and CCL22 were analyzed in relation to development of allergic sensitization during the first 6 y of life. The cytokines were not detectable, or only sporadically detectable, in the CB samples.
Sensitized children (with positive SPT and/or presence of circulating allergen-specific IgE antibodies) had higher CB CCL22 levels (Fig. 2A) and CCL22/CXCL10 ratios (Fig. 2B) than nonsensitized children. The levels of CCL17 (Fig. 2C) and the other chemokines were similar between the two groups. Furthermore, CB CCL22 levels predicted development of allergic sensitization during the first 6 y of life (OR = 1.14; 95% CI = 1.03–1.26; p = 0.02) based on 100-pg/mL intervals. Neonatal IgE, CCL17 and, in particular, CCL22 levels, were correlated to the total IgE levels later in life (Table 2).
CB CCL22, CCL22/CXCL10 ratio, and CCL17 levels in sensitized and nonsensitized children. (A) Sensitized children (with positive SPT and/or circulating allergen-specific IgE antibodies, n = 15) during the first 6 y of life showed increased CB CCL22 levels and (B) CCL22/CXCL10 ratios compared with nonsensitized children (n = 17). SPT and circulating IgE antibodies were performed/measured at 6, 12, 24 mo, and 6 y of age. (C) The CB levels of CCL17 were similar in the sensitized and nonsensitized children. * = p < 0.05, ** = p < 0.01.
Increased CB CCL17 levels, but not CCL22 levels, are associated with development of allergic symptoms later in life.
Development of allergic symptoms during the first 6 y of life was associated with high CB CCL17 levels (Fig. 3A) and high CCL17/CXCL10 ratios (p = 0.01). Even though a weak relationship between CB CCL22 levels and development of allergic symptoms was seen (Fig. 3B), a significantly increased CCL22/CXCL10 ratio (p = 0.03) was observed in the group of children who developed allergic symptoms. The CB CCL17 levels predicted development of allergic symptoms during the first 6 y of life (OR = 1.27; 95% CI = 1.01–1.59; p = 0.04) for a 100 pg/mL increase in CCL17.
CB CCL17 and CCL22 levels in children with and without allergic symptoms. (A) Increased CB CCL17 levels were shown in the group of children with allergic symptoms (n = 15) compared with children without allergic symptoms (n = 22). (B) Children who reported allergic symptoms during the first 6 y of life showed a trend to higher levels of CB CCL22 as the children without allergic symptoms. ‡ = p < 0.1, ** = p < 0.01.
Asthma development was associated with increased CB CCL17, CCL22, and CCL22/CXCL10 ratio (p = 0.04 for all comparisons). The same pattern was shown for the development of asthma and/or ARC, p = 0.003 for CB CCL17 and p = 0.007 for the CB CCL22 levels, p = 0.01 for the CCL17/CXCL10, and p = 0.03 for the CCL22/CXCL10 ratios. Increased CB IgE levels tended to be associated with development of asthma and/or ARC (p = 0.07). Development of AD was associated with high CB CCL17 (p = 0.02) levels, CCL17/CXCL10 (p = 0.01), and CCL22/CXCL10 (p = 0.02) ratios.
Increased CB CCL17 and CCL22 levels are associated with development of allergic symptoms and sensitization during the first 6 y of life.
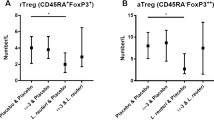
The sensitized children with allergic symptoms had higher CB CCL17 and CCL22 levels than nonsensitized children without allergic symptoms (Fig. 4).
CB CCL17 and CCL22 levels in sensitized children with allergic symptoms and nonsensitized children without allergic symptoms. Increased CB CCL17 and CCL22 levels are associated with development of allergic symptoms and sensitization. The sensitized children with allergic symptoms (n = 8) showed increased (A) CB CCL17 and (B) CCL22 levels compared with nonsensitized children without allergic symptoms (n = 12). * = p < 0.05.
The Th1/Th2 balance was shifted toward a more Th2-like profile as well, because the ratios of CCL17/CXCL10 and CCL22/CXCL10 were higher in sensitized children with allergic symptoms than nonsensitized children without allergic symptoms (p = 0.04 and p = 0.005, respectively). Increased CB IgE levels tended to be associated with development of allergic symptoms combined with sensitization as well (p = 0.09). The levels of CXCL10, CXCL11, CCL11, and CCL18 were similar in the two groups.
Possible confounders, i.e. older siblings, gender, and smoking during pregnancy, did not affect the CB chemokine levels in this cohort (Mann-Whitney U-test). CCL11, CCL17, CCL18, CCL22, and CXCL11 levels were not affected by the mode of delivery but children delivered by cesarean section showed lower CXCL10 levels compared with the children which were born vaginally (p = 0.04). Fifty percent of the children delivered by cesarean section (n = 10) and 39% of the children delivered vaginally developed allergic symptoms during the first 6 y of life.
DISCUSSION
Circulating levels of the Th2-associated chemokines CCL17 and CCL22 at birth might be important for the immune development later in life. Thus, increased CB CCL17 levels were associated with development of allergic symptoms, with and without accompanying sensitization during the first 6 y of life, whereas elevated CB CCL22 levels were seen in children who develop sensitization, with and without accompanying allergic symptoms. Our results clearly indicate that high CCL17 and CCL22 levels at birth could affect the offspring postnatally. CB CCL17 levels predicted development of allergic symptoms and CB CCL22 levels predicted development of allergic sensitization later in life. If CCL17 and CCL22 are actively involved in the initiation of the disease, or if increased CCL17 and CCL22 levels are markers for a general, stronger Th2 shift at birth in these children remains to be settled.
A possible mechanism for the contribution of CCL22 in allergy development could be the increased IgE production seen up to 2 y of age. Children with a more marked Th2 deviation at birth might experience difficulties in the down-regulation of Th2 responses, possibly causing a delayed maturation of the immune system. A continued Th2 dominance during infancy might stimulate IgE synthesis and promote allergy development. A prolonged Th2 dominance in the immune responses to allergens has been associated with allergy development (24,25). We did observe a relationship between CB CCL22 levels and total IgE levels during the first 2 y of age, while a corresponding relationship between CB IgE, CB CCL17, and future total IgE levels was observed at 6 mo of age only. The rho values indicated moderate correlations. As CB CCL17 levels were associated with development of allergic symptoms, but not sensitization only, it is tempting to speculate that CB CCL17 and CCL22 contribute to development of allergic disease through different mechanisms, despite the similarities of these two chemokines. CCL17 and CCL22 share 32% sequence homology (26) and are both induced by IL-4 and IL-13 (9,10). They also bind to the same receptor, CCR4 (16).
The present study confirms and extends our previous data on CB CCL22 and development of sensitization and allergic disease up to 2 y of age. AD is the predominant symptom of allergic disease during the first 2 y of life and the time period between 2 and 6 y of age allows other allergic symptoms, such as asthma and ARC, to develop. Thus, it is very interesting to demonstrate a relationship between a pronounced Th2 deviation at birth, shown as increased CB CCL17 and CCL22 levels, and development of allergic symptoms and sensitization up to 6 y of age. Our study did not reveal any relationship between CCL11, CCL18, CXCL10, and CXCL11 levels, and allergy development. We cannot exclude the possible influence of the present study size on these negative findings, because our population may have been too small to reveal such relationship.
CB IgE has been evaluated as a potential predictor of elevated IgE levels and development of allergic disease later in life (27,28). However, the use of CB IgE as a predictor has been limited because of poor sensitivity (27–29). Although our findings need to be confirmed in a larger number of samples, CB CCL22 may possibly be an attractive candidate as a predictor of elevated IgE levels and future allergy development. We did observe correlations between CB CCL22 and total IgE levels up to 2 y of age and a corresponding correlation between CB IgE and total IgE levels up to 6 mo of age. Furthermore, CCL22, in contrast to IgE, is easily detected in CB. In the present study, CCL22 was detected in all CB samples, while only 12 (26%) of the 46 CB samples had detectable levels of total IgE. The CB levels of CCL22 are, in fact, ∼20 times higher than adult levels (unpublished data), thereby also reducing the impact of contamination of the CB samples with maternal blood. It should also be noted that cytokine levels were too low to be safely detected in CB and therefore not suitable for prediction of allergy development.
In conclusion, children who develop allergic symptoms and sensitization during the first 6 y of life showed increased CCL17 and CCL22 levels already in CB compared with children who remained nonallergic, indicating that the Th2 deviation preceding established allergy takes place very early in life.
Abbreviations
- AD:
-
atopic dermatitis
- ARC:
-
allergic rhinoconjunctivitis
- CB:
-
cord blood
- SPT:
-
skin prick test
- Th:
-
T-helper
References
Liu CA, Wang CL, Chuang H, Ou CY, Hsu TY, Yang KD 2003 Prenatal prediction of infant atopy by maternal but not paternal total IgE levels. J Allergy Clin Immunol 112: 899–904
Ruiz RG, Kemeny DM, Price JF 1992 Higher risk of infantile atopic dermatitis from maternal atopy than from paternal atopy. Clin Exp Allergy 22: 762–766
Johnson CC, Ownby DR, Peterson EL 1996 Parental history of atopic disease and concentration of cord blood IgE. Clin Exp Allergy 26: 624–629
Magnusson CG 1988 Cord serum IgE in relation to family history and as predictor of atopic disease in early infancy. Allergy 43: 241–251
Kondo N, Kobayashi Y, Shinoda S, Takenaka R, Teramoto T, Kaneko H, Fukao T, Matsui E, Kasahara K, Yokoyama Y 1998 Reduced interferon gamma production by antigen-stimulated cord blood mononuclear cells is a risk factor of allergic disorders—6-year follow-up study. Clin Exp Allergy 28: 1340–1344
van der Velden VH, Laan MP, Baert MR, de Waal Malefyt R, Neijens HJ, Savelkoul HF 2001 Selective development of a strong Th2 cytokine profile in high-risk children who develop atopy: risk factors and regulatory role of IFN-gamma, IL-4 and IL-10. Clin Exp Allergy 31: 997–1006
Leung TF, Ng PC, Tam WH, Li CY, Wong E, Ma TP, Lam CW, Fok TF 2004 Helper T-lymphocyte-related chemokines in healthy newborns. Pediatr Res 55: 334–338
Sandberg M, Frykman A, Ernerudh J, Berg G, Matthiesen L, Ekerfelt C, Nilsson LJ, Jenmalm MC 2009 Cord blood cytokines and chemokines and development of allergic disease. Pediatr Allergy Immunol 20: 519–527
Andrew DP, Chang MS, McNinch J, Wathen ST, Rihanek M, Tseng J, Spellberg JP, Elias CG 3rd 1998 STCP-1 (MDC) CC chemokine acts specifically on chronically activated Th2 lymphocytes and is produced by monocytes on stimulation with Th2 cytokines IL-4 and IL-13. J Immunol 161: 5027–5038
Nomura T, Terada N, Kim WJ, Nakano K, Fukuda Y, Wakita A, Numata T, Konno A 2002 Interleukin-13 induces thymus and activation-regulated chemokine (CCL17) in human peripheral blood mononuclear cells. Cytokine 20: 49–55
Terada N, Hamano N, Nomura T, Numata T, Hirai K, Nakajima T, Yamada H, Yoshie O, Ikeda-Ito T, Konno A 2000 Interleukin-13 and tumour necrosis factor-alpha synergistically induce eotaxin production in human nasal fibroblasts. Clin Exp Allergy 30: 348–355
van Lieshout AW, van der Voort R, le Blanc LM, Roelofs MF, Schreurs BW, van Riel PL, Adema GJ, Radstake TR 2006 Novel insights in the regulation of CCL18 secretion by monocytes and dendritic cells via cytokines, toll-like receptors and rheumatoid synovial fluid. BMC Immunol 7: 23
Günther C, Bello-Fernandez C, Kopp T, Kund J, Carballido-Perrig N, Hinteregger S, Fassl S, Schwärzler C, Lametschwandtner G, Stingl G, Biedermann T, Carballido JM 2005 CCL18 is expressed in atopic dermatitis and mediates skin homing of human memory T cells. J Immunol 174: 1723–1728
Jahnz-Rozyk K, Targowski T, Paluchowska E, Owczarek W, Kucharczyk A 2005 Serum thymus and activation-regulated chemokine, macrophage-derived chemokine and eotaxin as markers of severity of atopic dermatitis. Allergy 60: 685–688
Nakazato J, Kishida M, Kuroiwa R, Fujiwara J, Shimoda M, Shinomiya N 2008 Serum levels of Th2 chemokines, CCL17, CCL22, and CCL27, were the important markers of severity in infantile atopic dermatitis. Pediatr Allergy Immunol 19: 605–613
Pease JE, Williams TJ 2006 Chemokines and their receptors in allergic disease. J Allergy Clin Immunol 118: 305–318
Hieshima K, Imai T, Baba M, Shoudai K, Ishizuka K, Nakagawa T, Tsuruta J, Takeya M, Sakaki Y, Takatsuki K, Miura R, Opdenakker G, Van Damme J, Yoshie O, Nomiyama H 1997 A novel human CC chemokine PARC that is most homologous to macrophage-inflammatory protein-1 alpha/LD78 alpha and chemotactic for T lymphocytes, but not for monocytes. J Immunol 159: 1140–1149
Cole KE, Strick CA, Paradis TJ, Ogborne KT, Loetscher M, Gladue RP, Lin W, Boyd JG, Moser B, Wood DE, Sahagan BG, Neote K 1998 Interferon-inducible T cell alpha chemoattractant (I-TAC): a novel non-ELR CXC chemokine with potent activity on activated T cells through selective high affinity binding to CXCR3. J Exp Med 187: 2009–2021
Luster AD, Ravetch JV 1987 Biochemical characterization of a gamma interferon-inducible cytokine (IP-10). J Exp Med 166: 1084–1097
Miotto D, Christodoulopoulos P, Olivenstein R, Taha R, Cameron L, Tsicopoulos A, Tonnel AB, Fahy O, Lafitte JJ, Luster AD, Wallaert B, Mapp CE, Hamid Q 2001 Expression of IFN-gamma-inducible protein; monocyte chemotactic proteins 1, 3, and 4; and eotaxin in TH1- and TH2-mediated lung diseases. J Allergy Clin Immunol 107: 664–670
Singh UP, Singh S, Iqbal N, Weaver CT, McGhee JR, Lillard JW Jr 2003 IFN-gamma-inducible chemokines enhance adaptive immunity and colitis. J Interferon Cytokine Res 23: 591–600
Sandberg M, Frykman A, Jonsson Y, Persson M, Ernerudh J, Berg G, Matthiesen L, Ekerfelt C, Jenmalm MC 2009 Total and allergen-specific IgE levels during and after pregnancy in relation to maternal allergy. J Reprod Immunol 81: 82–88
Hanifin JM, Rajka G 1980 Diagnostic features of atopic dermatitis. Acta Derm Venereol (Stockholm) 92: 44–47
Böttcher MF, Jenmalm MC, Björksten B 2002 Immune responses to birch in young children during their first 7 years of life. Clin Exp Allergy 32: 1690–1698
Prescott SL, Macaubas C, Smallacombe T, Holt BJ, Sly PD, Holt PG 1999 Development of allergen-specific T-cell memory in atopic and normal children. Lancet 353: 196–200
Godiska R, Chantry D, Raport CJ, Sozzani S, Allavena P, Leviten D, Mantovani A, Gray PW 1997 Human macrophage-derived chemokine (MDC), a novel chemoattractant for monocytes, monocyte-derived dendritic cells, and natural killer cells. J Exp Med 185: 1595–1604
Hansen LG, Halken S, Host A, Moller K, Osterballe O 1993 Prediction of allergy from family history and cord blood IgE levels. A follow-up at the age of 5 years. Cord blood IgE. IV. Pediatr Allergy Immunol 4: 34–40
Kjellman NI, Croner S 1984 Cord blood IgE determination for allergy prediction–a follow-up to seven years of age in 1,651 children. Ann Allergy 53: 167–171
Pesonen M, Kallio MJ, Siimes MA, Elg P, Bjorksten F, Ranki A 2009 Cord serum immunoglobulin E as a risk factor for allergic symptoms and sensitization in children and young adults. Pediatr Allergy Immunol 20: 12–18
Acknowledgements
We thank the families who participated in the study, the midwives at the maternity health care clinic, and the staff in the delivery room. We also thank Anne-Marie Fornander, research nurse Lena Lindell for excellent technical assistance, and Olle Eriksson, Department of Mathematics, Linköping University, Sweden, for valuable help with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Swedish Research Council (project 73X-15335-01A and 74X-20146-01-2), the National Swedish Association against Allergic Diseases, the National Heart and Lung Association, The Vardal Foundation—for Health Care Sciences and Allergy Research, Samariten Foundation, Queen Silvia Research Foundation, and the County Council of Östergötland.
The authors report no conflicts of interest.
Rights and permissions
About this article
Cite this article
Abelius, M., Ernerudh, J., Berg, G. et al. High Cord Blood Levels of the T-Helper 2-Associated Chemokines CCL17 and CCL22 Precede Allergy Development During the First 6 Years of Life. Pediatr Res 70, 495–500 (2011). https://doi.org/10.1203/PDR.0b013e31822f2411
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31822f2411
This article is cited by
-
Low Mother-to-Child CCL22 Chemokine Levels Are Inversely Related to Mite Sensitization and Asthma in Early Childhood
Scientific Reports (2018)
-
Immune Alterations in CD8+ T Cells Are Associated with Neuronal C-C and C-X-C Chemokine Receptor Regulation Through Adenosine A2A Receptor Signaling in a BTBR T+ Itpr3tf/J Autistic Mouse Model
Molecular Neurobiology (2018)
-
Effect of camel milk on thymus and activation-regulated chemokine in autistic children: double-blind study
Pediatric Research (2014)
-
Elevated serum levels of macrophage-derived chemokine and thymus and activation-regulated chemokine in autistic children
Journal of Neuroinflammation (2013)
-
CCR4 Agonists CCL22 and CCL17 are Elevated in Pediatric OMS Sera: Rapid and Selective Down-Regulation of CCL22 by ACTH or Corticosteroids
Journal of Clinical Immunology (2013)