Abstract
Infants with hemolytic diseases frequently develop hyperbilirubinemia and are treated with phototherapy, which only eliminates bilirubin after its production. A better strategy might be to directly inhibit heme oxygenase (HO), the rate-limiting enzyme in bilirubin production. Metalloporphyrins (Mps) are heme analogs that competitively inhibit HO activity in vitro and in vivo and suppress plasma bilirubin levels in vivo. A promising Mp, zinc deuteroporphyrin bis glycol (ZnBG), is orally absorbed and effectively inhibits HO activity at relatively low doses. We determined the I50 (the dose needed to inhibit HO activity by 50%) of orally administered ZnBG in vivo and then evaluated ZnBG's effects on in vivo bilirubin production, HO activity, HO protein levels, and HO-1 gene expression in newborn mice after heme loading, a model analogous to a hemolytic infant. The I50 of ZnBG was found to be 4.0 μmol/kg body weight (BW). At a dose of 15 μmol/kg BW, ZnBG reduced in vivo bilirubin production, inhibited heme-induced liver HO activity and spleen HO activity to and below baseline, respectively, transiently induced liver and spleen HO-1 gene transcription, and induced liver and spleen HO-1 protein levels. We conclude that ZnBG may be an attractive compound for treating severe neonatal hyperbilirubinemia caused by hemolytic disease.
Similar content being viewed by others
Main
The degradation of heme to biliverdin by heme oxygenase (HO) is the rate-limiting step in the production of bilirubin (1). HO degrades heme to produce equimolar amounts of carbon monoxide (CO), iron, and biliverdin, which is rapidly reduced to bilirubin by biliverdin reductase. Because bilirubin production is two to three times higher in a newborn compared with an adult on a body weight (BW) basis (2), and the newborn liver has an immature ability to conjugate and therefore excrete bilirubin, bilirubin can accumulate to excessive levels in the circulation and cause neonatal hyperbilirubinemia.
Infant risk factors for hyperbilirubinemia include prematurity, maternal diabetes, and hemolytic conditions such as glucose-6-phosphate dehydrogenase (G6PD) deficiency, Rh/ABO blood incompatibilities, and closed-space bleeding (3,4). If left untreated, neonatal hyperbilirubinemia can become severe and lead to bilirubin-induced neurologic dysfunction (BIND) or, rarely, permanent irreversible brain injury called kernicterus (5).
Phototherapy and exchange transfusion remain the most common strategies for treating neonatal hyperbilirubinemia, but these approaches only eliminate bilirubin after it has been produced. Moreover, recent evidence suggests that aggressive phototherapy might increase the mortality of extremely LBW (ELBW) infants (6), further emphasizing the need for alternative treatment methods including pharmacological approaches to prevent the bilirubin production and to reduce bilirubin levels in this high-risk group.
Various compounds have been proposed as potential chemopreventive treatments for hyperbilirubinemia, but the most promising are the metalloporphyrins (Mps), which are heme analogs that contain a central metal such as tin, zinc, or chromium, and a porphyrin ring (3,7). Maines (8) and Drummond and Kappas (9) originally reported that Mps, such as zinc and tin protoporphyrins, inhibit HO activity in the liver.
We have also been investigating Mps and have concluded that besides tin mesoporphyrin (SnMP), zinc protoporphyrin, chromium mesoporphyrin (CrMP), and zinc deuteroporphyrin bis glycol (ZnBG) are promising Mps for use in treating neonates with severe hyperbilirubinemia (4,10). We believe that an ideal antihyperbilirubinemic drug should be potent, short acting, not phototoxic, not affect other important enzymes such as NOS and soluble guanylate cyclase (sGC), and not induce HO-1 gene expression (11). We have found that SnMP, which has been used in human trials, has high inhibitory potency (12) but may be photoreactive at therapeutic doses (3,7). SnMP also affects NOS and sGC and induces HO-1 expression, further limiting its clinical use (3,11,13). CrMP and ZnBG are also highly potent (12) and orally absorbable, but minimally affect NOS and sGC (14) and may be less phototoxic than SnMP at effective doses (11,15), suggesting that CrMP and ZnBG may be attractive alternative Mps to SnMP (16).
We have previously shown that in vivo, successive exposures of adult mice to 30 μmol heme/kg BW effectively increase HO activity in the liver and spleen at least 2-fold (17) and thus can be used as an animal model to study the hemolytic condition (3). In this study, we first determined the dose of ZnBG needed to inhibit in vivo HO activity by 50% (I50) in 1-wk-old mice. We then evaluated the effects of ZnBG on bilirubin production, HO activity, HO-1 mRNA, and protein levels in a heme-loaded newborn mouse model that simulates a hemolytic infant, who has a high risk of developing hyperbilirubinemia.
MATERIALS AND METHODS
Animals.
For these studies, 1-, 3-, and 5-wk-old FVB mice were used. Animal use for this study was approved by Stanford University's Institutional Animal Care and Use Committee. One-week-old mice were kept with their mothers.
Reagents.
A stock solution of 4 mM ZnBG was prepared by dissolving 4.72 mg of ZnBG (Frontier Scientific, Logan, UT) in 60 μL of 0.4 M Na3PO4 and adding 250 μL deionized water. The pH was titrated to 7.4 with ∼25 μL 1 N HCl, and the final volume was adjusted to 1.70 mL with saline (0.9% NaCl). A 2 mM solution of ZnBG was prepared by diluting the stock solution with saline.
A 4.5 mM solution of reduced nicotinamide adenine dinucleotide phosphate (NADPH; Calbiochem, La Jolla, CA) was prepared by dissolving 3.82 mg of Na4NADPH in 1.0 mL of 0.1 M KPO4.
Stock solutions of MHA—a 1.5 mM stock solution used for the HO activity assay and 4.00 mM used for s.c. injection—were prepared as previously described (3). For the HO activity assay, a working solution of 150 μM MHA was prepared daily by diluting the stock solution with 0.1 M KPO4.
ZnBG at doses of 3.75, 7.5, 15, or 30 μmol/kg BW, or an equal volume of vehicle (saline), was administered by oral gavage (OG) using a 1-mL insulin syringe attached to a 29-gauge needle covered with soft polyethylene tubing. Approximately 30 μmol/kg BW of heme (MHA), or an equal volume of vehicle, was administered s.c. using a 0.5-mL insulin syringe fitted with a 30-gauge needle. None of the injection volumes exceeded 50 μL.
Tissue preparation.
After mice were killed, livers, brains, and spleens were harvested and rinsed with ice-cold 0.1 M KPO4. One hundred milligrams of each tissue was placed into a 1.5-mL microfuge tube. Liver and brain tissues were diluted 10× with 0.1 M KPO4. Spleen tissues were diluted 15× with 0.1 M KPO4. Tissues were sonicated at 50% power with a Microson Ultrasonic Cell Disruptor (Misonix, Farmingdale, NY).
In vitro HO activity.
Because equimolar quantities of CO and bilirubin are produced during heme degradation, the production of CO in the presence of heme and NADPH in tissue sonicates can be used as an index of HO activity (18). Twenty microliters of sonicate (representing 2 mg of liver and brain or 1.33 mg of spleen) was incubated with 20 μL of 4.5 mM NAPDH and 20 μL of 150 μM MHA for 15 min at 37°C in septum-sealed 2 mL amber vials (18,19). Reactions were terminated with the addition of 5 μL of 15% sulfosalicylic acid. CO generated by the reaction into the vial headspace was quantitated using gas chromatography with a Reduction Gas Analyzer (RGA-2, Peak Laboratories LLC, Mountain View, CA). HO activity was calculated as pmoles CO/h/mg fresh weight (FW) and expressed as the percent of HO activity remaining compared with age-matched control levels.
Total body CO excretion rate (VeCO).
In vivo bilirubin production rates (or VeCO) were measured by placing the 1-wk-old mice in 15 mL acrylic chambers supplied with 10 to 15 mL of air/min for a maximum of 6 h (4). CO concentrations in the outlet air were quantified using gas chromatography. VeCO were calculated as μL CO/h/kg BW, normalized to baseline levels, and expressed as fold change from baseline (mean ± SD).
Western blots.
Following standard laboratory procedure, 50 μg of liver, spleen, or brain protein was mixed with equal volumes of 2× loading buffer (3). Samples were applied to a 12% polyacrylamide gel, separated using electrophoresis, and transferred to polyvinylidene fluoride (PVDF) membrane (Bio-Rad, Hercules, CA). HO-1 and HO-2 proteins were detected, immunocomplexes were visualized, and signals were quantified as previously described (3). Results were expressed as fold change (mean ± SD) from protein levels of age-matched vehicle-treated control animals.
RT-PCR.
Approximately, 5 × 5 × 1 mm pieces of liver, spleen, and brain were taken immediately after sacrifice, placed in RNAlater (Qiagen, Valencia, CA), and stored at −80°C until use. Total RNA was extracted and HO-1 mRNA was measured by RT-PCR according to standard laboratory procedure, using the RNAeasy Mini Kit (Qiagen) and a Mx-3005 Quantitative PCR System (Stratagene, Cedar Creek, TX) (3). All results were normalized to 5 β-actin mRNA levels in the same tissues and expressed as fold change (mean ± SD) from baseline levels.
Statistical analyses.
Statistical significance was calculated using unpaired, two-tailed t tests, with differences deemed significant when p ≤ 0.05.
Determination of I50.
One-week-old mice were given vehicle, 3.75, 7.5, 15, or 30 μmol/kg BW of ZnBG by OG. Because we have previously reported that maximum inhibition of HO activity by 30 μmol ZnBG/kg BW occurs 3 h after oral administration (3), HO activity was quantitated in liver, spleen, and brain at this time point. The I50 was determined using interpolation.
Determination of ZnBG effectiveness after heme loading.
Although ZnBG is most effective at 3 h after administration (3), hemolysis in infants can be unpredictable or ongoing, and so a single dose of ZnBG should ideally mitigate hemolytic insults occurring more than 3 h after ZnBG administration. As such, to model a more persistent hemolytic condition and extend the efficacy of ZnBG, we administered a higher dose (15 μmol ZnBG/kg BW) between two heme loads and measured HO activity 24 h after the second heme load, i.e. 48 h after ZnBG administration (Fig. 1).
Heme-loaded study design. After administration of the first heme load or vehicle at t = 0 h, VeCO was monitored for up to 6 h to assess the effect of a single heme load on in vivo bilirubin production. At t = 24 h, 15 μmol ZnBG/kg BW or vehicle was administered OG. At t = 48 h, a second heme load or vehicle was administered, and VeCO was again monitored for up to 6 h. An additional set of liver and spleen tissues from mice treated with the V-V-V or H-Zn-H regimen was harvested at t = 54 h for measurements of HO-1 mRNA levels. At t = 72 h, VeCO was again measured. Mice were then killed, and liver, spleen, and brain tissues were harvested for HO activity, HO-1 mRNA, and HO protein levels.
At t = −24 h, baseline in vivo bilirubin production was measured. Mice were randomly assigned to the following three treatment groups:
-
a
Vehicle-treated controls (V-V-V): vehicle given at t = 0, 24, and 48 h.
-
b
Heme controls (H-V-H): heme given at t = 0 h, vehicle at t = 24 h, and heme at t = 48 h.
-
c
ZnBG-treated (H-Zn-H): heme given at t = 0 h, 15 μmol ZnBG/kg BW at t = 24 h, and heme at t = 48 h.
At t = 0 h, 30 μmol heme/kg BW or vehicle was administered via s.c., and VeCO was monitored for up to 6 h to assess the effect of a single heme load on bilirubin production. At t = 24 h, 15 μmol ZnBG/kg BW or vehicle was administered via OG. At t = 48 h, a second 30 μmol heme/kg BW dose or vehicle was administered via s.c., and VeCO was monitored for up to 6 h to assess the effect of the ZnBG on bilirubin production after a second heme load. A separate set of animals treated with V-V-V, H-V-H, or H-Zn-H was used to assess HO-1 mRNA levels in the liver and spleen at t = 54 h, or 6 h after the second heme load. At t = 72 h, VeCO was again measured. Animals were then killed, and liver, spleen, and brain tissues were harvested for in vitro assays of HO activity, HO-1 mRNA levels, and HO protein levels.
RESULTS
Determination of ZnBG I50.
At 3 h after administration of vehicle, liver HO activity was 186 ± 25 pmol CO/h/mg FW (n = 16) (Fig. 2A). Administration of 3.75-, 7.5-, 15-, or 30-μmol ZnBG/kg BW by OG resulted in significant inhibition of HO activity to 97 ± 1 (48% inhibition), 73 ± 2 (61%), 71 ± 9 (62%), and 61 ± 8 (67%) pmol CO/h/mg FW, respectively (n = 3 at each ZnBG dose). Interpolation of these results revealed that the I50 was ∼4.0 μmol/kg BW. No significant inhibition on spleen (Fig. 2B) or brain (Fig. 2C) HO activity was found at any dose.
HO activity after treatment with various doses of ZnBG. Liver (A), spleen (B), and brain (C) HO activity was measured 3 h after oral administration with 3.75, 7.5, 15, and 30 μmol ZnBG/kg BW to 1-wk-old mice. Data are expressed as %HO activity (mean ± SD), n ≥ 3 mice for each treatment group. *p ≤ 0.05 compared with the control levels.
Effectiveness of ZnBG after heme loading
Bilirubin production.
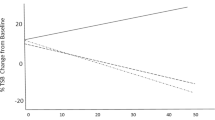
No change in the rates of total body CO production, an index of in vivo bilirubin production, was observed in the V-V-V group (Fig. 3). After a second heme load (H-V-H), bilirubin production significantly increased to a maximum of 4.5-fold in 2.5 h. In mice treated with 15 μmol ZnBG/kg BW (H-Zn-H), the peak heme-induced fold change was significantly reduced by 19% (p ≤ 0.05). For all groups, bilirubin production rates returned to baseline by the next day.
Effects of heme and heme/ZnBG on bilirubin production. In vivo bilirubin production rates of control ( ), (V-V-V), heme-loaded (▴), (H-V-H), and heme-loaded and ZnBG-treated (▪) (H-Zn-H, 15 μmol ZnBG/kg BW) mice were measured after a second heme load, with peak levels measured in H-Zn-H-treated mice averaged and compared with the average peak level of all H-V-H-treated mice. Data are expressed as fold change from baseline (mean ± SD), n ≥ 5 mice for each treatment group. *p ≤ 0.05.
), (V-V-V), heme-loaded (▴), (H-V-H), and heme-loaded and ZnBG-treated (▪) (H-Zn-H, 15 μmol ZnBG/kg BW) mice were measured after a second heme load, with peak levels measured in H-Zn-H-treated mice averaged and compared with the average peak level of all H-V-H-treated mice. Data are expressed as fold change from baseline (mean ± SD), n ≥ 5 mice for each treatment group. *p ≤ 0.05.
HO activity.
When HO activity was measured at 24 h after a second heme load, liver HO activity in the V-V-V group was found to be 220 ± 19 pmol CO/h/mg FW (n = 5). Liver HO activity in the H-V-H group was significantly increased by 45% (319 ± 35 pmol CO/h/mg FW, n = 5) over control levels, as expected (Fig. 4A). In mice treated with 15 μmol ZnBG/kg BW (H-Zn-H), the heme-induced increase in liver HO activity was completely suppressed to 232 ± 9 pmol CO/h/mg FW (n = 5), or 105% of control levels.
Effects of heme and heme/ZnBG on HO activity. HO activity (mean ± SD) in the liver (A), spleen (B), and brain (C) of control (V-V-V), heme-loaded (H-V-H), and heme-loaded and ZnBG-treated (H-Zn-H, 15 μmol ZnBG/kg BW) mice was measured 24 h after a second heme load. Data are expressed as %HO activity (mean ± SD), n ≥ 5 mice for each treatment group. *p ≤ 0.05 compared with V-V-V levels; †p ≤ 0.05 compared with H-V-H levels.
In the spleen, there was no significant increase in HO activity in the H-V-H group (Fig. 4B), with an H-V-H activity level of 446 ± 30 pmol CO/h/mg FW (n = 5) compared with the V-V-V level of 401 ± 82 pmol CO/h/mg FW (n = 5). After ZnBG treatment (H-Zn-H), HO activity was significantly inhibited by 35% (compared with H-V-H) to 288 ± 44 pmol CO/h/mg FW (n = 5) or 70% of control (V-V-V) levels. No change in HO activity was found in the brain as a result of either heme loading (H-V-H) or ZnBG treatment (H-Zn-H) (Fig. 4C).
HO-1 protein levels.
After measuring HO-1 protein levels at 24 h after a second heme load, we found no significant difference in liver protein levels in the H-V-H group, compared with the V-V-V group (Fig. 5A). In the H-Zn-H group, treatment with ZnBG increased liver HO-1 protein to 1.6-fold. In the spleen, protein levels also did not significantly increase after the second heme load (H-V-H) compared with the V-V-V group (Fig. 5B), whereas after treatment with ZnBG (H-Zn-H), protein levels significantly increased to 1.2-fold. In the brain, protein levels did not significantly change after repeated heme loads (H-V-H) or ZnBG treatment (H-Zn-H) (Fig. 5C). When HO-2 protein levels in the same tissue samples were measured, there were no significant changes found in any tissue or any group.
Effects of heme and heme/ZnBG on HO-1 protein. HO-1 protein (mean ± SD) in the liver (A), spleen (B), and brain (C) of control (V-V-V), heme-loaded (H-V-H), and heme-loaded and ZnBG-treated (H-Zn-H, 15-μmol ZnBG/kg BW) mice was measured 24 h after a second heme load. Data were expressed as fold change from baseline (mean ± SD), n ≥ 5 mice for each treatment group. *p ≤ 0.05 compared with V-V-V levels; †p ≤ 0.05 compared with H-V-H levels.
HO-1 mRNA levels.
Because HO-1 protein levels were increased in the H-Zn-H group, we assessed HO-1 mRNA levels in liver and spleen samples from V-V-V, H-V-H, and H-Zn-H animals at 6 h after a second heme load. In the liver, HO-1 mRNA levels did not significantly increase after the second heme load (H-V-H) compared with the V-V-V group but did significantly increase to 2.3-fold after ZnBG treatment (H-Zn-H) (Fig. 6A). In the spleen, HO-1 mRNA levels significantly increased to 2.1-fold after repeated heme loads (H-V-H), with no further significant change after ZnBG treatment (H-Zn-H) (Fig. 6B). When HO-1 mRNA levels were assessed in the liver, spleen, and brain samples taken at 24 h after a second heme load, no significant effects were observed in any group (Table 1).
Effects of heme and heme/ZnBG on HO-1 mRNA, 6 h postsecond heme load. HO-1 mRNA (mean ± SD) in the liver (A) and spleen (B) of control (V-V-V), heme-loaded (H-V-H), and heme-loaded and ZnBG-treated (H-Zn-H, 15 μmol ZnBG/kg) mice was measured 6 h after a second heme load and normalized to 5 β-actin mRNA levels in the same tissues, n ≥ 4 mice for each treatment group. *p ≤ 0.05 compared with V-V-V levels, †p ≤ 0.05 compared with H-V-H levels.
DISCUSSION
First, to evaluate ZnBG's inhibitory efficacy on HO activity, we orally administered vehicle or a range of ZnBG doses to 1-wk-old mice. We observed that ZnBG is orally absorbed by neonatal mice and can rapidly inhibit liver HO activity in a dose-dependent and organ-specific manner within 3 h of oral administration, with an I50 of 4.0 μmol/kg BW.
Next, to evaluate the effects of ZnBG in heme-loaded newborn mice, we orally administered a higher dose of ZnBG in between two s.c. heme loads to 1-wk-old mice. A property necessary for ZnBG to be an effective antihyperbilirubinemia drug is its ability to reduce in vivo bilirubin production. We observed that peak bilirubin production in 1-wk-old mice receiving two heme loads and 15 μmol ZnBG/kg BW was 19% lower than peak production in heme-loaded mice not treated with ZnBG. Similarly, previous studies of adult mice treated with 30 μmol SnMP/kg BW at 3 h before a 30-μmol/kg BW heme load showed a 20% reduction of peak bilirubin production as estimated from total body CO excretion (17).
In addition to effectively reducing bilirubin production, 15 μmol ZnBG/kg BW completely eliminated heme-induced liver HO activity to baseline levels at 24 h after a second heme load. Unlike in the liver, heme loading did not significantly increase spleen HO activity in the newborn mice. This result corroborates the findings by Braggins et al. (20) and Maines (21) that spleen HO-1 is already maximally up-regulated in normal conditions, because it is a primary organ for red blood cell turnover. Under conditions of hemolysis, the liver can also act as another organ for processing excess heme, which results in the induction of both liver HO activity and transcription. When ZnBG was administered at the 15 μmol/kg BW dose between heme loads, we found that liver and spleen HO activity was reduced to baseline and to 30% below baseline levels, respectively. Inhibition to baseline or near-baseline levels of HO activity is desirable because under- or overmodulation of any key enzyme, such as HO, may be detrimental to a developing neonate (21).
Our observed inhibition of HO activity by ZnBG in the liver and spleen, but not the brain, is most likely due to the delivery route of oral administration because we have shown that in vitro, ZnBG inhibits HO activity to comparable degrees in tissue sonicates of liver, spleen, and brain (4). In addition, a recent in vivo study also showed that when ZnBG/kg BW was administered i.v. to adult mice, HO activity was inhibited in the liver, spleen, and brain within 1 h after administration (Ronald J. Wong, unpublished data). We have observed that orally administered ZnBG to adult mice results in the inhibition of HO activity in the liver, spleen, and intestine (3). In this study, we also found significant inhibition of liver and spleen HO activity after oral administration of ZnBG to 1-wk-old mice. When a drug is administered orally, it is absorbed directly by the digestive and hepatic portal system—“first pass effect”—and therefore is not available to circulate to other tissues (22), accounting for our observed lack of inhibition of brain HO activity.
At 6-h after administration of repeated heme loads (H-V-H), we found a 2.1-fold increase in spleen HO-1 mRNA. At this same time point, H-Zn-H treatment resulted in 2.3- and 2.2-fold increases in liver and spleen HO-1 mRNA, respectively, correlating with the increased HO-1 protein levels observed in these tissues 24 h later. This up-regulation of HO-1 mRNA appears to be transient, because by 24-h after administration of H-V-H or H-Zn-H, mRNA returned to baseline levels. In adult mice, we found a similar transient increase in HO-1 transcription 6-h after ZnBG administration, which returned to baseline by 24 h (3).
Even though HO-1 protein is induced 24 h after ZnBG treatment, we found that by 2 wk after treatment, liver and spleen HO-1 protein (1.0 ± 0.1 and 1.2 ± 0.2-fold change, respectively) and HO activity (101 ± 4% and 100 ± 2%, respectively) levels have already returned to baseline levels. At 1 wk after treatment, liver HO-1 protein has already returned to baseline levels (1.1 ± 0.1-fold), whereas spleen HO-1 protein (1.6 ± 0.1-fold) is still increased. However, this induction was counteracted by a persistent inhibition of spleen HO activity to 77 ± 5% of baseline. Taken together, the induction of HO-1 by ZnBG most likely has no long-term effects.
Our previous work in adult mice also showed that at 24 h after two successive heme loads, liver HO-1 transcription and protein increased 7- and 2.3-fold over baseline, respectively (17). That heme loads apparently have a more dramatic and sustained effect on HO-1 transcription in adult (17) than in newborn mice may occur in part because HO is developmentally regulated in the liver, being expressed at a higher level in the neonate than the adult. This observation has been shown in the rat liver (23) and the mouse cortex (24). There may also be suppression of neonatal HO-1 inducibility in response to stresses such as heme loading. Previous reports by Kassovska-Bratinova et al. (25), Di Giulio et al. (26), and Lavrovsky et al. (27) have demonstrated reduced HO-1 inducibility in the neonatal rat because of increased levels of the known HO-1 repressor Bach1 in infancy (25) or increased levels of the HO-1 inducer NF-κB in adulthood (27). These mechanisms and their potential relevance to hemolysis merit further investigation.
It is possible that the induction of liver and spleen HO-1 in the H-Zn-H group occurs in response to not simply the exogenous heme from heme loads but also the native heme that remains unmetabolized after the inhibition of HO by ZnBG. Kappas et al. (28) reported that after inhibition of HO by tin protoporphyrin, the unmetabolized heme is eventually excreted into the bile, and we found that this excretion is proportional to the degree of HO inhibition (29). It is likely that after inhibition of HO by ZnBG, unmetabolized heme (including any excess from heme loading) is eventually excreted through the same route.
Our result (30) and the results of Bonkovsky and co-workers (31,32) have shown that various Mps, including SnMP, up-regulate HO-1 gene transcription by sequestering or causing downstream degradation of Bach1. However, we believe that ZnBG has much less interaction with Bach1 than CrMP or SnMP (S. Schulz, unpublished data), which suggests that ZnBG up-regulates HO-1 through an as-yet-unknown mechanism.
Although ZnBG is similar in photoreactivity to SnMP, ZnBG's high potency could make it clinically effective at much lower doses (11,15). This study showed the effectiveness of oral doses as low as 3.75 μmol ZnBG/kg BW in suppressing HO activity and also showed the effectiveness of 15 μmol ZnBG/kg BW in our hemolytic newborn mouse model. In addition, unlike SnMP, ZnBG has minimal effects on NOS and sGC (14). To further examine the clinical utility of ZnBG, ongoing work includes light exposure studies comparing the relative photosensitivities of newborn mice under treatment with SnMP, CrMP, and ZnBG.
We have demonstrated that ZnBG is orally absorbable, inhibits both basal and heme-induced HO activity in the liver and spleen, and also reduces in vivo bilirubin production. Our data strongly suggest that even if ZnBG does up-regulate HO-1 transcription and translation, the effect is a transient one. ZnBG is therefore an attractive compound for oral use in the treatment of neonatal jaundice caused by hemolytic disease, comparable or even preferable to SnMP.
Abbreviations
- BW:
-
body weight
- CrMP:
-
chromium mesoporphyrin
- FW:
-
fresh weight
- H:
-
subcutaneous heme load
- HO:
-
heme oxygenase
- I50:
-
dose needed to inhibit HO activity by 50%
- MHA:
-
methemalbumin
- Mp:
-
metalloporphyrin
- OG:
-
oral gavage
- sGC:
-
soluble guanylate cyclase
- SnMP:
-
tin mesoporphyrin
- V:
-
vehicle (saline)
- VeCO:
-
total body CO excretion rate
- ZnBG:
-
zinc deuteroporphyrin bis glycol
References
Tenhunen R, Marver HS, Schmid R 1968 The enzymatic conversion of heme to bilirubin by microsomal heme oxygenase. Proc Natl Acad Sci U S A 61: 748–755
Stevenson DK, Wong RJ, Hintz SR, Vreman HJ 2011 Drugs for hyperbilirubinemia. In: Yaffe SJ, Aranda JV (eds) Neonatal and Pediatric Pharmacology. Therapeutic Principles in Practice. Lippincott Williams & Wilkins: Philadelphia, PA 221–232
Morioka I, Wong RJ, Abate A, Vreman HJ, Contag CH, Stevenson DK 2006 Systemic effects of orally-administered zinc and tin (IV) metalloporphyrins on heme oxygenase expression in mice. Pediatr Res 59: 667–672
Vreman HJ, Ekstrand BC, Stevenson DK 1993 Selection of metalloporphyrin heme oxygenase inhibitors based on potency and photoreactivity. Pediatr Res 33: 195–200
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia 2004 Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114: 297–316
Morris BH, Oh W, Tyson JE, Stevenson DK, Phelps DL, O'Shea TM, McDavid GE, Perritt RL, Van Meurs KP, Vohr BR, Grisby C, Yao Q, Pedroza C, Das A, Poole WK, Carlo WA, Duara S, Laptook AR, Salhab WA, Shankaran S, Poindexter BB, Fanaroff AA, Walsh MC, Rasmussen MR, Stoll BJ, Cotten CM, Donovan EF, Ehrenkranz RA, Guillet R, Higgins RD 2008 Aggressive vs. conservative phototherapy for infants with extremely low birth weight. N Engl J Med 359: 1885–1896
Vreman HJ, Cipkala DA, Stevenson DK 1996 Characterization of porphyrin heme oxygenase inhibitors. Can J Physiol Pharmacol 74: 278–285
Maines MD 1981 Zinc protoporphyrin is a selective inhibitor of heme oxygenase activity in the neonatal rat. Biochim Biophys Acta 673: 339–350
Drummond GS, Kappas A 1981 Prevention of neonatal hyperbilirubinemia by tin protoporphyrin IX, a potent competitive inhibitor of heme oxidation. Proc Natl Acad Sci USA 78: 6466–6470
Stevenson DK, Rodgers PA, Vreman HJ 1989 The use of metalloporphyrins for the chemoprevention of neonatal jaundice. Am J Dis Child 143: 353–356
Vreman HJ, Wong RJ, Stevenson DK 2001 Alternative metalloporphyrins for the treatment of neonatal jaundice. J Perinatol 21: S108–S113
Wong RJ, Vreman HJ, Schulz S, Kalish FS, Pierce NW, Stevenson DK 2011 In vitro inhibition of heme oxygenase isoenzymes by metalloporphyrins. J Perinatol 31: S35–S41
Wong RJ, Bhutani VK, Vreman HJ, Stevenson DK 2007 Tin mesoporphyrin for the prevention of severe neonatal hyperbilirubinemia. Neoreviews 8: e77–e84
Appleton SD, Chretien ML, McLaughlin BE, Vreman HJ, Stevenson DK, Brien JF, Nakatsu K, Maurice DH, Marks GS 1999 Selective inhibition of heme oxygenase, without inhibition of nitric oxide synthase or soluble guanylyl cyclase, by metalloporphyrins at low concentrations. Drug Metab Dispos 27: 1214–1219
Vreman HJ, Lee OK, Stevenson DK 1991 In vitro and in vivo characteristics of a heme oxygenase inhibitor: ZnBG. Am J Med Sci 302: 335–341
Stevenson DK, Wong RJ 2010 Metalloporphyrins in the management of neonatal hyperbilirubinemia. Semin Fetal Neonatal Med 15: 164–168
DeSandre GH, Wong RJ, Morioka I, Contag CH, Stevenson DK 2006 The effectiveness of oral tin mesoporphyrin prophylaxis in reducing bilirubin production after an oral heme load in a transgenic mouse model. Biol Neonate 89: 139–146
Vreman HJ, Stevenson DK 1988 Heme oxygenase activity as measured by carbon monoxide production. Anal Biochem 168: 31–38
Vreman HJ, Stevenson DK 2001 Detection of heme oxygenase activity by measurement of CO. In: Maines MD, Costa LG, Reed DJ, Sassa S, Sipes IG (eds) Current Protocols in Toxicology. Unit 9.2. John Wiley & Sons, Inc: New York, NY, 9.2.1–9.2.10.
Braggins PE, Trakshel GM, Kutty RK, Maines MD 1986 Characterization of two heme oxygenase isoforms in rat spleen: comparison with the hematin-induced and constitutive isoforms of the liver. Biochem Biophys Res Commun 141: 528–533
Maines MD 2005 The heme oxygenase system: update. Antioxid Redox Signal 7: 1761–1766
Gibaldi M, Boyes RN, Feldman S 1971 Influence of first-pass effect on availability of drugs on oral administration. J Pharm Sci 60: 1338–1340
Lin JH, Villalon P, Nelson JC, Abraham NG 1989 Expression of rat liver heme oxygenase gene during development. Arch Biochem Biophys 270: 623–629
Zhao H, Wong RJ, Nguyen X, Kalish F, Mizobuchi M, Vreman HJ, Stevenson DK, Contag CH 2006 Expression and regulation of heme oxygenase isozymes in the developing mouse cortex. Pediatr Res 60: 518–523
Kassovska-Bratinova S, Yang G, Igarashi K, Dennery PA 2009 Bach1 modulates heme oxygenase-1 expression in the neonatal mouse lung. Pediatr Res 65: 145–149
Di Giulio C, Verratti V, Artese L, Petruccelli G, Walski M, Pokorski M 2009 Aging and expression of heme oxygenase-1 and endothelin-1 in the rat carotid body after chronic hypoxia. J Physiol Pharmacol 60: 41–44
Lavrovsky Y, Song CS, Chatterjee B, Roy AK 2000 Age-dependent increase of heme oxygenase-1 gene expression in the liver mediated by NFkappaB. Mech Ageing Dev 114: 49–60
Kappas A, Simionatto CS, Drummond GS, Sassa S, Anderson KE 1985 The liver excretes large amounts of heme into bile when heme oxygenase is inhibited competitively by Sn-protoporphyrin. Proc Natl Acad Sci U S A 82: 896–900
Hintz SR, Kwong LK, Vreman HJ, Stevenson DK 1987 Recovery of exogenous heme as carbon monoxide and biliary heme in adult rats after tin protoporphyrin treatment. J Pediatr Gastroenterol Nutr 6: 302–306
Abate A, Zhao H, Wong RJ, Stevenson DK 2007 The role of Bach1 in the induction of heme oxygenase by tin mesoporphyrin. Biochem Biophys Res Commun 354: 757–763
Hou W, Shan Y, Zheng J, Lambrecht RW, Donohue SE, Bonkovsky HL 2008 Zinc mesoporphyrin induces rapid and marked degradation of the transcription factor Bach1 and up-regulates HO-1. Biochim Biophys Acta 1779: 195–203
Shan Y, Lambrecht RW, Donohue SE, Bonkovsky HL 2006 Role of Bach1 and Nrf2 in up-regulation of the heme oxygenase-1 gene by cobalt protoporphyrin. FASEB J 20: 2651–2653
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by a Stanford Undergraduate Advising and Research Major Grant, as well as National Institutes of Health Grants HL68703-07 S1 (ARRA) and HL68703-07.
The authors report no conflicts of interest.
Rights and permissions
About this article
Cite this article
He, C., Campbell, C., Zhao, H. et al. Effects of Zinc Deuteroporphyrin Bis Glycol on Newborn Mice After Heme Loading. Pediatr Res 70, 467–472 (2011). https://doi.org/10.1203/PDR.0b013e31822e1675
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31822e1675
This article is cited by
-
Heme oxygenase-1 deficiency promotes severity of sepsis in a non-surgical preterm mouse model
Pediatric Research (2018)
-
Inhibition of heme oxygenase activity using a microparticle formulation of zinc protoporphyrin in an acute hemolytic newborn mouse model
Pediatric Research (2016)
-
Effect of light exposure on metalloporphyrin-treated newborn mice
Pediatric Research (2012)