Abstract
Prolonged unconjugated hyperbilirubinemia in infants associated with breast milk feeding is a common pediatric problem known as breast milk jaundice (BMJ). A polymorphic mutation (G71R) of bilirubin UDP-glucuronosyltransferase (UGT1A1) is a known cause of BMJ on the infantile side, but the responsible components of breast milk are not currently known. We analyzed the inhibitory effect of 5β-pregnane-3α,20β-diol (pregnanediol) on transcriptional activity and enzyme activity of UGT1A1. To this end, we constructed two types of expression vectors. One type comprised vectors including the upstream enhancer-promoter sequence of UGT1A1 for WT and variant type (-3279T>G with A(TA)7TAA), used in studying transcriptional regulation. The other type comprised vectors including cDNA of UGT1A1 for WT and the G71R variant, used in studying enzyme activity. In an in vitro expression study, pregnanediol did not affect the transcriptional activity of UGT1A1 enhancer-promoter complex of WT and variant type, even with coexistence of transcriptional factors such as constitutive androstane receptor or pregnane X receptor. In contrast, in the presence of 100 μM pregnanediol, bilirubin glucuronidation of G71R-UGT1A1 was reduced to 51% of WT. We suggest that pregnanediol is a cause of breast milk jaundice in carriers of G71R.
Similar content being viewed by others
Main
Breast milk jaundice (BMJ) is characterized by prolonged unconjugated hyperbilirubinemia in healthy infants connected with ingestion of breast milk (1). Infants with BMJ always have an elevated serum bilirubin level, above 171 μM (10 mg/dL); it occasionally exceeds 342 μM (20 mg/dL), and at such levels infants are at risk of bilirubin encephalopathy (kernicterus) (2).
BMJ was first described by Newman and Gross, who found a causal relation between human milk feeding and jaundice, based on rapid clearance of jaundice when the infants were taken off breast milk (3). Arias et al. (4) first reported the inhibiting effect of breast milk on human liver slices and homogenates using bilirubin and o-aminophenol as substrates for conjugation. In their pioneering study, the inhibitory substance in milk was identified as 5β-pregnane-3α,20β-diol (pregnanediol). However, a further study by Adlard et al. (5) found that bilirubin conjugation by slices taken from two human livers was not inhibited by pregnanediol. Moreover, other research groups have reported that BMJ may be caused by other breast milk components such as free fatty acids (FFA) or β-glucuronidase (6,7). The responsible substance in breast milk has not yet been identified with certainty (8–10).
The elimination pathway of bilirubin in humans is catalyzed exclusively by bilirubin UDP-glucuronosyltransferase (UGT1A1) (11). A defect in UGT1A1 causes hereditary unconjugated hyperbilirubinemias, specifically Crigler-Najjar syndrome type I (CN-I; MIM #218800), Crigler-Najjar syndrome type II (CN-II; MIM #606785), and Gilbert syndrome (GS; MIM #43500) (12–16). Polymorphic mutations of UGT1A1, namely G71R in the coding region and A(TA)7TAA with -3279T>G in the regulatory region, are the most common causes of Gilbert syndrome, and the latter linked mutations are the sole cause of Gilbert syndrome in Caucasians and Africans (17). Maruo et al. (18,19) have shown that G71R (but not A(TA)7TAA with -3279T>G) is an infantile cause of prolonged unconjugated hyperbilirubinemia in East Asia and is also a risk factor for BMJ.
Previous studies seeking substances in breast milk that lead to BMJ were based on histochemical and enzymatic assays using samples prepared from tissues. In the present study, we analyzed the effect of pregnanediol on both wild and variant UGT1A1s based on our gene analyses of infants suffering from neonatal and BMJ. We examined the effect of pregnanediol on the transcriptional activities of UGT1A1 of both WT (-3279T with A(TA)6TAA) and variant-type (-3279G with A(TA)7TAA) enhancer-promoter complexes. The variant-type enhancer-promoter is the cause of Gilbert syndrome in Caucasian and African populations (17). We also examined the effect of pregnanediol on transcriptional activities of UGT1A1 in the presence of constitutive androstane receptor (CAR) and pregnane X receptor (PXR), which have both been proposed as key transcriptional factors of bilirubin clearance in the human liver (20–24). We first examined the effect of pregnanediol on enzyme activities of WT UGT1A1 and G71R-UGT1A1 in an in vitro study.
METHODS
Effect of pregnanediol on transcriptional activity of UGT1A1.
To construct an expression vector, two types of enhancer-promoter complex, including upstream of UGT1A1 (c.-1 to c.-4076); WT enhancer-promoter complex and variant-type enhancer-promoter complex (-3279 T>G with A(TA)7TAA) (variant-type enhance-promoter) of DNA fragments, were amplified from genomic DNA. The distal region (c.-4076 to c.-1945) and the proximal region (c.-2483 to c.247) were amplified separately by PCR using the respective primers with the restriction sites: 5′-GAGAGCTCCCTCAGCCCCTAGAGCACCATC-3′/5′-CTCTCGAGGCGCCTTTGCTCCTGCCAGAGG-3′ (the SacI site is underlined) and 5′-GAGAGCTCGAAGGGATTAGTTTAGGACAACCCTCCTTC-3′/5′-GCAGAGCTTCCAAGCTTTTTGAGGCTG-3′ (the XhoI site is underlined).
Each PCR product (proximal; c.2323 to c.-1; distal:c.-4076 to c.-1945) was inserted into the pCR-XL-TOPO vector using a TOPO XL PCR cloning kit. We constructed PGV-B2 expression vectors (TOYO B-Net Co., Ltd, Tokyo, Japan) having WT enhancer-promoter and variant type enhancer-promoter with continuous 4-kbp regulatory region (c.-4076 to c.-1) by restriction (SacI and XhoI) and ligation using a Ligation-Convenience Kit (NIPPON GENE Co., Ltd, Tokyo, Japan) as described previously (25).
CAR-cDNA was amplified from a human liver cDNA library (TaKaRa BIO, Inc.) by PCR using the following primers with the restriction sites (EcoR I and EcoR V): 5′-GATCGAATTCGTCATGGCCAGTGGGAAGATGAG-3′ (the EcoR I site is underlined) and 5′-GATCGATATCTCAGCTGCAGATCTCCTGGAGCCAG-3′ (the EcoR V site is underlined) (26). The PCR product ligated into the pCR3.1 vector (Invitrogen Corporation). PXR-cDNA was amplified from a human liver cDNA library (TaKaRa BIO, Inc.) by PCR using the following primers: 5′-AGCCATGAATTCCTGGAGGTGAGACCCAAA-3′ and 5′-AGCCATGAATTCTCAGCTACCTGTGATGCC-3′ (the EcoR I site is underlined) (27). PXR-cDNA was cut out by EcoR I. The PCR product was ligated into the pcDNA 3.3-TOPO vector (Invitrogen Corporation).
The in vitro expression study by assay for transcriptional activity of WT enhancer-promoter and variant-type enhancer-promoter (c.-4076 to c.-1) proceeded as we have reported elsewhere (26), with minor modification. At 25 h before transfection, 7 × 104 HepG2 cells (Riken Cell Bank, Japan) cultured in minimal essential medium (MEM; Invitrogen Corporation) with 10% fetal bovine serum (Invitrogen Corporation) were seeded onto 24-well culture plates.
For transfection, 250 μL of MEM, 3.0 μL of GenePORTER transfection reagent (GeneLantis, San Diego, CA), and plasmid vectors were poured onto the cells in each well. The composition of the plasmid vectors for transfection was as follows: luciferase reporter plasmid PGV-B2 with the transcriptional regulatory region (400 ng), the CAR-pCR3.1 expression plasmid or PXR-pCR3.1 expression plasmid (200 ng), and the Renilla luciferase expression plasmid pRL-SV40 (6 ng; TOYO B-Net Co., Ltd) for normalization. After 3 h, 250 μL of MEM containing 20% fetal bovine serum and 0 to 100 mM pregnanediol was added to each well. After 25 h, the transfected cells in each well were lysed, and the dual luciferase activities were immediately measured with a PicaGene Dual SeaPansy Luminescence Kit (TOYO B-Net Co.).
Effect of pregnanediol on bilirubin glucuronidation activity of UGT1A1.
The cDNA of human liver UGT1A1 was amplified from a human cDNA library (TaKaRa BIO, Inc.) by PCR using the primer pair 5′-CATGGCTGTGGAGTCCCAGGGC-3′ and 5′-GAATCCCGCACTCCCAAACAGG-3′ and was inserted into a pCR3.1 expression vector using a eukaryotic bidirectional TA cloning kit (Invitrogen, San Diego, CA). The constructed WT cDNA was excised from the pCR3.1 vector by two restriction enzymes (HindIII and XbaI) and ligated into a pkF18 vector (TaKaRa BIO, Inc.) for mutagenesis. To introduce the mutations into the UGT1A1 cDNA, we used the following primers (the mutation point is underlined): 5′-CATCAGAGACAGAGCATTTTA-3′ for the G to A transversion at nucleotide 211 (c.211G>A) for G71R using the site-directed mutagenesis method and a Mutan Km Kit (TAKARA, Kyoto, Japan). The converted cDNA was cut out and religated into the pCR3.1 vector. We verified the cDNA by sequencing (18).
At 24 h before transfection, 6 × 105 COS-7 cells suspended in DMEM with 10% fetal bovine serum were seeded onto 100-mm-diameter culture plates. For transfection, we poured onto the cells 5 mL of DMEM, containing 50 μL GenePORTER Transfection Reagent (GeneLantis) and 10.0 μg DNA. Four hours later, 5 mL of DMEM containing 20% fetal bovine serum was added to each plate. Two models were generated, WT UGT1A1 and G71R-UGT1A1, and nontransfected cells were used as controls. After 48 h, the transfected cells were harvested and stored at −80°C before use. Protein content was measured with a Bicinchoninic Acid Protein Assay Kit (Pierce Chemical, Rockford, IL).
The methods used in the assay for glucuronidation activity toward bilirubin by UGT1A1 have been reported previously (28). The glucuronidation process of the substrate was assayed with [14C] UDP-glucuronic acid (PerkinElmer Life and Analytical Sciences, Boston, MA). The incubation mixture contained 100 to 150 μg of cell homogenate, 0 to 400 μM unconjugated bilirubin (Wako Pure Chemical Industries, Ltd, Osaka, Japan), 500 μM UDP-glucuronic acid (Sigma Chemical Co.-Aldrich, St. Louis, MO), 9.25 kBq [14C] UDP-glucuronic acid (5.97 μM), DMSO (1%), 5 mM MgCl2, 50 mM Tris-HCl buffer (pH 7.5), and 5 mM saccharolactone in a final volume of 100 μL. Incubation took place for 30 min at 37°C. The resultant bilirubin-glucuronide was isolated by thin layer chromatography (TLC) on a TLC plastic sheet 5748 (Merck, Darmstadt, Germany) and was scanned on an Instant Imager (Packard, Meriden, CT). At a bilirubin concentration of 400 μM, pregnanediol (0–100 μM) was added to the reaction mixture to examine its inhibitory effect on bilirubin glucuronidation.
The amounts of enzyme expressed were determined by Western blotting analysis, using anti-UGT1A antibody (diluted 1:10,000; BD Gentest, Woburn, MA) to adjust the enzyme activity. The cell homogenates underwent SDS-PAGE. The protein was transferred to a polyvinylidene fluoride membrane. The membrane was incubated for 4 h in blocking solution, 1 h in a solution of rabbit anti-human UGT1A (diluted 1:10,000; BD Gentest), and 1 h in a solution of anti-rabbit antibody (1:20,000). The detection solution was then added, and the membrane was exposed to film for 5 min, after which the protein was visualized (ECL: enhanced chemiluminescence Plus Western blotting detection system; Amersham Bioscience, United Kingdom). The relative amounts of UGT1A1 expressed at the protein bands were measured with a LAS-4000 (Fujifilm Lifescience, Tokyo, Japan).
Data analysis.
We calculated kinetic parameters by performing nonlinear regression on the Michaelis-Menten equation using the Prism 3.0 software (Graph Pad Software, San Diego, CA). Changes in transcriptional activity and enzyme activity were analyzed by regression analysis using JMP software (SAS Institute, Inc., NC).
RESULTS
Effect of pregnanediol on transcriptional activity of UGT1A1.
Transcriptional activity of the regulatory region of UGT1A1 with variant-type enhancer-promoter decreased to 42% of WT enhancer-promoter (p < 0.05). The transcriptional activity of WT and variant type was not reduced in the presence of pregnanediol (up to100 μM); Figure 1.
Effect of pregnanediol on transcriptional activities of the regulatory region (c.4076 to c.-1) of UGT1A1; WT enhancer-promoter (▪) and variant-type enhancer-promoter [-3279T>G with A(TA)7TAA] (□). All activities in the figure are expressed relative to the mean transcriptional activity of WT in the absence of pregnanediol, taken as 1.00.
As shown in Figure 2, the transcriptional activities of the regulatory region with WT and variant type were increased about 4-fold in the presence of CAR (p < 0.001). Transcriptional activities of both of the enhancer-promoter complexes were not inhibited by pregnanediol, even in the presence of CAR.
Effect of pregnanediol on transcriptional activities of the regulatory region (c.4076 to c.-1) of WT and variant-type UGT1A1 in the presence of CAR. Bars are as follows: WT (▪), variant type (□), WT with CAR ( ), and variant type with CAR (
), and variant type with CAR ( ). All activities in the figure are expressed relative to the mean transcriptional activity of WT in the absence of pregnanediol, taken as 1.00.
). All activities in the figure are expressed relative to the mean transcriptional activity of WT in the absence of pregnanediol, taken as 1.00.
In the presence of PXR, the transcriptional activities of the regulatory region with WT and variant type increased by a factor of about 1.5 (p < 0.001); Figure 3. As with CAR, pregnanediol did not inhibit the transcriptional activities of either of the enhancer-promoter complexes in the presence of PXR.
Effect of pregnanediol on transcriptional activities of the regulatory region (c.4076 to c.-1) of WT and variant-type UGT1A1 in the presence of PXR. Bars are as follows: WT (▪), variant type (□), WT with PXR ( ), variant type with PXR (
), variant type with PXR ( ). All activities in the figure are expressed relative to the mean transcriptional activity of WT in the absence of pregnanediol, taken as 1.00.
). All activities in the figure are expressed relative to the mean transcriptional activity of WT in the absence of pregnanediol, taken as 1.00.
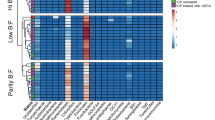
Effect of pregnanediol on bilirubin glucuronidation of UGT1A1.
The relative expression levels of each UGT1A1 protein were determined by Western blotting with a polyclonal anti-human UGT1A antibody. Simultaneous expression of wild UGT1A1 in three independent experiments resulted in UGT1A1 protein levels in the culture cells between 0.9 and 1.1 times the average amount. The amount of G71R UGT1A1 was always 0.85–0.9 times that of wild.
Table 1 shows the kinetic parameters of WT UGT1A1 and G71R-UGT1A1. The Vmax value of WT UGT1A1 was 7.80 pmol/min/mg protein. For G71R-UGT1A1, Vmax was 83.3% of WT. The enzyme activity for bilirubin glucuronidation of WT UGT1A1 in the absence of pregnanediol was 9.34 ± 1.07 pmol/min/mg protein and that of G71R-UGT1A1 was 7.57 ± 0.90 pmol/min/mg protein (81.0% of WT); see Figure 4. Unexpectedly, the enzyme activity of WT increased slightly on adding pregnanediol, in all concentrations (Fig. 4). In contrast, the enzyme activity of G71R-UGT1A1 decreased slightly in the presence of pregnanediol in all concentrations. The ratio of the activity of G71R-UGT1A1 to WT decreased from 81% to 51% on adding 100 μM pregnanediol (Fig. 5). This ratio decreased significantly in the presence of pregnanediol according to our regression analysis (p = 0.02).
DISCUSSION
BMJ is characterized by prolonged unconjugated hyperbilirubinemia associated with breast milk feeding in healthy infants more than 3–4 wk after birth. BMJ has been variously ascribed to breast milk components such as 5β-pregnane-3α,20β-diol (pregnanediol), other steroids (cortisol and estriol), nonesterified fatty acids, and β-glucuronidase, but the relevant components of breast milk have not yet been identified.
We have investigated here the inhibition of transcriptional activity of UGT1A1 by pregnanediol using an in vitro expression system. The transcriptional activities of WT and variant-type (-3279T>G with A(TA)7TAA) enhancer-promoter were both unaffected by pregnanediol (Fig. 1). The gtPBREM (phenobarbital-responsive enhancer module) in the regulatory region of UGT1A1 is an important enhancer module of UGT1A1, and functions in the presence of nuclear receptors (29,30) such as CAR and PXR, which have been proposed as key transcriptional factors of bilirubin clearance in the human liver and intestine (31). The transcriptional activities of WT and variant-type enhancer-promoters both increased in the presence of these receptors (Figs. 2,3). The transcriptional activities of WT and variant-type enhancer-promoters were not affected by pregnanediol, even in the presence of these receptors. UGT1A1 activity in early infancy is less than 1% of adult activity, which is reached by 3 mo of age (32). This change is believed to involve the induction of the UGT1A1 enzyme by increasing transcriptional activity of the UGT1A1 gene. Our study suggests that pregnanediol does not inhibit the neonatal induction of UGT1A1.
Variant-type enhancer-promoter is the prevalent cause of Gilbert syndrome. In our previous study of BMJ in the Japanese population, the variation was not a risk factor for BMJ or neonatal hyperbilirubinemia (18,19). Bancroft et al. (33) also reported that the variant-type enhancer-promoter did not significantly affect neonatal hyperbilirubinemia. The variant-type enhancer-promoter might therefore be less effective in giving rise to BMJ than G71R. In the European population, however, this variant has been reported to be a risk factor for BMJ (34). This report is inconsistent with our observation that pregnanediol did not inhibit transcriptional activity of WT or of variant-type enhancer-promoter. It is possible that further unknown mutations, specific to Caucasians, link to the variant, and that ingredients of breast milk other than pregnanediol are involved in BMJ caused by the variation.
The recent report by Fujiwara et al. (35) with human UGT1A1 gene complex, using humanized mice, revealed that bilirubin clearance during the neonatal period is associated not with hepatic UGT1A1 but with intestinal UGT1A1. Furthermore, A(TA)7TAA causes a decline in expression of hepatic UGT1A1, but the induction of UGT1A1 in the small intestine in the neonatal period is independent of the polymorphism in the mice. These findings support and explain the observation that A(TA)7TAA is not a risk factor of BMJ (18,19). Although the regulatory sequence responsible for intestinal induction of UGT1A1 has not yet been fully clarified, PXR activator, pregnenolone-16α-carbonitrile has reported to induce UGT1A1 in mouse small intestine (31). If PXR is responsible for inducing intestinal UGT1A1 in neonatal period, our results indicate that pregnanediol does not inhibit the induction.
We found that enzyme activity of WT UGT1A1 was not inhibited in the presence of pregnanediol but enzyme activity of G71R-UGT1A1 decreased (Fig. 4). The relative enzyme activity (G71R/WT) decreased to 51% (p = 0.02). G71R is a very common mutation of UGT1A1 in Gilbert syndrome in East Asians (14,18) and has been reported as a cause of BMJ on the infantile side by Maruo et al. (19). Pregnanediol in breast milk may directly inhibit UGT1A1 expressed in the human intestine in carriers of G71R (35). The present results, demonstrating the inhibitory effect of pregnanediol on G71R-UGT1A1, confirm previous results and clarify the underlying mechanism of BMJ (17).
In the neonatal period, UGT1A1 activity is very low (32). Furthermore, pregnanediol inhibits glucuronidation activity of G71R-UGT1A1, which has lower activity than WT UGT1A1. These observations may explain why severe unconjugated hyperbilirubinemia, with a serum bilirubin concentration above 20 mg/dL (340 μM), occasionally occurs in carriers of G71R. Beyond 4 mo of age, UGT1A1 activity runs at adult levels, as reported by Onishi et al. (32), and prolonged unconjugated hyperbilirubinemia in infants with G71R variant disappears even if breast milk feeding continues. It is possible that BMJ is caused by the combined effect of three factors: 1) a low amount of UGT1A1-protein in the neonatal period; 2) decreased enzyme activity by G71R; and 3) inhibition of G71R-UGT1A1 by pregnanediol. The inhibitory effect of pregnanediol is also consistent with our finding that G71R is a risk factor for neonatal hyperbilirubinemia (18). When infants with G71R ingest pregnanediol in breast milk in the early neonatal period, neonatal hyperbilirubinemia, and BMJ, may manifest or be intensified.
Breast milk contains a number of steroids, such as progesterone, cortisol, estrone, estradiol and estriol, and pregnanediol (36–38). Although these steroids are found in breast milk in much lower concentrations than pregnanediol (15 to 45 μg/100 mL) (39), they may still inhibit the activity of UGT1A1. For a deeper understanding of BMJ, especially in Caucasians, it would be helpful to examine whether these steroids contribute to the development of BMJ, in addition to pregnanediol.
This study has shown that a combination of G71R and pregnanediol in breast milk is a cause of BMJ in an East Asian population. Further research into the components of breast milk is necessary to settle the exact mechanism of BMJ.
Abbreviations
- BMJ:
-
breast milk jaundice
- CAR:
-
constitutive androstane receptor
- MEM:
-
minimal essential medium
- PXR:
-
pregnane X receptor
- UGT1A1:
-
bilirubin UDP-glucuronosyltransferase
References
Newman AJ, Gross S 1963 Hyperbilirubinemia in breast-fed infants. Pediatrics 32: 995–1001
Maisels MJ, Newman TB 1995 Kernicterus in otherwise healthy, breast-fed term newborns. Pediatrics 96: 730–733
Arias IM, Gartner LM 1964 Production of unconjugated hyperbilirubinemia in full-term new-born infants following administration of pregnane-3α,20β-diol. Nature 203: 1292–1293
Arias IM, Gartner LM, Seifter S, Furman M 1964 Prolonged neonatal unconjugated hyperbilirubinemia associated with breast feeding and a steroid, pregnane-3α,20β-diol, in maternal milk that inhibits glucuronide formation in vitro. J Clin Invest 43: 2037–2047
Adlard BP, Lathe GH 1970 Breast milk jaundice: Effect of 3α,20β-pregnanediol on bilirubin conjugation by human liver. Arch Dis Child 45: 186–189
Bevan BR, Holton JB 1972 Inhibition of bilirubin conjugation in rat liver slices by free fatty acids, with relevance to the problem of breast milk jaundice. Clin Chim Acta 41: 101–107
Hargreaves T 1973 Effect of fatty acids on bilirubin conjugation. Arch Dis Child 48: 446–450
Ramos A, Silverberg M, Stern M 1966 Pregnanediols and neonatal hyperbilirubinemia. Am J Dis Child 111: 353–356
Constantopoulos A, Messaritakis J, Matsaniotis N 1980 Breast milk jaundice: the role of lipoprotein lipase and the free fatty acids. Eur J Pediatr 134: 35–38
Gaffney PT, Buttenshaw RL, Ward M, Diplock RD 1986 Breast milk β-glucuronidase and neonatal jaundice. Lancet 1: 1161–1162
Bosma PJ, Seppen J, Goldhoorn B, Bakker C, Oude Elferink RP, Chowdhury JR, Chowdhury NR, Jansen PL 1994 Bilirubin UDP-glucuronosyltransferase 1 is the only relevant bilirubin glucuronidating isoform in man. J Biol Chem 269: 17960–17964
Sato H, Adachi Y, Koiwai O 1996 The genetic basis of Gilbert's syndrome. Lancet 347: 557–558
Aono S, Yamada Y, Keino H, Hanada N, Nakagawa T, Sasaoka Y, Yazawa T, Sato H, Koiwai O 1993 Identification of defect in the genes for bilirubin UDP-glucuronosyltransferase in a patient with Crigler-Najjar syndrome type II. Biochem Biophys Res Commun 197: 1239–1244
Maruo Y, Wada S, Yamamoto K, Sato H, Yamano T, Shimada M 1999 A case of anorexia nervosa with hyperbilirubinemia in a patient homozygous for a mutation in the bilirubin UDP-glucuronosyltransferase gene. Eur J Pediatr 158: 547–549
Monaghan G, Ryan M, Seddon R, Hume R, Burchell B 1996 Genetic variation in bilirubin UDP-glucuronosyltransferase gene promoter and Gilbert syndrome. Lancet 347: 578–581
Kadakol A, Ghosh SS, Sappal BS, Sharma G, Chowdhury JR, Chowdhury NR 2000 Genetic lesions of bilirubin uridine-disphosphoglucuronate glucuronosyltransferase (UGT1A1) causing Crigler-Najjar and Gilbert syndromes: correlation of genotype to phenotype. Hum Mutat 16: 297–306
Maruo Y, Nishizawa K, Sato H, Doida Y, Shimada M 1999 Association of neonatal hyperbilirubinemia with bilirubin UDP-glucuronosyltransferase polymorphism. Pediatrics 103: 1224–1227
Maruo Y, Nishizawa K, Sato H, Takahashi H, Shimada M 2000 Prolonged unconjugated hyperbilirubinemia associated with breast milk and mutations of the bilirubin uridine diphosphate-glucuronosyltransferase gene. Pediatrics 106: E59
Maruo Y, D'Addario C, Mori A, Iwai M, Takahashi H, Sato H, Takeuchi Y 2004 Two linked polymorphic mutations (A(TA)7TAA and T-3279G) of UGT1A1 as the principal cause of Gilbert syndrome. Hum Genet 115: 525–526
Sugatani J, Yamakawa K, Yoshinari K, Machida T, Takagi H, Mori M, Kakizaki S, Sueyoshi T, Negishi M, Miwa M 2002 Identification of a defect in the UGT1A1 gene promoter and its association with hyperbilirubinemia. Biochem Biophys Res Commun 292: 492–497
Sugatani J, Sueyoshi T, Negishi M, Miwa M 2005 Regulation of the human UGT1A1 gene by nuclear receptors constitutive active/androstane receptor, pregnane X receptor, and glucocorticoid receptor. Methods Enzymol 400: 92–104
Yoshinari K 2006 [Roles of nuclear receptors in the gene expression of drug-metabolizing enzymes under various physiological conditions]. Yakugaku Zasshi 126: 343–348
Xie W, Yeuh MF, Radominsha-Pandya A, Saini SP, Negishi Y, Bottroff BS, Cabrera GY, Tukey RH, Evans RM 2003 Control of steroid, heme, and carcinogen metabolism by nuclear pregnane X receptor and constitutive androstane receptor. Proc Natl Acad Sci U S A 100: 4150–4155
Huang W, Zhang J, Chua SS, Qatanani M, Han Y, Granata R, Moore DD 2003 Induction of bilirubin clearance by the constitutive androstane receptor (CAR). Proc Natl Acad Sci U S A 100: 4156–4161
Matsui K, Maruo Y, Sato H, Takeuchi Y 2010 Combined effect of regulatory polymorphisms on transcription of UGT1A1 as a cause of Gilbert syndrome. BMC Gastroenterol 10: 57–65
Auerbach SS, Ramsden R, Stoner MA, Verlinde C, Hassett C, Omiecinski CJ 2003 Alternatively spliced isoforms of the human constitutive androstane receptor. Nucleic Acids Res 31: 3194–3207
Lehmann JM, Mckee DD, Watson MA, Willson TM, Moore JT, Kliewer SA 1998 The human orphan nuclear receptor PXR is activated by compounds that regulate CYP3A4 gene expression and cause drug interactions. J Clin Invest 102: 1016–1023
Maruo Y, Serdaroglu E, Iwai M, Takahashi H, Mori A, Bak M, Calkavur S, Sato H, Takeuchi Y 2003 A novel missense mutation of bilirubin UDP-glucuronosyltransferase gene in a Turkish patient with Crigler-Najjar syndrome type1. J Pediatr Gastroenterol Nutr 37: 627–630
Ritter JK, Chen F, Sheen YY, Tran HM, Kimura S, Yeatman MT, Owens IS 1992 A novel complex locus UGT1 encodes human bilirubin, phenol, and other UDP-glucuronosyltransferase isozymes with identical carboxyl termini. J Biol Chem 267: 3257–3261
Sugatani J, Kojima H, Ueda A, Kakizaki S, Yoshinari K, Gong QH, Owens IS, Negishi M, Sueyoshi T 2001 The phenobarbital response enhancer module in the human bilirubin UDP-glucuronosyltransferase UGT1A1 gene and regulation by the nuclear CAR. Hepatology 33: 1232–1238
Buckley DB, Klaassen CD 2009 Induction of mouse UDP-glucuronosyltransferase mRNA expression in liver and intestine by activators of aryl-hydrocarbon receptor, constitutive androstane receptor, pregnane X receptor, peroxisome proliferator-activated receptor α, and nuclear factor erythroid 2-related factor 2. Drug Metab Dispos 37: 847–856
Onishi S, Kawade N, Itoh S, Isobe K, Sugiyama S 1979 Postnatal development of uridine diphosphate glucuronyltransferase activity towards bilirubin and 2-aminophenol in human liver. Biochem J 184: 705–707
Bancroft JD, Kreamer B, Gourley GR 1998 Gilbert syndrome accelerates development of neonatal jaundice. J Pediatr 132: 656–660
Monaghan G, McLellan A, McGeehan A, Li Volti S, Mollica F, Salemi I, Din Z, Cassidy A, Hume R, Burchell B 1999 Gilbert's syndrome is a contributory factor in prolonged unconjugated hyperbilirubinemia of the newborn. J Pediatr 134: 441–446
Fujiwara R, Nguyen N, Chen S, Tukey RH 2010 Developmental hyperbilirubinemia and CNS toxicity in mice humanized with the UDP-glucuronosyltransferase 1 (UGT1) locus. Proc Natl Acad Sci U S A 107: 5024–5029
Kulski JK, Smith M, Hartmann PE 1977 Perinatal concentrations of progesterone, lactose and alpha-lactalbumin in the mammary secretion of women. J Endocrinol 74: 509–510
Kulski JK, Hartmann PE 1981 Changes in the concentration of cortisol in milk during different stages of human lactation. Aust J Exp Biol Med Sci 59: 769–778
McGarrigle HH, Lachelin GC 1983 Oestrone, oestradiol and oestriol glucosiduronates and sulphates in human puerperal plasma and milk. J Steroid Biochem 18: 607–611
Severi F, Rondini G, Zaverio S, Vegni M 1970 Prolonged neonatal hyperbilirubinemia and pregnane-3(α),20(β)-diol in maternal milk. Helv Paediatr Acta 25: 517–521
Acknowledgements
We thank M. Suzaki of the Central Research Laboratory, Shiga University of Medical Science for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors report no conflicts of interest.
Rights and permissions
About this article
Cite this article
Ota, Y., Maruo, Y., Matsui, K. et al. Inhibitory Effect of 5β-Pregnane-3α,20β-Diol on Transcriptional Activity and Enzyme Activity of Human Bilirubin UDP-Glucuronosyltransferase. Pediatr Res 70, 453–457 (2011). https://doi.org/10.1203/PDR.0b013e31822f242e
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31822f242e
This article is cited by
-
Gilbert or Crigler–Najjar syndrome? Neonatal severe unconjugated hyperbilirubinemia with P364L UGT1A1 homozygosity
Italian Journal of Pediatrics (2022)
-
Physiologically Based Pharmacokinetic Modeling Framework to Predict Neonatal Pharmacokinetics of Transplacentally Acquired Emtricitabine, Dolutegravir, and Raltegravir
Clinical Pharmacokinetics (2021)
-
Inherited disorders of bilirubin clearance
Pediatric Research (2016)
-
Contribution of UGT1A1 variations to chemotherapy-induced unconjugated hyperbilirubinemia in pediatric leukemia patients
Pediatric Research (2016)
-
Development of icterus gravis in a preterm infant with G71R UGT1A1 polymorphism
BMC Research Notes (2013)