Abstract
Modifications to diagnostic criteria and introduction of genetic testing have likely affected the pattern and timing of Rett syndrome diagnosis. The trends in incidence and prevalence of Rett syndrome in Australia were examined; the cumulative risk of a female being diagnosed was determined; and the impact of changes to diagnostic criteria and availability of genetic testing on these frequencies was investigated. The population-based Australian Rett Syndrome Database was used to identify a total of 349 verified Rett syndrome females born 1976–2006 and diagnosed 1982–2008. The proportion of female cases born and diagnosed per year and the cumulative risk of a diagnosis were determined. The median age of Rett syndrome diagnosis decreased from 4.5 y if diagnosed before 2000 to 3.5 y if diagnosed after 1999. The cumulative risk of diagnosis had almost doubled by 32 y of age [1/8,905 or 11.23 per 100,000 person-years (95% CI, 10.03–12.45)] in comparison with 5 y of age [1/15,361 or 6.51 per 100,000 person-years (95% CI, 5.65–7.39)]. Earlier age of diagnosis may result in families experiencing less stress and emotional strain compared with those with delayed diagnosis.
Similar content being viewed by others

Main
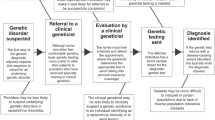
Rett syndrome (RTT), a severe neurodevelopment disorder occurring most frequently in females, has only been recognized worldwide since 1983 (1). The 1985 “Vienna criteria” were the first to define its “classical” characteristics (2). Additional case series (3,4) served as a framework for the establishment of updated guidelines (1988) (5) that included a set of supportive criteria and removed female sex as mandatory. Only in 1994 (6) were criteria for defining atypical variants developed, allowing those with more severe phenotypes such as the “congenital RTT variant” (7) and those with milder phenotypes such as the “preserved speech variant” (8) to be recognized within the RTT spectrum.
In 1999, mutations within the Methyl-CpG Binding Protein 2 gene (MECP2) were identified as the major cause of RTT (9). This allowed molecular confirmation of clinical cases and contributed to additional amendment of diagnostic criteria (2002) (10). The likelihood of genetic confirmation has increased with both the introduction of Multiplex Ligation-dependent Probe Amplification (MLPA) (11), which detects large deletions, and through the identification of causative mutations in exon 1 (12).
Early epidemiological studies have reported varying estimates of RTT although most studies were conducted before 1999 and did not necessarily define the inclusion or otherwise of atypical cases (Table 1) (13–28). Recent studies (20,27) varied in their ascertainment methods, inclusion criteria, measures of frequency, sample size, and methods of analysis, making comparisons difficult. For example, exclusion of mutation negative (13) or atypical cases (27) could partly explain why the prevalence in France (0.58 per 10,000 females aged 4–15 y) (13) and Hong Kong (0.57 per 10,000 females 35 y or younger) (27) were only two thirds of that in Australia (0.88 per 10,000 females aged 5–18 y) (20).
Changes in clinical practice resulting both from modifications to diagnostic criteria and the introduction of genetic testing have likely affected the pattern and timing of RTT diagnosis. This article describes the changing incidence and prevalence of RTT in Australia and examines if and why diagnostic practices may have changed over time.
METHODS
The Australian Rett Syndrome Database (ARSD), established in 1993, is a population-based database of RTT cases born since 1976 (21). Study approval was obtained from the Human Research Ethics Committee of Princess Margaret Hospital, and families provided informed consent before participating. Diagnosed cases are ascertained through multiple sources including the Australian Paediatric Surveillance Unit (APSU) (29). The APSU was established in 1993 and has since actively surveyed ∼43 childhood conditions (30). Pediatricians and other medical child health specialists receive a monthly report card by e-mail (or mail in 20%) and are requested to indicate by return whether in the last month they have seen any newly diagnosed cases of any of the conditions listed. If they have, the researcher is notified by the APSU (31,32). The researcher can then contact the doctor about collecting further information. The diagnosis of RTT is usually made by child neurologists, clinical geneticists, and general or developmental pediatricians. At the time of the study, only clinically suspected cases verified by the presence of a MECP2 pathogenic mutation or by fulfilment of the 2002 diagnostic criteria (10) for classical or atypical RTT were included in this study. Contact has been maintained with families via the administration of follow-up questionnaires at approximately two yearly intervals since 1996.
Trends in birth prevalence (the proportion of Australian female births with RTT) by birth year and incidence of diagnosis (the number of girls diagnosed out of the pool of those eligible for diagnosis) each calendar year were examined by investigating the cohort- and period-related effects, respectively, during the study period (1976–2008) and by replicating methods used in a recent population-based study assessing autism spectrum disorders (33). The cumulative risk or probability of a girl being diagnosed with RTT by a certain age was also calculated and estimated separately for the periods before and during or after 1999, when the genetic cause of RTT was identified. The 2009 point prevalence of RTT (the proportion of the female population of that age range alive with RTT in that year) in females aged 5–32 y was also calculated and estimated separately for those aged 5–18 y and those aged 19–32 y.
Cohort-related effect.
With the cohort effect, we examined how the birth prevalence (the proportion of Australian female births with RTT) changed by birth year for each year from 1976 to 2006. We used birth prevalence because the condition RTT is already present, although not clinically apparent, at birth as in congenital malformations. Therefore, birth prevalence is the most suitable measure applicable (34). For the birth prevalence (expressed per 100,000 live female births), the numerator comprised all females born in Australia in that birth year and diagnosed with RTT between 1982 and 2008 and the denominator was the number of live female births in Australia for the given birth year (35,36). The birth prevalence (regardless of MECP2 mutation status) was determined separately for cases classified as either “Classical” or “Atypical” to investigate the change over time of the recognition of variable phenotypes. Confidence intervals were calculated assuming a binomial distribution.
Period-related effect.
With the period effect, we examined how the occurrence of RTT diagnosis changed by calendar year by investigating the annual incidence over time. The incidence (the number of girls diagnosed out of the pool of those eligible for diagnosis) was based on all female cases born since 1976 and diagnosed each calendar year from 1982 to 2008 divided by all females at risk of diagnosis in a particular calendar year from 1982 to 2008 and expressed per 100,000 female years. For example, in 1982, only girls aged up to 6 y were included, whereas in 1993, girls aged up to 17 y were included. Population data were obtained from the Australian Bureau of Statistics Estimated Resident Population (ERP) (37). The ERP is based on the 2006 Census of Population and Housing and estimates the resident population of Australian states and territories by single year of age and by sex as at June 30 of each reference year. This includes all Australian residents irrespective of their place of birth or resident status but excludes foreign diplomatic personnel and their families. Specific events and time periods related to the diagnosis were then marked on the plot of the annual incidence.
Changes in the age group specific trend per birth year and per diagnostic year were also calculated for children diagnosed at the ages of between 0–3, 4–7, 8–11, and ≥12 y of age. These age groups were used so that the youngest ages of possible diagnosis were represented without being influenced by the most frequently diagnosed age group (4–7 y).
The cumulative risk (likelihood of a female child being diagnosed with RTT by a certain age) was estimated using survival analysis. Population denominators from the ERP (37) were used to calculate female person-years at risk for those without a RTT diagnosis, such that each individual at risk of diagnosis in each calendar year contributed one person-year of risk. The survival curve was then calculated using the Kaplan-Meier survival function (38) and risk evaluated as 1 − the survival function at each age (expressed per 100,000 females). Separate curves were derived for cases diagnosed before and during or after 1999 and their equality compared using the log-rank test. Cox regression was used to estimate the hazard ratio (HR) for the two time periods.
The 2009 point prevalence of females with RTT aged between 5 and 32 y was defined as follows. The numerator was the number of cases aged 5–32 y alive on the June 30, 2009, and the denominator, obtained from the ERP (37), was the number of females in the Australia population within this age range. The point prevalence was calculated separately for those aged between 5 and 18 y and those aged 19 y and older in 2009.
The age of RTT diagnosis was obtained from either the family or clinician questionnaires. If no age of diagnosis was available, a surrogate age was estimated using multiple sources of information including date of ascertainment, date of genetic testing, or through contact with families. All records were updated with date of death or date last known to be alive as of December 31, 2009 (estimated from the last contact with the families or their clinician). We also linked the cohort to the National Death Index housed at the Australian Institute of Health and Welfare to determine whether any of the subjects had died since their last contact with the study. Ethics approval was received from the Australian Institute of Health and Welfare for the linkage to the National Death Index.
RESULTS
As of December 31, 2009, the ARSD contained information on a total of 349 females (of whom 44 were deceased) born between 1976 and 2006 and diagnosed with RTT between 1982 and 2008. Age of diagnosis ranged from 1 to 28 y of age (mean, 5.5 y; 95% CI, 5.04–5.96; Table 2). There was a decreasing trend in age of diagnosis from 6.04 y for those born 1999 or before to 3.03 y for those born after 1999. The point prevalence of RTT in Australia on June 30, 2009, was 8.6 per 100,000 females (95% CI, 7.4–10.1) aged 5–18 y and 5.8 per 100,000 females (95% CI, 4.8–6.9) aged 19–32 y.
The birth prevalence varied by birth year (Table 2), peaking for those born in the early to mid-1990s. For classical RTT, there was a steep upward trend until 1988 followed by a rapid decline with a later increase for atypical cases (Fig. 1). In those younger than 4 y, the birth prevalence increased from 1985, although in other age groups it remained consistent over time (Fig. 2).
The period effect is shown in Figure 3, starting with the first English-speaking publication of RTT in 1983 (1). Peaks in incidence occurred after the publication of each set of diagnostic criteria and following the establishment of the ARSD in 1993 and its subsequent systematic case ascertainment (21). A further peak occurred with the introduction of MECP2 testing in the early 2000s. The subsequent availability of testing with MLPA (11) seemed to have had little further impact.
Initially, RTT was diagnosed most commonly in those aged 4–11 y. From 1986 onward, diagnosis became more frequent in those younger than 4 y, whereas fewer diagnoses were made in those older than 12 y (Fig. 4). The age at diagnosis decreased from a median of 4.5 y before 1999 to 3.5 y afterward (log-rank test p = 0.01; Fig. 5). This is equivalent to a 32% increase in risk of diagnosis (HR, 1.32; 95% CI, 1.06–1.63) from 1999 onward. Generally, more than half of all girls would be diagnosed by the age of 5 y. This represented a cumulative risk of 6.51 per 100,000 person-years (95% CI, 5.65–7.39) or a likelihood of 1 in 15,361 Australian girls being diagnosed with RTT by the age of 5 y; increasing to 1 in 10,299 (9.71 per 100,000 person-years (95% CI, 8.64–10.78) by the age of 12 y and 1 in 8,905 (11.23 per 100,000 person-years (95% CI, 10.03–12.45) by the age of 32 y.
DISCUSSION
This is the first study to investigate changing trends in RTT diagnosis. The mean age at diagnosis in Australia decreased over time from ∼6 y for those born before 2000 to 3 y of age for those born since 2000, although a small proportion of cases were still diagnosed at a later age. Active case ascertainment through the ARSD (21) and the introduction of genetic testing (9) seem to have resulted in the subsequent identification of many previously undiagnosed individuals born since 1976. The recognition of atypical relative to classical RTT has also increased over time, suggesting better awareness of clinical variation. However, the low birth prevalence in girls born after 2003 shows that some lag time to diagnosis may still persist.
We acknowledge that obtaining complete case ascertainment for a rare disease is challenging. However, the strengths of this study are that it was population-based and used an active system for ascertaining rare pediatric disorders in Australia. Moreover, one of the sources of ascertainment, the APSU, has been found to meet all the necessary criteria developed by the Centres for Disease Control and Prevention for the evaluation of surveillance systems (30). We have also previously shown that in comparison with international data, there seems to be no socioeconomic bias in regards to age at diagnosis of RTT in Australia (39). The use of multiple sources (provided often by clinician and family) to determine age at diagnosis both strengthens the precision and reduces possible recall bias. Thus, our data are likely to be representative of RTT in Australia and unbiased in that respect. One unavoidable shortcoming, however, is the restriction to those born 1976 and onward. In the absence of a mechanism to ascertain adult women with RTT in Australia in a systematic and comprehensive way, this restriction was felt to be the only way to maintain the rigor of the register. On the other hand, were some girls with RTT to have died before diagnosis, as is possible, we may have minimally under-ascertained the birth prevalence. Furthermore, we only have information on the number of diagnoses made not the number of genetic tests requested to confirm these and other diagnoses. However, we have demonstrated possible effects of the changing of diagnostic criteria (2,5,6,10,40) over time on the clinical identification, epidemiology, and monitoring of trends in RTT. However, this impact has been less deleterious than the effects seen with autism spectrum disorders over the past few decades (33).
Thirteen of the 16 previous epidemiological studies (Table 1) were conducted before the discovery of causative mutations within MECP2. Cases were usually ascertained through a single contact with specialists (14–18,25,27), child health departments (22,23,28) or education departments (15,27), institutions (14,25), and special schools (14,15,24,26), although some used population-based sources (19–21). In one study, case ascertainment involved contacting laboratories for MECP2 positive individuals or analysis of precollected blood from a family RTT organization (13), and only cases with a pathogenic MECP2 mutation were included. There are few study groups (17,20) that have followed their cohort over time and therefore, RTT may have been previously under-ascertained.
Frequency measures have also varied in that in some studies the term “incidence” was used (13,18) (expressed, by one study, as per 10,000 births) (18) and considered by another study as an estimate of the prevalence (13). Where the term incidence has been used, the denominators have been the annual female births, and the numerator the number of RTT cases for that period in question. For “prevalence,” the denominators have also differed with some studies using the female population at risk and others the number of female births per year. It is generally unclear whether incidence, birth prevalence, or current point prevalence were actually measured (41). In the latter, any deceased cases should be excluded from the numerator and this may or may not have been done. Subject numbers have also varied from one (26) to 274 (20). Some studies have been restricted to classical cases (14–18,25–28) and one to only mutation positive individuals (13). The variation in age boundaries from 0 y to the highest age possible can often cause an underestimate of the prevalence due to an increased denominator. Although RTT is a condition present from birth, its observable onset is generally between 6 and 18 mo and thus an earlier diagnosis is unlikely.
The age-specific trends were similar for both year of birth and year of diagnosis, in that diagnosis in the younger age groups increased, and for older cases, it remained fairly consistent over time. One difference is the peak in 4–7 y olds being diagnosed between 2003 and 2005, which is not mirrored by any changes in the birth prevalence for this age group, and a decrease in birth prevalence for the 8–11 y olds from 1995 onward. This may signify that children were being diagnosed younger. In general, the calendar year of diagnosis seems to have had more of an impact than the year of birth, with significant research events in the history of RTT increasing the number of diagnoses being made.
Our RTT frequency estimates were generally higher than in previous studies. Given the phenotypic variability in this disorder (42), it is important not to exclude or at least to separately define atypical cases, but this was only done in seven of 16 studies (19–24), whereas another was restricted to mutation positive cases (13). Our population-based database with assisted recruitment by the APSU (29) will have enhanced ascertainment and, therefore, have reported higher subject numbers than studies not using active population-based methods of surveillance. Our prevalence was also higher than the 1993 population-based Texas study (19), which was undertaken before the identification of the relationship with MECP2 and may have under-ascertained atypical cases, which tend to be diagnosed at an older age (39). Through genetic testing and the identification of additional genes that can cause Rett-like symptoms, a broader spectrum of RTT phenotypes has emerged (7,42,43), from a very severe early onset presentation to one which is much milder. In recent years in Australia, the number of cases diagnosed with atypical has approached that of classical RTT, indicating an increase in the identification of atypical presentations and improvement in diagnostic practice.
Cumulative risk has only been estimated in Australia where the necessary population-based register exists (20,21). It provides an accurate estimate of the risk of RTT diagnosis by age and is a useful and intuitive measure. The change in cumulative risk before and after 1999 shows a clear increase in the risk of RTT diagnosis and a parallel decrease in age of diagnosis. The highest prevalence was in those aged between 5 and 18 y, with a decrease in those aged 19 y and older. This decrease would be expected in line with the increased mortality in older girls and women (20). In combination, these measures provide vital information about the diagnostic pattern of RTT over time so that we can discern whether the age of diagnosis has actually decreased or whether this is an artifact due to the absence of cases generally not diagnosed till older. An earlier diagnosis is important for families in that it provides them with the ability to come to terms with the cause of their child's symptoms, to have a label for their child's condition, obtain earlier access to appropriate services, and receive support from within parents' organizations (44).
The European Organization for Rare Diseases suggests that 6–8% of the European population suffer from a rare disease (45), so that together these conditions are no longer rare. Many rare disorders impact not only on those diagnosed but also on their family, society, and the healthcare system. Limited information and research into rare diseases means that those people who suffer from them usually have delayed diagnosis and limited access to support and services. Receiving an earlier diagnosis provides families with mechanisms to cope and move on with their lives, whereas a delayed diagnosis may result in families experiencing potentially avoidable stress and emotional or financial strain. It is essential that appropriate and comparable methods, which are population-based wherever possible, be used to research the epidemiology of RTT. Only then can real changes in incidence and prevalence over time and differences across countries be identified. Such methods will also help identify inequality in access to diagnostic services between and within countries, any true ethnic variation and any possible environmental exposures that might predispose to occurrence of the causative MECP2 mutations.
Abbreviations
- APSU:
-
Australian Paediatric Surveillance Unit
- ARSD:
-
Australian Rett Syndrome Database
- ERP:
-
Estimated Residential Population
- MECP2 :
-
Methyl-CpG Binding Protein 2
- RTT:
-
Rett Syndrome
References
Hagberg B, Aicardi J, Dias K, Ramos O 1983 A progressive syndrome of autism, dementia, ataxia, and loss of purposeful hand use in girls: Rett's syndrome: report of 35 cases. Ann Neurol 14: 471–479
Hagberg B, Goutieres F, Hanefield F, Rett A, Wilson J 1985 Rett Syndrome: criteria for inclusion and exclusion. Brain Dev 7: 372–373
Naidu S, Murphy M, Moser HW, Rett A 1986 Rett syndrome—natural history in 70 cases. Am J Med Genet Suppl 1: 61–72
Hagberg B, Witt-Engerström I 1986 Rett syndrome: a suggested staging system for describing impairment profile with increasing age towards adolescence. Am J Med Genet Suppl 1: 47–59
Trevathan E, Moser HW 1988 Diagnostic criteria for Rett syndrome. The Rett Syndrome Diagnostic Criteria Work Group. Ann Neurol 23: 425–428
Hagberg BA 1994 Rett variants: a suggested model for inclusion criteria. Pediatr Neurol 11: 5–11
Ariani F, Hayek G, Rondinella D, Artuso R, Mencarelli MA, Spanhol-Rosseto A, Pollazzon M, Buoni S, Spiga O, Ricciardi S, Meloni I, Longo I, Mari F, Broccoli V, Zappella M, Renieri A 2008 FOXG1 is responsible for the congenital variant of Rett syndrome. Am J Hum Genet 83: 89–93
Zappella M, Gillberg C, Ehlers S 1998 The preserved speech variant: a subgroup of the Rett complex: a clinical report of 30 cases. J Autism Dev Disord 28: 519–526
Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY 1999 Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nat Genet 23: 185–188
Hagberg B, Hanefeld F, Percy AK, Skjeldal OH 2002 An update on clinically applicable diagnostic criteria in Rett syndrome. Comments to Rett syndrome clinical criteria consensus panel satellite to European Paediatric Neurology Society Meeting, Baden Baden, Germany, September 11, 2001. Eur J Paediatr Neurol 6: 293–297
Erlandson A, Samuelsson L, Hagberg B, Kyllerman M, Vujic M, Wahlstrom J 2003 Multiplex ligation-dependent probe amplification (MLPA) detects large deletions in the MECP2 gene of Swedish Rett syndrome patients. Genet Test 7: 329–332
Amir RE, Fang P, Yu Z, Glaze DG, Percy AK, Zoghbi HY, Roa BB, Van den Veyver IB 2005 Mutations in exon 1 of MECP2 are a rare cause of Rett syndrome. J Med Genet 42: e15
Bienvenu T, Philippe C, De Roux N, Raynaud M, Bonnefond JP, Pasquier L, Lesca G, Mancini J, Jonveaux P, Moncla A, Feingold J, Chelly J, Villard L 2006 The incidence of Rett syndrome in France. Pediatr Neurol 34: 372–375
Boltshauser E, Kunzle C 1987 Prevalence of Rett syndrome in Switzerland. Helv Paediatr Acta 42: 407–411
Burd L, Vesley B, Martsolf JT, Kerbeshian J 1991 Prevalence study of Rett syndrome in North Dakota children. Am J Med Genet 38: 565–568
Hagberg B 1985 Rett's syndrome: prevalence and impact on progressive severe mental retardation in girls. Acta Paediatr Scand 74: 405–408
Hagberg B, Witt-Engerström I 1987 Rett syndrome: epidemiology and nosology—progress in knowledge 1986—a conference communication. Brain Dev 9: 451–457
Kerr AM, Stephenson JB 1985 Rett's syndrome in the west of Scotland. BMJ (Clin Res Ed) 291: 579–582
Kozinetz CA, Skender ML, MacNaughton N, Almes MJ, Schultz RJ, Percy AK, Glaze DG 1993 Epidemiology of Rett syndrome: a population-based registry. Pediatrics 91: 445–450
Laurvick CL, de Klerk N, Bower C, Christodoulou J, Ravine D, Ellaway C, Williamson S, Leonard H 2006 Rett syndrome in Australia: a review of the epidemiology. J Pediatr 148: 347–352
Leonard H, Bower C, English D 1997 The prevalence and incidence of Rett syndrome in Australia. Eur Child Adolesc Psychiatry 6: 8–10
Pini G, Milan M, Zappella M 1996 Rett syndrome in Northern Tuscany (Italy): family tree studies. Clin Genet 50: 486–490
Skjeldal OH, Vontetzchner S, Aspelund F, Herder GA, Lofterod B 1997 Rett syndrome—geographic variation in prevalence in Norway. Brain Dev 19: 258–261
Suzuki H, Hirayama Y, Arima M 1989 [Prevalence of Rett syndrome in Tokyo]. No To Hattatsu 21: 430–433
Talvik T, Soot A, Beilmann A, Soopld T, Nurk K 1995 Rett syndrome in Estonia: prevalence of the classical phenotype. Acta Paediatr 84: 1070–1071
Terai K, Munesue T, Hiratani M, Jiang ZY, Jibiki I, Yamaguchi N 1995 The prevalence of Rett syndrome in Fukui prefecture. Brain Dev 17: 153–154
Wong VC, Li SY 2007 Rett syndrome: prevalence among Chinese and a comparison of MECP2 mutations of classic Rett syndrome with other neurodevelopmental disorders. J Child Neurol 22: 1397–1400
Zappella M, Cerioli M 1987 High prevalence of Rett syndrome in a small area. Brain Dev 9: 479–480
Elliott EJ, Chant KG 1994 Rare disease surveillance. J Paediatr Child Health 30: 463–465
He S, Zurynski YA, Elliott EJ 2009 Evaluation of a national resource to identify and study rare diseases: the Australian Paediatric Surveillance Unit. J Paediatr Child Health 45: 498–504
Zurynski Y, Davey E, Elliot EJ 2010 Australian Paediatric Surveillance Unit annual report, 2008 and 2009. Commun Dis Intell 34: 285–290
Srikanthan S, Zurynski Y, Elliott E 2008 APSU Australian Paediatric Surveillance Unit: Celebrating 15 Years of Surveillance 1993–2007. Australian Paediatric Surveillance Unit, Westmead,
Nassar N, Dixon G, Bourke J, Bower C, Glasson E, de Klerk N, Leonard H 2009 Autism spectrum disorders in young children: effect of changes in diagnostic practices. Int J Epidemiol 38: 1245–1254
Rothman KJ, Greenland S, Lash TL 2008 Modern Epidemiology. Wolters Kluwer Health/Lippincott Williams & Wilkins, Philadelphia, p 47
Australian Bureau of Statistics 3105.0.65.001 Australian historical population statistics, 2006, Table 36. Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3105.0.65.0012006?OpenDocument. Accessed October 20, 2009
Australian Bureau of Statistics 2007.3301.0 Births, Australia, 2007, Table 1. Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3301.02007?OpenDocument. Accessed October 20, 2009
Australian Bureau of Statistics 2009 3201.0 Population by age and sex, Australian states and territories, Table 9.1. Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3201.0Jun%202008?OpenDocument. Accessed October 20, 2009
Kaplan EL, Meier P 1958 Nonparametric estimation from incomplete observations. J Am Stat Assoc 53: 457–481
Fehr S, Downs J, Bebbington A, Leonard H 2010 Atypical presentations and specific genotypes are associated with a delay in diagnosis in diagnosis in females with Rett syndrome. Am J Med Genet A 152: 2535–2542
Neul JL, Kaufmann WE, Glaze DG, Christodoulou J, Clarke AJ, Bahi-Buisson N, Leonard H, Bailey ME, Schanen NC, Zappella M, Renieri A, Huppke P, Percy AK, RettSearch Consortium 2010 Rett syndrome: revised diagnostic criteria and nomenclature. Ann Neurol 68: 944–950
Last JM, Spasoff RA, Harris SS, Thuriaux MC, International Epidemiological Association 2001 A Dictionary of Epidemiology. Oxford University Press, New York,
Bebbington A, Anderson A, Ravine D, Fyfe S, Pineda M, de Klerk N, Ben-Zeev B, Yatawara N, Percy AK, Kaufmann WE, Leonard H 2008 Investigating genotype-phenotype relationships in Rett syndrome using an international dataset. Neurology 70: 868–875
Mari F, Azimonti S, Bertani I, Bolognese F, Colombo E, Caselli R, Scala E, Longo I, Grosso S, Pescucci C, Ariani F, Hayek G, Balestri P, Bergo A, Badaracco G, Zappella M, Broccoli V, Renieri A, Kilstrup-Nielsen C, Landsberger N 2005 CDKL5 belongs to the same molecular pathway of MeCP2 and it is responsible for the early-onset seizure variant of Rett syndrome. Hum Mol Genet 14: 1935–1946
Graungaard AH, Skov L 2007 Why do we need a diagnosis? A qualitative study of parents' experiences, coping and needs, when the newborn child is severely disabled. Child Care Health Dev 33: 296–307
European Organisation for Rare Diseases 2005 Rare diseases: understanding this public health priority. Available at: http://www.eurordis.org/IMG/pdf/princeps_document-EN.pdf. Accessed March 18, 2009
Acknowledgements
We thank the families who have participated in the Australian Rett syndrome study. We also gratefully acknowledge the clinicians who completed questionnaires and extend our gratitude to the Australian Pediatric Surveillance Unit (APSU) and the Australian Rett syndrome Association for their ongoing support in case ascertainment in Australia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the National Institute of Health grant 5R01HD043100-05, NHMRC #303189. H.L. was previously funded by a NHMRC program grant (#353514) and current funding is from an NHMRC Senior Research Fellowship #572568. N.N. is funded by a NHMRC Career Development Award (#632955).
Rights and permissions
About this article
Cite this article
Fehr, S., Bebbington, A., Nassar, N. et al. Trends in the Diagnosis of Rett Syndrome in Australia. Pediatr Res 70, 313–319 (2011). https://doi.org/10.1203/PDR.0b013e3182242461
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3182242461
This article is cited by
-
Rett syndrome in Ireland: a demographic study
Orphanet Journal of Rare Diseases (2024)
-
Global prevalence of Rett syndrome: systematic review and meta-analysis
Systematic Reviews (2023)
-
Non-Verbal Social Skills Assessment in Rett Syndrome: a Systematic Review
Review Journal of Autism and Developmental Disorders (2023)
-
A brief history of MECP2 duplication syndrome: 20-years of clinical understanding
Orphanet Journal of Rare Diseases (2022)
-
A Phase 1, Open-Label Study to Evaluate the Effects of Food and Evening Dosing on the Pharmacokinetics of Oral Trofinetide in Healthy Adult Subjects
Clinical Drug Investigation (2022)



 , birth prevalence of girls with atypical Rett syndrome.
, birth prevalence of girls with atypical Rett syndrome.


