Abstract
NO is involved in normal kidney function and perturbed in acute kidney injury (AKI). We hypothesized that urinary concentration of NO metabolites, nitrite, and nitrate would be lower in children with early AKI presenting to the emergency department (ED), when serum creatinine (SCr) was uninformative. Patients up to 19 y were recruited if they had a urinalysis and SCr obtained for routine care. Primary outcome, AKI, was defined by pediatric Risk, Injury, Failure, Loss of function, End-stage renal disease (pRIFLE) criteria. Urinary nitrite and nitrate were determined by HPLC. A total of 252 patients were enrolled, the majority (93%) of whom were without AKI. Although 18 (7%) had AKI by pRIFLE, 50% may not have had it identified by the SCr value alone at the time of visit. Median urinary nitrate was lower for injury versus risk (p = 0.03); this difference remained significant when the injury group was compared against the combined risk and no AKI groups (p = 0.01). Urinary nitrite was not significantly different between groups. Thus, low urinary nitrate is associated with AKI in the pediatric ED even when SCr is normal. Predictive potential of this putative urinary biomarker for AKI needs further evaluation in sicker patients.
Similar content being viewed by others
Main
Acute kidney injury (AKI), previously referred to as acute renal failure (ARF), is a common complication among ambulatory and hospitalized patients (1,2). The incidence of AKI varies from 5% in hospitalized patients to 30–82% of patients in intensive care units (ICUs) (3,4). Children who are or will get critically ill from AKI are likely to pass through the emergency department (ED). From the ED perspective, knowing the type and/or severity of AKI will help in the judicious usage of fluid therapy; being more liberal in administering fluid in fluid responsive (e.g. prerenal azotemia) AKI versus otherwise (fluid nonresponsive, e.g. acute tubular necrosis). Early diagnosis will also help avoid usage of potential nephrotoxic medication in the ED.
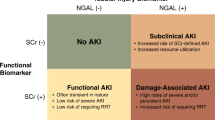
The gold standard kidney function marker, serum creatinine (SCr), is a poor one for AKI, only rising at a relatively late stage of kidney injury when intervention is unlikely to be of benefit. AKI diagnosis is currently based on SCr increase from baseline or absolute SCr values above a certain threshold (4–6). Recent data on urinary biomarkers for AKI in the adult ED have shown that a single novel urinary biomarker, neutrophil gelatinase-associated lipocalin (NGAL), was predictive of hospitalization, need for dialysis, and patient mortality, at a time when SCr was uninformative (7). Shapiro et al. (8) showed that in patients with suspected sepsis in the ED, an increased plasma NGAL concentration was associated with the development of AKI. Thus, there is potential benefit for the discovery and validation of biomarkers for AKI in the ED setting (9,10). We have recently shown that urinary NGAL, independently as well as part of a panel, was able to accurately predict AKI in the pediatric ED, even in cases where SCr was normal (11). Ultimately, it is conceivable that a panel of urinary biomarkers may be needed for better outcomes of AKI. Thus, there is a significant unmet need to describe additional early biomarkers that can be diagnostic and prognostic of AKI in the pediatric ED, at a time when baseline SCr is often unavailable.
NO, a gaseous signaling molecule, is shown to have several functions in the kidney, depending on its concentration, site of release, and duration of action (12). Lack of NO generation by a specific isoform of NO synthase may reflect endothelial damage in the kidney after ischemia-reperfusion (12,13), the leading cause of acute tubular necrosis type of AKI. In an adult postischemic model of AKI, urinary concentration of NO (as measured by its metabolites nitrate and nitrite) was markedly lower, suggesting that this was a reflection of potential endothelial damage in the kidney (13). These may be potential biomarkers for the disease. Thus, we conducted this study to test the hypothesis that urinary concentration of NO metabolites, nitrite, and nitrate would be decreased in early AKI in children presenting to the ED.
METHODS
Study design, study setting, and population.
We performed a cross-sectional single-center evaluation of multiple urinary biomarkers in children who presented to the Texas Children's Hospital ED in Houston, TX, from January 1 through March 31, 2009. Patients were included if the ED physician ordered a SCr and urine test as part of the standard of care for evaluation. Urine was collected in the same manner in all patients using age-appropriate techniques (catheter or fresh void). Patients were excluded if they had a known diagnosis of chronic kidney disease including dialysis or transplantation. Patient caregivers provided informed written consent. The protocol and consent forms were approved by the Baylor College of Medicine Institutional Review Board before study commencement (IRB#H-24243).
Study protocol.
We assessed the following data at the time of the ED visit: patient age, gender, height, weight, ethnicity, and vital signs. We also recorded the primary diagnosis listed on the ED visit written medical record and categorized these diagnoses by primary organ involvement. If the patient was admitted to the hospital, we recorded the primary medical or surgical service of record, length of hospitalization and need for ICU admission, and/or renal replacement therapy.
Laboratory data.
Data from the ED that were required for entry into the study included SCr and urinalysis. We also recorded any other relevant laboratory data including complete blood counts, serum and urine electrolytes, and liver and pancreatic enzymes. If the patient was admitted, we recorded subsequent SCr values obtained as part of the patient's clinical course; no additional laboratory values were obtained as part of this study.
Urinary biomarker assessment.
Urine was obtained for biomarker assessment at the time of urinalysis collection in the ED. Five milliliters of urine was obtained, spun at 3000 rpm for 15 min, and then the supernatant decanted into five 1-mL aliquots and stored at −80°C. Combined nitrate and nitrite (NOx) analysis was performed in the laboratory of one of the authors (N.S.B.) by a dedicated ENO-20 HPLC System (EiCom Corporation, San Diego, CA) (14). This system is sensitive and selective for the measurement of NOx in all biological matrices and has the capacity for high throughput. In brief, to separate nitrite and nitrate, the nitrate was first reduced to nitrite through a reaction with cadmium and reduced copper inside a reduction column. The two resolved peaks were then mixed with Griess reagent (dinitrogen trioxide, N2O3, generated from acidified nitrite that reacts with sulfanilamide) in-line to form the classical diazo compound that was then detected spectrophotometrically. Triplicate determinations were performed on each specimen and the final values averaged.
AKI definition.
Patients were classified by the validated pediatric Risk, Injury, Failure, Loss of function, End-stage renal disease (pRIFLE) criteria per which AKI outcome can be categorized as Risk, Injury, Failure, Loss of function, or End-stage renal disease using the changes in estimated creatinine clearance (eCCl) from baseline eCCl (4,11). Briefly, the pRIFLE criteria grade AKI severity into pRIFLE-R (Risk; 25–50% change in eCCl), pRIFLE-I (Injury; 50–75% change), and pRIFLE-F (Failure; >75% change). Baseline kidney function was defined as the lowest known SCr value in the previous 3 months. The minimal diagnostic criterion for AKI was a 25% decrease in eCCl. Patients with no known prior SCr were assumed to have normal baseline renal function and assigned a baseline eCCl of 120 mL/min/1.73 m2. This cut-off was chosen because the Schwartz eCCl is known to overestimate GFR and we have previously validated this cut-off as the most accurate method when back calculating in patients with known baseline creatinine values (15).
Data analysis.
SPSS version 18 (SPSS Inc., Chicago, IL) was used to perform the statistical analysis. Patient demographic characteristics were described using frequencies for categorical variables and measures of central tendency and dispersion for continuous variables. Distributions were explored for absolute urinary nitrate and nitrite as well as after normalization to urinary creatinine; all were found to be non-Gaussian in distribution. Therefore, these measures were described using medians and compared using nonparametric methods (Kruskal-Wallis test for multiple groups and Mann-Whitney U test for two groups). We compared median urinary nitrite and nitrate concentrations across AKI severity categorized by pRIFLE strata: 1) no AKI, pRIFLE-R, and pRIFLE-I and 2) no AKI and pRIFLE-R combined and pRIFLE-I. The diagnostic accuracy of normalized urinary nitrate was evaluated using receiver operator characteristic (ROC) techniques.
RESULTS
Demographics and clinical follow-up data.
Two hundred fifty-two patients who met inclusion criteria were enrolled in the study. Median age was 12 y (range 0–19 y), 50% male, 38% white, 31% Hispanic, 24% black, and 4% Asian. We observed a high hospitalization rate of 56% (142 patients), likely because enrollment was restricted to patients who had a SCr assessed. The median hospital length of stay was 3 d (range 1–39 d). Only three patients were admitted to the ICU during hospitalization.
AKI results.
The primary diagnostic categories for all the patients enrolled in the study showed a high prevalence of diabetic ketoacidosis (32%); gastrointestinal and infectious disease-related diagnoses were also commonly represented (14% each). Eighteen of the total 252 patient cohort (7.1%) had AKI as defined by pRIFLE; 12 (5%) had pRIFLE-R and 6 (2%) had pRIFLE-I. There were miscellaneous primary diagnoses and organ systems involved in the 18 patients with AKI: type 1 diabetes mellitus was the commonest (17%).
Fifteen of the admitted patients (11%) had AKI; 10 (7%) had pRIFLE-R; and 5 (4%) had pRIFLE-I. No patient had or developed pRIFLE-F. The mean SCr was 0.6 ± 0.26 mg/dL (range 0.2–2.2 mg/dL) and mean eCCl was 154 ± 40 mL/min/1.73m2 (range 45–315 mL/min/1.73m2). Sixty patients (24%) had a baseline SCr within the 3 months before the ED visit. Demographic data did not differ between patients with versus without known SCr within the 3 months before the ED visit.
While the mean SCr was higher and corresponding mean eCCl lower, for patients with AKI, nine of the AKI patients had SCr <1 mg/dL and six had eCCl >90 mL/min/1.73m2 in the ED. Thus, 33–50% of the patients with AKI calculated by pRIFLE may not have had AKI identified by the SCr value alone at the time of ED visit.
The rate of AKI detection by pRIFLE was higher in patients with versus patients without a known baseline SCr (8.7 versus 4.9%, p < 0.03). Fifty-four (38%) of the hospitalized patients had a subsequent SCr measured as part of the course of their clinical care, none of whom developed new onset or worsening AKI.
Urinary nitrite and nitrate results.
We compared urinary biomarker concentrations for the entire 252 patient cohort across AKI severity by pRIFLE strata. Figure 1 shows absolute median urinary nitrate values in the three groups; there was a significant decline in urinary nitrate in pRIFLE-I versus pRIFLE-R or the no AKI groups (p = 0.033 by Kruskal-Wallis test). Table 1 lists the results for the controls (no AKI) and AKI patients (pRIFLE-R and pRIFLE-I) as absolute values of nitrite and nitrate (μM) and normalized to urinary creatinine (μg/mg Cr). Using the Kruskal-Wallis test, urinary nitrate normalized to creatinine was significantly lower in pRIFLE-I versus pRIFLE-R or the no AKI groups (p = 0.036). A separate analysis of urinary biomarker levels revealed absolute median urinary nitrate to be significantly lower for the injury group (pRIFLE-I) compared with the combined risk (pRIFLE-R) and no AKI groups (p = 0.012; Table 2). Urinary nitrate normalized to creatinine was also significantly lower (712 μg/mg Cr in the combined group versus 389 μg/mg Cr in pRIFLE-I; p = 0.020). Urinary nitrite failed to show any significant differences between the AKI versus no AKI groups.
Absolute median urinary nitrate concentrations in patients presenting to TCH-ED with no AKI, at risk for AKI (pRIFLE-R), and those with injury (pRIFLE-I; n = 252 patients). Data are shown as box plots with the heavy line in the box representing the median (50th percentile) and the ends of the box representing 25th and 75th percentiles, respectively. Groups were compared using the nonparametric Kruskal-Wallis test *(p = 0.03). TCH, TX Children's Hospital.
Urinary biomarker diagnostic characteristics.
Figure 2 shows the ROC curve to predict the sensitivity and specificity of urinary nitrate for AKI and to predict the presence of pRIFLE-I. Diagnostic accuracy using ROC curve analysis of urinary nitrate demonstrated good accuracy, area under curve [(AUC) 0.778; 95% CI 0.642–0.914] to predict patients with pRIFLE-I versus patients with pRIFLE-R or without AKI. Maximizing both sensitivity and specificity, the best cut point for the identification of pRIFLE-I was a normalized nitrate ≤410 μg/mg Cr with sensitivity 66.6% and specificity 80.9%.
DISCUSSION
Data from our study provide the first evidence that urinary nitrate, a metabolite of NO, is associated with early AKI in the pediatric ED setting. This is at a time when baseline kidney function, as reflected by SCr, is normal, unchanged, or most often, unavailable. An important aspect of our study was that the majority of patients (75%) did not have a SCr available in the 3 months before the ED visit. This highlights the potential utility of a urinary biomarker to detect acute illness in the setting of unknown baseline kidney function. Nitrate is the predominant urinary NO-based metabolite, whereas nitrite is low to undetectable in urine (16). Hence, it is not surprising why nitrate and not nitrite was the more informative of the two.
Our findings are supported by the study by Kwon et al. (13) which showed diminished excretion of urinary NO metabolites in postischemic AKI, albeit the study was done in adult recipients of cadaveric renal allografts. Ischemia is the most common cause of AKI in both native and transplanted kidneys, with cardiac arrest, sepsis, and shock exposing the kidney to ischemic injury (13). Recent findings have suggested that endothelial injury acts as a primary event leading to renal hypoxia with disturbances in NO pathways playing a major role (12). Studies have suggested that these metabolites may be useful markers of endogenous NO synthase activity (17). Thus, diminished urinary nitrate in patients with early AKI may reflect diminished endothelial production of NO and suggests targeting the NO pathway as a means to treat or prevent the development of AKI.
The morbidity we observed was far less severe; no patients required dialysis; only three patients required ICU admission and we did not observe any patient mortality. However, given that urinary nitrate was lower in patients with pRIFLE-I, we speculate that this biomarker may detect AKI presence and severity in more severely ill children, similar to what was observed for a different set of urinary biomarkers, including NGAL, in a previous study of critically ill children (18,19). However, larger numbers of patients need to be enrolled in more prospective studies to confirm that urinary nitrate can predict severe outcome in children.
We attempted to distinguish sepsis or ischemic causes from the rest, but lack of clear-cut diagnostic categories such as the above and the small number of cases for pRIFLE-I (n = 6) precluded adequate statistical comparison. As hydration status was readily available, we compared urinary biomarkers between patients with and without dehydration; no significant difference was obtained for the biomarkers NGAL and nitrate (data not shown). Nitrate being a relatively novel urinary biomarker prompted us to internally validate it for AKI. Using the cutoff points from the ROC curves for the values that corresponded to the highest diagnostic accuracy, the correlation between the urinary nitrate and NGAL was 0.32. Specifically, of the six patients with renal injury, five would be correctly identified by NGAL and four by nitrate. Three would overlap and all identify the injury.
Our study had limitations. We only had a single measurement of urinary NO metabolites during the ED admission and are thus unable to conclusively correlate changes in markers with subsequent changes in renal function in hospitalized patients. The number of patients with AKI in the ED was relatively small compared with adult studies. However, our study represents the largest single group of children with AKI in the ED from whom urinary NO metabolites have been assessed. We also did not observe any patients with pRIFLE-F (Failure). Because 96% of the filtered nitrite and nitrate is reabsorbed in the renal tubules (20), we speculate that pRIFLE-F may be associated with an increase in urinary NO metabolites due to reduced reabsorption. Enrolling sicker patients will also enable us to assess if urinary NO metabolites are associated with important patient outcome parameters such as the need for ICU admission, renal replacement therapy, hospital length of stay, or patient mortality.
Plasma and urinary levels of nitrate are extremely variable in the individual and between individuals, mainly due to the impact of dietary NOx and endogenous formation of NO (16). Thus, human plasma and urinary nitrate measurements are recommended only after a low NOx diet for at least 4 d (16). However, given the rapid clinical setting of the ED, ensuring a low dietary NOx state in the patient before collection of specimens would be exceedingly hard. Furthermore, our results indicated an effect on urinary nitrate that was opposite to what one would predict given high levels of dietary nitrate, and thus this may be a valid tool in the ED setting. We did not confirm return of the low urinary nitrate excretion to normal after recovery in patients with pRIFLE-I because our study was not designed to collect follow-up urinary specimens. Future prospective study would be needed to elucidate this important aspect because NO production is low in chronic kidney disease and the low urinary nitrate excretion could reflect chronic rather than acute kidney disease.
We are aware of overlap between the groups and the difficulty that arises with a biomarker that is potentially diagnostic when the concentration is low. Our study was not powered to determine the diagnostic accuracy of urinary nitrate, and that coupled with the small number of patients with pRIFLE-I likely explains the high steps on the ROC curve in Figure 2. Our study was not designed to collect and bank extra blood specimens for plasma AKI biomarkers, and thus we could not attempt correlations between plasma NOx and urinary NOx. Plasma NOx would have enabled us to determine the fractional excretion of urinary NO metabolites, potentially a more informative parameter. Ongoing studies will address all the above issues.
In conclusion, our study indicates that in the pediatric ED, decreased urinary nitrate, as a proxy for NO, may be an early biomarker for acute AKI. Given the low prevalence of AKI in our patient group in the ED, it is not prudent to speculate that in all the AKI detected there was an ischemic component given the association with low urinary nitrate. Prospective cohort studies with larger numbers and of more severely ill AKI patients will be required to truly ascertain if urinary nitrate levels obtained in the ED setting can serve well to predict important in-patient clinical outcomes. These studies will enable us to (1) control for potential confounders such as dietary NOx and (2) obtain plasma NOx to determine correlations with urinary NOx in pediatric AKI. Finally, additional work is required to determine whether diminished urinary nitrate in AKI is truly indicative of renal endothelial dysfunction.
Abbreviations
- AKI:
-
acute kidney injury
- eCCl:
-
estimated creatinine clearance
- ED:
-
emergency department
- NGAL:
-
neutrophil gelatinase-associated lipocalin
- NOx:
-
combined nitrite and nitrate concentration
- pRIFLE:
-
AKI outcome as measured by the pediatric RIFLE criteria: risk, injury, failure, loss of function, end-stage renal disease
- pRIFLE-I:
-
injury
- pRIFLE-R:
-
risk
- prifle-f:
-
failure
- ROC:
-
receiver operator characteristic
- SCr:
-
serum creatinine
References
Lameire N, Van Biesen W, Vanholder R 2005 Acute renal failure. Lancet 365: 417–430
Devarajan P 2006 Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol 17: 1503–1520
Devarajan P 2007 Emerging biomarkers of acute kidney injury. Contrib Nephrol 156: 203–212
Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL 2007 Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int 71: 1028–1035
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P 2004 Acute renal failure- definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8: R204–R212
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A, Acute Kidney Injury Network 2007 Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11: R31
Nickolas TL, O'Rourke MJ, Yang J, Sise ME, Canetta PA, Barasch N, Buchen C, Khan F, Mori K, Giglio J, Devarajan P, Barasch J 2008 Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase-associated lipocalin for diagnosing acute kidney injury. Ann Intern Med 148: 810–819
Shapiro NI, Trzeciak S, Hollander JE, Birkhahn R, Otero R, Osborn TM, Moretti E, Nguyen HB, Gunnerson K, Milzman D, Gaieski DF, Goyal M, Cairns CB, Kupfer K, Lee SW, Rivers EP 2010 The diagnostic accuracy of plasma neutrophil gelatinase-associated lipocalin in the prediction of acute kidney injury in emergency department patients with suspected sepsis. Ann Emerg Med 56: 52–59.e1
Di Grande A, Giuffrida C, Carpinteri G, Narbone G, Pirrone G, Di Mauro A, Calandra S, Noto P, Le Moli C, Alongi B, Nigro F 2009 Neutrophil gelatinase-associated lipocalin: a novel biomarker for the early diagnosis of acute kidney injury in the emergency department. Eur Rev Med Pharmacol Sci 13: 197–200
Self WH, Barrett TW 2010 Novel biomarkers: help or hindrance to patient care in the emergency department?. Ann Emerg Med 56: 60–61
Du Y, Zappitelli M, Mian A, Bennett M, Ma Q, Devarajan P, Mehta R, Goldstein SL 2011 Urinary biomarkers to detect acute kidney injury in the pediatric emergency center. Pediatr Nephrol 26: 267–274
Goligorsky MS, Brodsky SV, Noiri E 2002 Nitric oxide in acute renal failure: NOS versus NOS. Kidney Int 61: 855–861
Kwon O, Hong SM, Ramesh G 2009 Diminished NO generation by injured endothelium and loss of macula densa nNOS may contribute to sustained acute kidney injury after ischemia-reperfusion. Am J Physiol Renal Physiol 296: F25–F33
Bryan NS, Grisham MB 2007 Methods to detect nitric oxide and its metabolites in biological samples. Free Radic Biol Med 43: 645–657
Zappitelli M, Parikh CR, Akcan-Arikan A, Washburn KK, Moffett BS, Goldstein SL 2008 Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin J Am Soc Nephrol 3: 948–954
Kelm M 1999 Nitric oxide metabolism and breakdown. Biochim Biophys Acta 1411: 273–289
Elli M, Soylemezoglu O, Erbas D, Bakkaloglu SA, Buyan N, Ozkaya O, Hasanoglu E 2005 Plasma and urine nitric oxide levels in healthy Turkish children. Pediatr Nephrol 20: 1605–1609
Zappitelli M, Washburn KK, Arikan AA, Loftis L, Ma Q, Devarajan P, Parikh CR, Goldstein SL 2007 Urine neutrophil gelatinase-associated lipocalin is an early marker of acute kidney injury in critically ill children: a prospective cohort study. Crit Care 11: R84
Washburn KK, Zappitelli M, Arikan AA, Loftis L, Yalavarthy R, Parikh CR, Edelstein CL, Goldstein SL 2008 Urinary interleukin-18 is an acute kidney injury biomarker in critically ill children. Nephrol Dial Transplant 23: 566–572
Rahma M, Kimura S, Yoneyama H, Kosaka H, Nishiyama A, Fukui T, Abe Y 2001 Effects of furosemide on the tubular reabsorption of nitrates in anesthetized dogs. Eur J Pharmacol 428: 113–119
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Thrasher Research Fund for the Early Career Award (NR-0058) [A.I.M.].
Rights and permissions
About this article
Cite this article
Mian, A., Du, Y., Garg, H. et al. Urinary Nitrate Might Be an Early Biomarker for Pediatric Acute Kidney Injury in the Emergency Department. Pediatr Res 70, 203–207 (2011). https://doi.org/10.1203/PDR.0b013e31822188b4
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31822188b4
This article is cited by
-
Renal Nitric Oxide Deficiency and Chronic Kidney Disease in Young Sheep Born with a Solitary Functioning Kidney
Scientific Reports (2016)
-
Towards a biomarker panel for the assessment of AKI in children receiving intensive care
Pediatric Nephrology (2015)