Abstract
Severe malnutrition is a major health problem in developing countries and can present itself as kwashiorkor or marasmus. Although marasmus is characterized by clinical wasting, kwashiorkor is associated with peripheral edema, oxidative stress, hypoalbuminemia, and hypoglycemia. The etiology of the hypoglycemia is poorly understood. We determined endogenous glucose production (EGP) in children with severe malnutrition. Children with kwashiorkor, marasmus, and controls received a primed constant infusion of [6,6H2]glucose for 2 h. An i.v. bolus of 13C-ketoisocaproic acid (KIC) was given, and breath samples were obtained during 2 h. Isotope dilution was used to calculate EGP, and 13CO2/12CO2 production was determined. Mean EGP ± SEM was 5.5 ± 0.3 mg/kg/min in the kwashiorkor group and 6.9 ± 0.4 mg/kg/min and 7.6 ± 0.7 mg/kg/min in the marasmic and control group, respectively, (p < 0.05 kwashiorkor versus marasmus and controls). EGP correlated with serum albumin concentration (r = 0.67; p < 0.001) and urinary 8-hydroxydeoxyguanosine as a marker of oxidative stress (r = −0.62; p < 0.005). 13CO2 secretion as a marker of hepatic mitochondrial function was significantly higher in the marasmic group compared with kwashiorkor and controls. We conclude that decreased EGP in severely malnourished children is related to the degree of hypoalbuminemia and oxidative stress but is not associated with a clear defect in hepatic mitochondrial function.
Similar content being viewed by others
Main
Severe malnutrition presenting as kwashiorkor or marasmus is still a significant health problem in developing countries (1,2). The HIV/AIDS epidemic has increased case fatality rates of severe malnutrition, and these children often have comorbidities caused by opportunistic infections (3). Despite the high incidence and severity of severe malnutrition, basic pathophysiological differences between kwashiorkor and marasmus are poorly understood. Although it was historically postulated that kwashiorkor was caused by a protein deficiency and marasmus by a calorie deficiency, these hypotheses have been largely abandoned (4). Kwashiorkor is characterized by irritability, hair changes, edema, hepatomegaly, and dyspigmentation. Metabolic features include hypoalbuminemia, hepatic steatosis, and hypoglycemia (5–7). Marasmus is characterized by severe wasting (low weight for height) without edema.
Hypoglycemia is a common phenomenon in kwashiorkor (5,8,9), although it is also described in patients with severe wasting (8). Theoretically, hypoglycemia could be caused by impaired hepatic endogenous glucose production (EGP) or increased glucose clearance. A small study in five children with malnutrition indicated normal glucose production (10), although data from a kwashiorkor animal model suggested impaired EGP (11).
Kwashiorkor has been firmly linked to hepatic steatosis and oxidative stress. The oxidative stress has been thought to be triggered by infections, decreased antioxidant status, or toxins (12–14). Patients with hepatic steatosis in the context of obesity and insulin resistance also demonstrate increased oxidative stress (15). Although kwashiorkor is related to a state of nutritional deficiency in contrast to obesity-related steatosis, surplus tissue fatty acids have been shown to stimulate oxidative stress, leading to mitochondrial damage and cell death irrespective of its cause (16,17). Steatosis can lead to impairment of mitochondrial function (18) and ATP production (19). Decreased hepatic glucose production rates as found in inborn errors of metabolism in the oxidative phosphorylation pathway (20) or animal models of shock indicate a close link between mitochondrial dysfunction and impaired gluconeogenesis (21). Finally, signs of hepatic failure have been described in patients with severe malnutrition (22), which would also be associated with decreased EGP.
Breath tests using stable isotopes have been used to determine various biochemical functions. Ketoisocaproic acid (KIC, a branched-chain amino acid) can undergo decarboxylation through a branched-chain α-ketoacid dehydrogenase complex, which is located exclusively in mitochondria. The enzyme complex has been shown to be primarily active in hepatic mitochondria (23). KIC decarboxylation activity assessed by 13C-KIC breath tests have been used to detect hepatic mitochondrial dysfunction in humans (24–26).
In this study, we aimed to address the underlying etiology of hypoglycemia in kwashiorkor. We hypothesized that kwashiorkor was associated with decreased EGP and KIC decarboxylation activity. EGP and KIC decarboxylation were assessed in severely malnourished and healthy children. Levels of oxidative stress, gluconeogenic precursors, and hormonal changes were also characterized.
METHODS
Subjects.
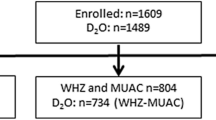
The study was conducted in severely malnourished children and control subjects admitted to MOYO House (a Nutrition Rehabilitation Unit) or one of the pediatric wards of the Queen Elizabeth Central Hospital (QECH) in Malawi. Children with kwashiorkor and marasmus were admitted as recommended by the WHO (27). Sample size was calculated to be seven per group, expecting a difference of EGP between kwashiorkor and the other groups of 20%, a power of 80%, and α of 0.05. We choose to recruit additional children to account for potential loss of sample or technical difficulties. Information about the study was provided verbally and through a detailed written information sheet. Informed consent was obtained from parents of all participants in accordance with the College of Medicine, University of Malawi, Ethical Committee guidelines. Kwashiorkor was defined as edema, not related to cardiac or renal disease and dyspigmentation of skin or hair. Marasmus was defined as a weight/age ratio <70%, i.e. >3 SDs below the mean of the WHO reference population. Children with and without HIV infection were included. Exclusion criteria were malaria, clear signs of sepsis, i.e. respiratory distress or circulatory failure, signs of pneumonia, Hb <8 mg/dL, and neurological symptoms of convulsions or decreased mental status. Malaria was excluded by blood film analysis. The use of antiretroviral therapy was an additional exclusion criterion. Control subjects were children admitted for a minor orthopedic problem, or children who had fully recovered from an intercurrent viral or bacterial respiratory infection and were included at the time of discharge. Additional exclusion criteria for this group were fever or auscultatory abnormalities at the time of the study. All malnourished children were admitted and treated according to a standard WHO protocol (27). Children were started on a liquid diet (F75), every 2 h to a total of 75 kcal energy/kg/d. With F75, energy obtained from fat is 32%, protein 5%, and the remaining percentage from carbohydrates.
Experimental protocol.
Children with malnutrition were studied as soon as possible after admission but at least within 4 d after admission. The control subjects were, except for one child, studied within 5 d after admission. The afternoon before the study, a peripheral i.v. access was placed in an antebrachial vein. From midnight onward, patients and control subjects were fasted, and a glucose infusion (2 mg/kg/min) was given to all subjects until ∼30 min before start of the isotope infusion to prevent hypoglycemia. Glucose concentrations were checked when clinically indicated. A baseline blood sample just before start of the isotope infusion was obtained. At 0800 h, a second peripheral venous access was established and a primed (13 mg/kg in 10 mL aqueous solution), constant infusion (0.15 mg/kg/min) of [6,6-H2]-glucose was given over 2 h. Blood spots (50 μL) were obtained at t = 0, 90, and 120 min for glucose concentration and collection on filter paper. Subsequently, children resumed their specific diets until midnight when the fasting protocol was repeated. On d 2, an i.v. bolus of 1 mg/kg [1-13C]ketoisocaproate, together with an i.v. bolus of 20 mg/kg leucine, was given at t = 0 (0800 h), and breath samples were obtained at t = 0, 10, 15, 20, 30, 60, 90, and 120 min. The leucine is administered to prevent reamination of the administered [1-13C]ketoisocaproate back to leucine (28). Breath samples were taken by allowing children to breath into a mask sealed to the face to which a collection bag was attached. Room air could not enter because of a unidirectional valve system. Urine was collected using collection bags during the study for a period of ∼5 h.
Biochemical analyses.
All blood analyses were determined in the sample after the overnight fast on d 1. Analyses for basic biochemistry were performed using routine methods. Plasma β-hydroxybutyrate and FFA concentrations were determined using commercially available kits (Roche Diagnostics, Mannheim, Germany and Wako Chemicals GmbH, Neuss, Germany). Amino acid analysis was performed according to Moore et al., (29), based on liquid chromatography and postcolumn derivatization using ninhydrin. Amino acid concentrations were measured using a Biochrom 20 amino acid analyzer (Biochrom Ltd., Cambridge, UK). Determination of insulin and glucagon concentrations was performed using enzyme immunoassays (EIA; Diagnostic Systems Laboratories, Sinsheim, Germany). Intra- and interassay coefficient of variation were <3% and <7% for insulin and <5% and 19% for glucagon, respectively. Cortisol and growth hormone concentrations were determined using EIA (ALPCO Diagnostics, Salem, NH) with a intra- and interassay coefficient of variation of <10% and <9% for cortisol and <3% for growth hormone. Urinary 8-hydroxydeoxyguanosine (8-OhdG) was determined using an ELISA (Northwest, Vancouver, Canada) and corrected for creatinine excretion. Intra- and interassay coefficient of variation were <3% and <8%, respectively.
Stable isotope analyses.
All the breath test measurements were performed by gas isotope-ratio mass spectrometry (Delta Plus, Thermo Electron, Bremen, Germany). The CO2 pulse was separated from other gas components in breath and then ionized and separated in the mass spectrometer into 12CO2 (m/z 44) and 13CO2 (m/z 45) ions. Measured values were expressed as δ13C versus PeeDeeBelemnite limestone (30). For the glucose analyses, a disk (6.5 mm in diameter) was punched out of a blood spot, wetted with 40 μL water and 400 μL ethanol, and shaken for 45 min at room temperature. The supernatant after centrifugation was dried at 60°C under a stream of N2. Glucose was converted to its pentaacetate derivative by adding 150 μL pyridine/acetic anhydride (1:2) and incubation for 30 min at 60°C, followed by drying at 60°C. The residue was dissolved in ethylacetate. All samples were analyzed by gas chromatography quadrupole mass spectrometry (SSQ7000; ThermoFinnigan, San Jose, CA). For all calculations of mass isotopomer distribution, Excaliber software (ThermoFinnigan) was used. Derivatives were separated on an AT-5MS 30 m × 0.25 mm ID (0.25-μm film thickness) capillary column (Alltech, Breda, the Netherlands). The gas chromatography oven temperature was started at 80°C for 1 min, increased to 280°C at a rate of 20°C for 1 min after which the oven was held at 280°C for 3 min. Mass spectrometric analyses were performed by positive ion chemical ionization with methane. Ions monitored for glucose pentaacetate were m/z 331–333, corresponding to the m0–m2 mass isotopomers.
Calculations.
The whole-body blood glucose production rate [Ra(glc; whole body)] was calculated as follows: Ra(glc;whole body) = M2infusate/M2blood × infusion(glc,M2), where total Ra glucose is the total rate of appearance of glucose and [glc] is the glucose concentration just before start of the stable isotope infusion. The rate of EGP was calculated as follows: Ra(glc;endogenous) = Ra(glc;whole body) − Ra(glc;exogenous), and in this study, Ra(glc;exogenous) was minimal. For the children with kwashiorkor, weight used for calculations of EGP and rate of exhalation of 13CO2 was the lowest weight at the time of complete clinical loss of edema, hence approaching normalized gross body composition. The calculations of mitochondrial KIC decarboxylation activity were as follows. The rate of exhalation of 13CO2 at each time point was calculated from the measured increment in the isotopic abundance of 13CO2 (δ13CPDB), the known purity of the labeled compound and an assumed constant endogenous production of CO2 (400 mmol/m2/h). The cumulative recovery of 13CO2 in breath was calculated as the area under the curve of the 13CO2 exhalation rate compared with the time curve determined by linear interpolation. Results were expressed as the percentage of the administered dose exhaled.
Statistical analysis.
The data were analyzed by using SPSS software version 16.0 (SPSS Inc, Chicago, IL). All values are represented as the mean ± SEM. One-way ANOVA with Tukey post hoc analysis was used for statistical comparison of study groups. Correlation analyses were performed using Pearson's rank correlation. Differences were considered significant at p < 0.05.
RESULTS
Basic patient characteristics.
There was a trend for the mean age to be lower in marasmic children and control subjects compared to children with kwashiorkor, but this difference was nonsignificant (Table 1). Weight and midupper arm circumference (MUAC) were lower (p < 0.05) in children with marasmus compared with kwashiorkor and controls. Forty-four percent of children with kwashiorkor and 36% of children with marasmus were HIV positive. Glucose concentrations before the start of the isotope infusion did not differ between groups. Alanine aminotransferase (ALT) levels were elevated (40 U/L) in 56% and 55% of children with kwashiorkor and marasmus, respectively. There were no electrolyte abnormalities in any of the children at the time of the study (data not shown). Children were followed clinically after the study until discharge or death. Mortality after the study was 25% in the malnourished children, whereas none of the controls died. Three children developed severe diarrhea after the study and then they were given a high caloric nutritional supplement [ready-to use therapeutic foods (RUTF)], possibly related to osmotic diarrhea. They likely died of acute severe dehydration. One child developed circulatory insufficiency after the study. One child was found dead a couple of days after the study, potentially related to hypoglycemia.
Endogenous glucose production.
We calculated rates of EGP in the different groups as shown in Figure 1. Glucose concentrations and calculated EGP at the 90 and 120 min time points were similar, indicating a steady state. EGP was calculated using the average of the two time points. EGP was lower in children with kwashiorkor (5.5 ± 0.3 mg/kg/min) compared with marasmus (6.9 ± 0.4 mg/kg/min) or controls (7.6 ± 0.7 mg/kg/min; p < 0.05). Regardless of the clinical classification, there was a correlation between serum albumin concentrations and EGP (Fig. 2). Rates of EGP were comparable between HIV infected (6.5 ± 0.4 mg/kg/min) and noninfected (6.1 ± 0.4 mg/kg/min) malnourished children, which was not altered after further stratification into children with kwashiorkor and marasmus (data not shown). There was no correlation between age and EGP in our study (r = −0.08; p = 0.7).
KIC decarboxylation.
We next determined KIC decarboxylation in children with severe malnutrition and controls. Figure 3A shows the maximum percentage of 13CO2 recovery per hour, and Figure 3B shows the cumulative percentage of 13CO2 recovery in study subjects. Both maximum and cumulative 13CO2 recovery were lower in control subjects compared with marasmic children (p < 0.05 for cumulative and p < 0.01 for maximum recovery) or those with kwashiorkor (p < 0.05). There was a significant correlation between EGP and cumulative 13CO2 recovery for all malnutrition groups combined (r = 0.48; p < 0.05; Fig. 4). Cumulative 13CO2 recovery was similar in HIV positive and negative malnourished children (data not shown).
Hormones and gluconeogenic precursors.
EGP is controlled by different hormones and can be limited by gluconeogenic precursor availability. Therefore, we determined relevant hormone concentrations and gluconeogenic precursor concentrations that are shown in Table 2. Pyruvate, lactate concentrations, and concentrations of the most abundant amino acids were similar across all groups, indicating no limited precursor availability. Insulin, cortisol, and growth hormone concentrations did not differ between groups although glucagon concentrations were lower in the children with kwashiorkor and controls compared with marasmic children (p < 0.005 and p < 0.05, respectively).
Oxidative stress markers.
Urinary 8-OhdG concentrations were 5.3 ± 0.8, 4.1 ± 1.2, and 1.9 ± 0.7 ng/mmol creatinine in children with kwashiorkor, marasmus, and controls, respectively (p < 0.05 kwashiorkor versus controls; p = 0.08 marasmus versus controls). There was a significant inverse correlation between the urinary 8-OhdG, corrected for creatinine excretion, and EGP (Fig. 5; r = −0.62; p < 0.005).
DISCUSSION
Severe malnutrition is a condition that is still widespread in low resource settings. Despite management practices following WHO guidelines, case fatality rates of 10% are reported in HIV noninfected children and between 30% and 40% in HIV infected children (3,27), similar to what was found in our study. High case fatality rates, irrespective of their HIV status, are associated with septicaemia, compromised reductive adaptation, (31) and hypoglycemia/hypothermia. Hypoglycemia could relate to decreased glucose absorption, hepatic glucose production, or increased glucose clearance. To our knowledge, this is the first study to examine EGP in children with kwashiorkor and marasmus.
A fine balance between EGP and glucose clearance maintains blood glucose concentrations. Young children have a limited capacity for fasting and generally develop hypoglycemia after 24 h because of insufficient glucose production (32,33). There are scarce data on EGP in young children. A recent study in young children (1–5 y) with malaria showed rates of EGP were similar to those observed in this study (34). Lower EGP could be caused by a decrease in glycogenolysis or gluconeogenesis. Glycogen content has been found to be high (35), low (36), or normal (5) in biopsies from children with kwashiorkor. In this study, the overnight fast, despite a small glucose infusion, would probably have depleted glycogen stores and differences in EGP are, therefore, more likely related to alterations in gluconeogenesis than glycogenolysis.
13C-KIC breath tests have been used extensively to detect hepatic mitochondrial dysfunction in humans with various hepatic insults including steatosis/steatohepatitis (24–26). For this study, it was chosen to give the KIC i.v. to eliminate effects because of the differences in intestinal absorption of KIC. Substantial difference in total CO2 production would influence breath test results. To minimize the variation in total CO2 production, all subjects were studied while abstaining from any physical exercise. Furthermore, signs of respiratory distress or septicaemia were exclusion criteria. Although differences in total CO2 production could not be excluded, we feel they would not substantially influence the findings. Higher KIC decarboxylation activity was found in all malnourished children compared with controls. These differences probably reflect a catabolic state in the malnourished children and an anabolic state in controls and indicate that malnourished children have a capability to increase KIC decarboxylation. Therefore, these data do not suggest gross hepatic mitochondrial dysfunction in these children. Interestingly, there was a significant correlation between KIC decarboxylation activity and EGP in children with severe malnutrition, and there was a trend toward lower decarboxylation activity in the kwashiorkor compared with marasmic group. It is tempting to speculate that this would be caused by a relative impairment in mitochondrial activity. The lower KIC decarboxylation in children with severe kwashiorkor is consistent with other data. KIC is formed from leucine, and the flux of leucine has been reported to be lower in children with kwashiorkor than in marasmus (37).
Studies on prolonged fasting in young children suggested a deficiency in amino acids used for gluconeogenesis (32). Concentrations of the most abundant amino acids did not differ significantly in our study, nor was there a correlation between total amino acid concentration and EGP (data not shown). Therefore, these results do not support a role for low precursor availability causing decreased EGP in kwashiorkor. Growth hormone concentration in a previous study was generally higher in children with kwashiorkor (38). Cortisol stress response has not been shown to be impaired in severe malnutrition (39). Plasma glucagon concentrations have been reported relatively low in severe kwashiorkor (5), and plasma glucose concentrations have been shown to respond to glucagon injection (40). In this study, glucagon concentrations were lower in children with kwashiorkor compared with marasmus but similar to control children. Specific fasting studies are needed to conclusively determine whether there is a defect in the glucagon response in children with kwashiorkor.
A number of children diagnosed by the admitting doctor on admission as marasmus, with no or minimal edema, were found to be hypoalbuminemic. These children had no clear additional features of kwashiorkor (hair discoloration and skin lesions). However, our data indicate that metabolically they resembled children with kwashiorkor. This supports the notion that hypoalbuminemia indicates a severe derangement in the child's metabolic system, reflecting a disturbance in protein metabolism (37,41), potentially cytokine-mediated inhibition of albumin synthesis (42), or, alternatively, cytokine-mediated capillary leak and redistribution of albumin to the extravascular space. Kwashiorkor is associated with increased oxidative stress (12,13). The significant correlation between levels of 8-OHdG, a cellular oxidative stress marker, albumin, and EGP further underscores the severity of the insult to hepatic metabolism in, especially hypoalbuminemic, malnourished children. We also performed multiple linear regression analyses to further investigate these correlations and found the standardized coefficient to be 0.45 for albumin (p = 0.05) and −0.46 (p = 0.05) for 8-OHdG. The hepatic insult was further illustrated by increased transaminase concentrations in these children, which have been documented previously (43). As hepatic steatosis is closely linked to the development of hepatic inflammation, this could play a role in the etiology of hepatic damage in severe malnutrition.
A limitation of this study was that EGP could not be examined under completely fasted conditions nor during hypoglycemia because of the ethical constraints. However, the children received a very limited glucose infusion compared with total glucose turnover that was stopped before the study. Therefore, we feel that this would have little impact on the results of this study. An additional limitation is the relatively small sample size, in particular for the control group, related to a very challenging recruitment. In addition, there was a substantial secondary exclusion because of the loss of i.v. access during the study and inability to replace the i.v. line. These secondary exclusions might have favored inclusion of children with less complicated malnutrition. Exclusion criteria of sepsis or respiratory distress and the inability to obtain i.v. access in the most edematous children also led to inclusion of less sick patients and could have biased the results in favor of less impaired glucose kinetics. Because the additional fluid as edema in the children with kwashiorkor was not considered to be metabolically active, we decided that we would use the weight at the time of complete disappearance of the edema for our isotope calculations. Using the measured body weight at the time of the study would have underestimated calculated EGP rates and 13CO2 exhalation rates. Furthermore, marasmus specifically is characterized by severe wasting and muscle atrophy. This would have likely led to a lower lean body mass in children with marasmus compared with kwashiorkor, causing an underestimation of the observed differences in EGP.
In conclusion, these results demonstrate decreased EGP in children with kwashiorkor compared with marasmus and healthy children. Differences in EGP were not associated with gross signs of hepatic mitochondrial dysfunction but were related to the degree of hypoalbuminemia and oxidative stress. Clinical criteria alone are insufficient to distinguish the severity of metabolic derangements in children with different forms of severe malnutrition.
Abbreviations
- EGP:
-
endogenous glucose production
- KIC:
-
ketoisocaproic acid
- 8-OhdG:
-
8-hydroxydeoxyguanosine
References
Bejon P, Mohammed S, Mwangi I, Atkinson SH, Osier F, Peshu N, Newton CR, Maitland K, Berkley JA 2008 Fraction of all hospital admissions and deaths attributable to malnutrition among children in rural Kenya. Am J Clin Nutr 88: 1626–1631
Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, Mathers C, Rivera J 2008 Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371: 243–260
Heikens GT, Bunn J, Amadi B, Manary M, Chhagan M, Berkley JA, Rollins N, Kelly P, Adamczick C, Maitland K, Tomkins A 2008 Case management of HIV-infected severely malnourished children: challenges in the area of highest prevalence. Lancet 371: 1305–1307
Golden MH 1998 Oedematous malnutrition. Br Med Bull 54: 433–444
Buchanan N, Moodley G, Eyberg C, Bloom SR, Hansen JD 1976 Hypoglycaemia associated with severe kwashiorkor. S Afr Med J 50: 1442–1446
Williams CD 1933 Kwashiorkor: a nutritional disease of children associated with a maize diet. 1935. Arch Dis Child 8: 423–433
Chanda NK 1958 Pathological study of the liver in kwashiorkor. BMJ 1: 1263–1266
Kerpel-Fronius E, Kaiser E 1967 Hypoglycaemia in infantile malnutrition. Acta Paediatr Scand 56: 119–127
Wharton B 1970 Hypoglycaemia in children with kwashiorkor. Lancet 1: 171–173
Kerr DS, Stevens MC, Picou DI 1978 Fasting metabolism in infants: II. The effect of severe undernutrition and infusion of alanine on glucose production estimated with U-13C-glucose. Metabolism 27: 831–848
Heard CR, Frangi SM, Wright PM, McCartney PR 1977 Biochemical characteristics of different forms of protein-energy malnutrition: an experimental model using young rats. Br J Nutr 37: 1–21
Golden MH, Ramdath D 1987 Free radicals in the pathogenesis of kwashiorkor. Proc Nutr Soc 46: 53–68
Manary MJ, Leeuwenburgh C, Heinecke JW 2000 Increased oxidative stress in kwashiorkor. J Pediatr 137: 421–424
Hendrickse RG 1991 Kwashiorkor: the hypothesis that incriminates aflatoxins. Pediatrics 88: 376–379
Yesilova Z, Yaman H, Oktenli C, Ozcan A, Uygun A, Cakir E, Sanisoglu SY, Erdil A, Ates Y, Aslan M, Musabak U, Erbil MK, Karaeren N, Dagalp K 2005 Systemic markers of lipid peroxidation and antioxidants in patients with nonalcoholic Fatty liver disease. Am J Gastroenterol 100: 850–855
Wei Y, Clark SE, Thyfault JP, Uptergrove GM, Li W, Whaley-Connell AT, Ferrario CM, Sowers JR, Ibdah JA 2009 Oxidative stress-mediated mitochondrial dysfunction contributes to angiotensin II-induced nonalcoholic fatty liver disease in transgenic Ren2 rats. Am J Pathol 174: 1329–1337
Schrauwen P, Hesselink MK 2004 Oxidative capacity, lipotoxicity, and mitochondrial damage in type 2 diabetes. Diabetes 53: 1412–1417
Pérez-Carreras del Hoyo P, Martin MA, Rubio JC, Martin A, Castellano G, Colina F, Arenas J, Solis-Herruzo JA 2003 Defective hepatic mitochondrial respiratory chain in patients with nonalcoholic steatohepatitis. Hepatology 38: 999–1007
Cortez-Pinto H, Chatham J, Chacko VP, Arnold C, Rashid A, Diehl AM 1999 Alterations in liver ATP homeostasis in human nonalcoholic steatohepatitis: a pilot study. JAMA 282: 1659–1664
Mochel F, Slama A, Touati G, Desguerre I, Giurgea I, Rabier D, Brivet M, Rustin P, Saudubray JM, DeLonlay P 2005 Respiratory chain defects may present only with hypoglycemia. J Clin Endocrinol Metab 90: 3780–3785
Rhodes RS, DePalma RG 1980 Mitochondrial dysfunction of the liver and hypoglycemia in hemorrhagic shock. Surg Gynecol Obstet 150: 347–352
McLean AE 1962 Hepatic failure in malnutrition. Lancet 2: 1292–1294
Khatra BS, Chawla RK, Sewell CW, Rudman D 1977 Distribution of branched-chain alpha-keto acid dehydrogenases in primate tissues. J Clin Invest 59: 558–564
Zocco MA, Di Campli C, Gaspari R, Candelli M, Nista EC, Zileri Dal Verme L, Di Gioacchino G, Santoliquido A, Flore R, Tondi P, Proietti R, Pola P, Gasbarrini G, Gasbarrini A 2005 Improvement of mitochondrial function evaluated by ketoisocaproic acid breath test in patients with HCV infection undergoing albumin dialysis. Transplant Proc 37: 2554–2556
Portincasa P, Grattagliano I, Lauterburg BH, Palmieri VO, Palasciano G, Stellaard F 2006 Liver breath tests non-invasively predict higher stages of non-alcoholic steatohepatitis. Clin Sci (Lond) 111: 135–143
Parra D, Gonzalez A, Garcia-Villarreal L, Martinez JA 2003 Methodological characterization of the 2-keto [1–13C]isocaproate breath test to measure in vivo human mitochondrial function: application in alcoholic liver disease assessment. Alcohol Clin Exp Res 27: 1293–1298
World Health Organization 1999 Management of Severe Malnutrition: A Manual for Physicians and Other Senior Health Workers. World Health Organization, Geneva, Switzerland. Available at: http://whqlibdoc.who.int/hq/1999/a57361.pdf. Accessed February 10, 2010
Berthold HK, Giesen TA, Gouni-Berthold I 2009 The stable isotope ketoisocaproic acid breath test as a measure of hepatic decarboxylation capacity: a quantitative analysis in normal subjects after oral and intravenous administration. Liver Int 29: 1356–1364
Moore S, Spackman DH, Stein WH 1958 Chromatography of amino acids on sulfonated polystyrene resins. An improved system. Anal Chem 30: 1185–1190
Stellaard F, Geypens B 1998 European interlaboratory comparison of breath 13CO2 analysis. Gut 43: S2–S6
Heikens GT 2007 How can we improve the care of severely malnourished children in Africa?. PLoS Med 4: e45
Haymond MW, Karl IE, Clarke WL, Pagliara AS, Santiago JV 1982 Differences in circulating gluconeogenic substrates during short-term fasting in men, women, and children. Metabolism 31: 33–42
Chaussain JL, Georges P, Calzada L, Job JC 1977 Glycemic response to 24-hour fast in normal children: III. Influence of age. J Pediatr 91: 711–714
Zijlmans W, van Kempen A, Ackermans M, de Metz J, Kager P, Sauerwein H 2008 Glucose kinetics during fasting in young children with severe and non-severe malaria in Suriname. Am J Trop Med Hyg 79: 605–612
Waterlow JC, Weisz T 1956 The fat, protein and nucleic acid content of the liver in malnourished human infants. J Clin Invest 35: 346–354
Aballi AJ 1950 Disturbances of carbohydrate metabolism in infantile malnutrition. Rev Cubana Pediatr 22: 509–541
Jahoor F, Badaloo A, Reid M, Forrester T 2005 Protein kinetic differences between children with edematous and nonedematous severe childhood undernutrition in the fed and postabsorptive states. Am J Clin Nutr 82: 792–800
Pimstone BL, Barbezat G, Hansen JD, Murray P 1968 Studies on growth hormone secretion in protein-calorie malnutrition. Am J Clin Nutr 21: 482–487
Jaya Rao KS, Srikantia SG, Gopalan C 1968 Plasma cortisol levels in protein-calorie malnutrition. Arch Dis Child 43: 365–367
Kassem AS, Badr-El-Din MK, Hassan A-H, Hafez M 1975 The liver and carbohydrate metabolism in protein calorie malnutrition. J Trop Pediatr Environ Child Health 21: 3–6
Golden MH, Waterlow JC, Picou D 1977 Protein turnover, synthesis and breakdown before and after recovery from protein-energy malnutrition. Clin Sci Mol Med 53: 473–477
Chojkier M 2005 Inhibition of albumin synthesis in chronic diseases: molecular mechanisms. J Clin Gastroenterol 39: S143–S146
Etukudo MH, Agbedana EO, Akinyinka OO, Osifo BO 1999 Plasma electrolytes, total cholesterol, liver enzymes, and selected antioxidant status in protein energy malnutrition. Afr J Med Med Sci 28: 81–85
Acknowledgements
We thank the MOYO nursing team and the Pediatric Research Ward nursing team of the Queen Elizabeth Central Hospital for their excellent clinical support. We thank Pim Modderman and Theo van Dijk for their technical support and James Bunn, Marko Kerac, Elizabeth Molyneux, Paul Pencharz, Annette Feigenbaum, and Patrick van Rheenen for their helpful discussions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by an international fellowship grant from the Nutricia Research Foundation (R.H.J.B.).
Rights and permissions
About this article
Cite this article
Bandsma, R., Mendel, M., Spoelstra, M. et al. Mechanisms Behind Decreased Endogenous Glucose Production in Malnourished Children. Pediatr Res 68, 423–428 (2010). https://doi.org/10.1203/PDR.0b013e3181f2b959
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181f2b959