Abstract
By the end of puberty, growth ceases and epiphyseal fusion occurs through mechanisms not yet completely understood. Human growth plate tissues were collected in various pubertal stages including a unique late pubertal growth plate, which was about to fuse. Apoptosis was studied by TUNEL staining, immunolocalization of pro- and antiapoptotic proteins, and electron microscopy (EM). Morphologic analyses of the fusing growth plate revealed disorganized, large chondrocytes surrounded by a border of dense, cortical-like bone. In the unfused growth plates, few chondrocytes were TUNEL positive. In contrast, the fusing growth plate contained no single TUNEL-positive cell. Antiapoptotic (Bcl-2 and Bcl-XL) and proapoptotic (Bax, Bad, and cleaved caspase-3) proteins were detected in all growth plate zones without change in intensity during pubertal progression. Expression of antiapoptotic proteins was found in the fusing growth plate but of the proapoptotic proteins only Bad was detected. EM revealed no typical signs of apoptosis or autophagy in any of the growth plates. In contrast, morpohological signs of hypoxia and necrosis were observed. We conclude that classical apoptosis is not likely to be involved in the process of human growth plate fusion.
Similar content being viewed by others
Main
Longitudinal growth occurs at the epiphyseal plate, a thin layer of cartilage entrapped between epiphyseal and metaphyseal bone, located at the distal ends of the long bones. The epiphyseal plate consists of three principal layers with immature cells lying toward the epiphysis, called the resting zone, more mature flat chondrocytes in the proliferating zone and the hypertrophic zone adjacent to this. Stem-like cells in the resting zone have a finite proliferative capacity that is gradually exhausted, which consequently results in fusion of the growth plate at the end of puberty (1). At the chondro-osseous junction site of the growth plate, a nowadays generally accepted hypothesis is that terminally hypertrophic chondrocytes die by undergoing apoptosis leaving behind a scaffold of cartilage matrix for osteoblasts that invade and lay down bone resulting in growth plate fusion (1,2). Apoptotic cells in general show typical morphologic changes like cell shrinkage, intact organelles and integrity of membranes, pyknotic nuclei by aggregation of chromatin, fragmented DNA, partitioning of the cytoplasm and nucleus into membrane bound-vesicles (apoptotic bodies), and absence of an inflammatory response (3,4). The Nomenclature Committee on Cell Death suggested to describe apoptosis at a biochemical level as a caspase-dependent process (5).
Apoptosis in growth plate chondrocytes has been reported in many in vivo and in vitro studies performed in different species applying mostly the TUNEL technique to label fragmented DNA (6–8). Additional studies in animals show that apoptosis-regulating proteins are predominantly expressed in the proliferative and hypertrophic zones with an increase of proapoptotic factors by age (7,9). Others have questioned apoptosis as the final mechanism through which chondrocytes die in the terminal hypertrophic zone. Ahmed et al.(10) hypothesized nonapoptotical mechanisms to be involved and described morphologic changes distinct from classical apoptosis. In addition, Roach and Erenpreisa (11) re-examined microscopic pictures of hypertrophic chondrocytes of in vitro cultured chick growth plates and hypothesized that terminal hypertrophic chondrocytes die not only through apoptosis but also through transdifferentiation to endochondral osteoblasts. In later studies, Roach and Clarke(12,13) studied rabbit growth plates and described chondrocytes with condensed chromatin, suggestive of apoptosis, but the “morphology of the cytosol” was unlike that of necrotic, apoptotic, or normal cells. In 2004, they came up with the name chondroptosis instead of apoptosis to describe the appearance of these cells (14). This study reported autophagic vacuoles in the chondroptotic cells, suggesting a role for autophagy in the process of cell death of the terminal hypertrophic cell. Autophagy and autophagosomes were also observed in avian hypertrophic chondrocytes and in chondrocytes of newborn mice (15,16).
Previous studies focusing on the fate of growth plate chondrocytes have been performed mostly in different animal models. It is uncertain whether the chick growth plate is comparable with the human, and studies in rodents are limited by the fact that growth plate fusion does not occur during sexual maturation in rats and mice. The only studies done in human tissues are not very extensive involving TUNEL analyses performed in spinal growth plates and slipped capital femoral epiphysis growth plates (6,17,18). To resolve this issue, we decided to jointly collect human growth plate tissue samples obtained during epiphyseal surgery performed in children at different stages of development. When analyzing all these samples of human growth plate tissues, we were lucky to discover that in one of the patients, a 17-y-old late pubertal female, the growth plate was captured just when it was in the process of undergoing epiphyseal fusion. This growth plate tissue can be considered as unique because epiphyseal fusion is a rapid process that is extremely difficult to capture. This specific human tissue specimen is therefore like a snapshot of epiphyseal fusion and could help us to better understand how growth plate fusion occurs and the underlying mechanisms involved. Using these tissues, we here aimed to describe the morphologic characteristics of a fusing human growth plate and possible mechanisms involved in the process of human epiphyseal fusion and discuss these in relation to previous published data obtained in different animal models.
METHODS
Patients and tissue preparation.
Human proximal and distal femur growth plate tissues were collected from 14 girls and five boys at different pubertal stages who were undergoing surgery for different medical indications (Table 1). The study protocol was approved by the Local Medical Ethics Committees of The Leiden University Center, Leiden, the Netherlands, and The Karolinska University Hospital, Stockholm, Sweden. Informed consent was obtained from all patients and their parents. No patient used any continuous medication. Patient 13, the patient with a growth plate in the process of epiphyseal fusion, was mostly wheelchair bound and mentally retarded. Because of frequent painful hip luxations hip replacement surgery was performed. Figure 1 shows an x-ray of her right hip where a complete luxation can be observed. All tissue samples were processed in the same way. Specimens were immediately fixed in 10% formaldehyde overnight, decalcified in 10% EDTA for 5 d, and then embedded in paraffin.
Immunohistochemistry.
Immunohistochemistry was performed as previously described (19) with the following modifications. After antigen retrieval by incubating with trypsin (Invitrogen) for 10 min at 37°C, the sections were additionally treated with 5 mg/mL hyaluronidase (Sigma Chemical Co.-Aldrich, Inc, Steinheim, Germany) for 30 min at 37°C. Anti-Collagen-X antibody was from Quartett (Berlin, Germany) and used in a 1:100 dilution. Anti-Bcl-2 antibody was from Upstate (#06-474 Upstate Biotechnology, Lake Placid, NY) and used in a 1:300 dilution. AntiBax antibody (P19) and antiBad antibody (C-20) were purchased from Santa Cruz Inc., (Santa Cruz Biotechnology, Inc., Santa Cruz, CA) and, respectively, used in a 1:300 and 1:200 dilution. Anti-Bcl-XL antibody was purchased from Transduction Laboratories (Becton Dickinson AB, Stockholm, Sweden) and used in a 1:100 dilution. Anti-cleaved-caspase three primary antibody was purchased from Cell Signaling Technology (In Vitro Sweden AB, Stockholm, Sweden) and used in a 1:50 dilution. Secondary anti-rabbit biotinilated antibody (Jackson Immunoresearch lab, West Grove, PA) or anti-mouse biotinilated antibody (DAKO, Glostrup, Denmark) were, respectively, used in a 1:1000 and 1:300 dilution, followed by incubation with avidin-biotin Vectastain ABC reagent according to manufactures instructions (Vector laboratories, Burlingame, CA). Digital images were collected us ing a Nicon Eclipse E800 microscope equipped with an Olympus DP70 digital camera.
Apoptosis assay (TUNEL).
Apoptotic cells were identified by TUNEL immunohistochemistry according to instructions for the TdT-FragEL DNA fragmentation kit (Oncogene Research, Boston, MA) with the following modifications. The sections were treated with 5 μg/mL proteinase K for 15 min (20–22). Control experiments showed that when pretreating sections with distilled water instead of TdT, all cells were negative, whereas pretreatment with DNase enabled labeling of all cells.
Tartrate-resistant acid phosphatase (TRACP) staining.
TRACP staining was performed using a combination of solutions that include naphtol–AS BI phosphate, dimethylformamide, tartaric acid, acetate buffer, vermoal buffer, sodium nitrite, and pararoseaniline pH 5.2. Tissue sections were deparaffinized, rehydrated, and incubated with the reactive solution for 30 min as described in detail previously (23). After washing with distilled water, the tissue sections were counterstained with Mayer's hematoxylin.
Transmission electron microscopy.
Small tissue pieces were cut out from blocks of paraffin embedded bone/cartilage tissue and the paraffin was dissolved in xylene at 60°C. The tissue was rehydrated in alcohol into distilled water and fixed in 2% glutaraldehyde + 0.5% paraformaldehyde in 0.1 M sodiumcacodylate buffer containing 0.1 M sucrose and 3 mM CaCl2, pH 7.4, 24 h at 4°C. Specimens were rinsed in 0.15 M sodiumcacodylate buffer containing 3 mM CaCl2, pH 7.4 postfixed in 2% osmium tetroxide in 0.07 M sodiumcacodylate buffer containing 1.5 mM CaCl2, pH 7.4 at 4°C for 2 h, dehydrated in ethanol followed by acetone and embedded in LX-112 (Ladd, Burlington, VT). Semithin sections were cut and stained with toluidine blue and used for light microscopic analysis. Ultrathin section were cut and contrasted with uranyl acetate followed by lead citrate and examined in a Tecnai 10 transmission electron microscope at 80 kV. Digital images were captured by a MegaView III digital camera (Soft Imaging System, GmbH, Münster, Germany).
RESULTS
Light microscopy.
Figure 2A and C show representative pictures of an early pubertal female growth plate (patient 4) at 40× (A) and 100× (C) magnification. Figure 2B and D show pictures of the late pubertal patient (patient 13) with ongoing fusion of her growth plate stained with H&E at, respectively, 40× and 100× magnification. As expected, early pubertal growth plate chondrocytes were found to be organized in parallel columns maturing from resting to proliferative and then to large hypertrophic cells. In the late pubertal patient, growth plate remnants were found at the site where in less mature bones the epiphyseal plate is located. These remnants were small and surrounded by dense cortical-like bone. Chondrocytes within these growth plate remnants were disorganized and no columns could be found. In addition, the cells were very large with big lacunae and some of them were fused together. To study in more detail the interface of the fusing growth plate, immunohistochemistry for collagen type X and TRACP staining were performed. The unfused growth plates showed expectedly positive staining for collagen type X in the hypertrophic zone (Fig. 2E). However, surprisingly, the growth plate remnant with large hypertrophic-like cells did not show any positive staining (Fig. 2F). TRACP staining, a marker for osteoclasts, was seen at the chondro-osseus junction of prepubertal growth plates (Fig. 2G) and in early pubertal growth plates (data not shown). However, at the interface of the growth plate remnant, no TRACP staining could be detected (Fig. 2H).
H&E staining of sectioned human growth plates. In early pubertal patients, growth plate chondrocytes were organized in parallel columns (patient 4; panel A 40× and panel C 100 × magnification). In a late pubertal patient, the growth plate was diminished to a small remnant surrounded by dense cortical-like bone (patient 13; panel B 40× and panel D 100× magnification). All unfused growth plates stained positive for collagen type X in the hypertrophic zone (patient 2; panel E 100× magnification), whereas the fusing growth plate did not show any staining (patient 13; panel F 100 × magnification). Panel G, shows positive TRACP staining in an early pubertal growth plate, indicated by arrows (patient 2, 100× magnification), whereas the fusing growth plate stained negative (patient 13; panel H 100× magnification). Bars in all figures indicate 200 μm.
Transmission electron microscopy.
To allow comparative electron microscopic studies of cell death characteristics, small pieces were cut out from paraffin blocks containing growth plate tissues from the patient with ongoing epiphyseal fusion. For comparative analysis, three younger pubertal female growth plates (patients 4, 9, and 11) were processed in a similar way.
The fusing growth plate was found to be entirely surrounded by a border of very dense, cortical-like bone clearly isolating the growth plate from any vessels or osteoclasts (Fig. 3F). In contrast, in nonfusing growth plates, there was a small distinct border between loosely packed collagen type II in the cartilage matrix and collagen type I in the bone matrix (Fig. 3E). Collagen type I contains thick fibers compared with the very thin collagen type II fibers and therefore these two types of collagen could easily be distinguished. There were no signs of classical apoptosis in the fusing growth plate; e.g. no apoptotic bodies or patched chromatin and proteins could be found (Fig. 3B and D). In addition, no typical signs of inflammation were found although we did observe some signs of early necrosis like empty vacuoles (see arrows Fig. 3B). In addition, we observed signs of hypoxia, e.g. patchy distributed chromatin and defect plasma cell membranes. No double-membrane autophagosomes, like typically seen in cells undergoing autophagy, were found in the fusing growth plate.
TEM images from the proximal femur epiphyseal growth plate in a mid-pubertal patient (patient 9; left panels, A, C, and E) and the late pubertal patient with a fusing growth plate (patient 13; right panels B, D, and F). In the midpubertal patient, hypertrophic zone chondrocytes displayed a normal morphology (A) and at a higher magnification, dense chromatin was found in the cell nucleus (C). In contrast, the fusing growth plate displayed a patchy chromatin pattern (B and D). At high-power magnifications of the interphase between cartilage and bone matrix, a distinct border between loosely packed cartilage matrix collagen type II (Coll-II) and bone matrix collagen type I (Coll-I) was found in the midpubertal patient (E), whereas in the fusing growth plate, the border was thicker and the bone matrix collagen type I more dense (F). Bars: A and B, 5 μm; C and D, 2 μm; E and F, 1 μm.
In early-pubertal and mid-pubertal growth plates (Fig. 3A and C), we observed normal chondrocytes with nonpyknotic nuclei containing homogenous dense chromatin without signs of DNA fragmentation. We specifically focused on the terminal hypertrophic chondrocytes that were about to be incorporated into the newly formed bone. In these cells, some chromatin condensation was seen, but this was clearly different from what normally is seen in cells undergoing classical apoptosis. Cell membranes were intact and the cytoplasm mostly empty. No autophagosomes could be found and no sign of necrosis was present.
TUNEL analysis.
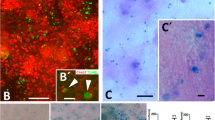
In all female (two prepubertal and 12 pubertal) and male (five pubertal) subjects, very few growth plate chondrocytes stained positive or showed an apoptotic-like morphology when applying the TUNEL method (Fig. 4A). The staining intensity was scored (0 to 3 points; 0 indicating no staining and 3 indicating many positive cells throughout the growth plate), and the results are shown in Table 1, ranked according to pubertal stages. It is important to point out that when evaluated by experienced scientists in the field, most TUNEL-positive cells indeed were considered to have a viable appearance, as indicated by a complete absence of apoptosis-related morphologic changes, and should therefore be considered as nonspecifically stained. In the fusing growth plate, no single TUNEL-positive cell was detected (Fig. 4B). In contrast, the surrounding bone marrow was abundantly stained with the TUNEL technique and could therefore serve as an internal positive control as previously described (21,24). Negative controls showed no staining.
TUNEL and immunohistochemistry staining of prepubertal, pubertal, and fusing growth plates (100× and inserts 200× magnification). Panel A, TUNEL analysis patient 4, left insert showing positive cells in surrounding bone marrow. Panel B, TUNEL analysis fusing growth plate (patient 13). Panels C and D, Bcl-2 staining patient 4 and fusing growth plate. Panels E and F, Bcl-XL staining patient 10 and fusing growth plate. Panels G and H, Bax staining patient 4 and fusing growth plate. Panels I and J, Bad staining patient 3 and fusing growth plate. Panels K and L, cleaved caspase-3 patient 3 and fusing growth plate. Bars indicate 100 μm.
Antiapoptotic proteins.
Bcl-2 staining was detected in cells throughout the whole growth plate in patients with nonfused growth plates (n = 4, Table 1) (Fig. 4C). When the relative staining intensity was scored (score 0 to 3), a possible tendency toward increased expression was found during maturation (Table 1). The fusing growth plate did show some staining for Bcl-2 (score 2; Fig. 4D).
Bcl-XL, another antiapoptotic factor, was also localized in cells throughout the whole growth plate (n = 6, Table 1, Fig. 4E). No change in percentage positive cells or staining intensity was seen during maturation. In addition, in the fusing growth plate some cells stained positive for Bcl-XL (score 2; Fig. 4F).
Proapoptotic proteins and caspase 3.
Staining for Bax, a proapoptotic factor, was seen in chondrocytes throughout the whole growth plate (n = 5, Table 1, Fig. 4G). No change in staining intensity or percentage Bax positive cells was seen during pubertal development. Interestingly, in the fusing growth plate no staining for Bax could be detected (Fig. 4H).
Staining for Bad, another proapopotic factor, was found throughout the whole growth plate (n = 5, Table 1, Fig. 4I). No change in staining intensity or percentage of positive cells was seen during development. Some staining for Bad proteins was observed in the fusing growth plate (score 2; Fig. 4J), unfortunately with abundant background staining.
Cleaved caspase 3, an effector caspase in the apoptotic cascade, was seen throughout the whole growth plate in all pubertal stages (n = 8, Table 1) with no change during maturation (Fig. 4K). In the fusing growth plate, no staining for cleaved caspase 3 was detected (Fig. 4L).
Negative controls showed no staining for all analyzed pro- and antiapoptotic proteins.
DISCUSSION
On the basis of well-established morphologic and histologic criteria of apoptosis, we could not detect any signs of classical apoptosis in human terminal hypertrophic growth plate chondrocytes. These findings were also confirmed by electron microscopy (EM). In a unique tissue specimen of a late pubertal fusing human growth plate, we found clear evidence that chondrocyte apoptosis is not likely to be involved in the end phase of growth plate fusion in humans. In contrast, signs of hypoxia and early necrosis were present in the fusing growth plate.
This is the first detailed study of apoptosis in the human pubertal growth plate that includes expression levels of pro- and antiapoptotic proteins together with morphologic analysis based on light and EM. Our study includes the characterization of a unique tissue sample from a growth plate in the process of undergoing fusion where we made the novel observation that the chondrocytes were markedly enlarged, disorganized, and surrounded by a border of dense, cortical-like bone. No morphologic signs of classical apoptosis were found in this fusing growth plate. Our findings are in agreement with earlier studies describing terminal hypertrophic zone chondrocytes at the chondro-osseous junction to have a morphology, which is not typically seen in cells undergoing classical apoptosis (11,14,25,26). However, it is important to point out that all these previous studies were performed in animal growth plates; avians or rodents that do not fuse their growth plates by the end of sexual maturation.
The mechanism by which terminal hypertrophic chondrocytes disappear during endochondral ossification is believed to be related to the underlying cause of eventual growth plate fusion. However, these two events involving the epiphyseal growth plate might as well be two different and independent processes. In this article, we compared both. Interestingly, we found some signs of early apoptosis and also some signs of necrosis such as empty vacuoles in the fusing growth plate, suggesting that fusing growth plate chondrocytes appear in a sort of intermittent stage between apoptosis and necrosis. Importantly, no signs of inflammation were observed around the fusing growth plate. Erenpreisa and Roach (26) also reported signs of necrosis in dark chondrocytes of the embryonic chick growth plate, however, such dark chondrocytes were not found in our human growth plate tissue samples. To our knowledge, no other signs of necrosis have previously been reported in the growth plate. Interestingly, Shapiro et al.(16) has reported that the morphology of terminal hypertrophic chondrocytes suggest autophagy, a type II programmed cell death, to occur in the growth plate. However, we did not see any double membrane structures like autophagosomes suggestive for autophagy but only vesicles with a single membrane that we interpreted as vacuoles.
Apoptosis is the most widely accepted and described mode of cell death through which terminal hypertrophic chondrocytes disappear and are replaced by bone (27). Most studies relay on TUNEL technique only, which often overestimates the number of apoptotic nuclei, as it labels not only fragmented DNA but also DNA in the process replication and repair. In many studies, TUNEL positive chondrocytes were observed not only in the hypertrophic layer where cells are assumed to die before being incorporated into the newly formed bone, but also in all zones of the growth plate (6,17,18). When re-evaluating pictures of growth plate chondrocytes positive for TUNEL staining, a high diversity of results could be found. Cell morphology is not always complementing TUNEL positivity and when data are presented, cells often do not look like cells in the process of undergoing apoptosis, but as healthy viable cells without showing signs of cell shrinkage and pyknotic nuclei (6,17,18). Thus, the TUNEL method is very sensitive, requires precise temporal control of each step (28) and must be verified by other techniques like EM or molecular markers of apoptosis.
Molecular markers of apoptosis include cleavage of caspases and often regulation of pro- and antiapoptotic proteins of the Bcl-2 family (29). In this study, we are the first to investigate these proteins in the human postnatal growth plate and we found that they are indeed expressed throughout the whole growth plate. We did not observe any caspase-3 cleavage, the effector caspase of apoptosis in the fusing growth plate. Moreover, in the fusing growth plate, we observed clear expression of the antiapoptotic proteins Bcl-2 and Bcl-XL and a possible down-regulation of the proapoptotic protein Bax. Thus, all three approaches including TUNEL technique, analysis of cell morphology by EM, and molecular markers by immunohistochemistry altogether suggest that there is no classical apoptosis occurring in the fusing human growth plate.
A novel and clear observation was that the fusing human growth plate is surrounded by a border of very dense thick bone, shelling the growth plate remnant. There are no vessels seen in or surrounding the fusing growth plate. Moreover, there were some signs of hypoxia in the fusing growth plate like patchy distributed chromatin. From these findings, one can hypothesize that this border of dense bone is functioning as a physical barrier for oxygen and nutrients to reach the fusing growth plate resulting in hypoxia and eventually cell death in a nonclassical apoptotic way through necrosis or a mixture of apoptosis and necrosis. White et al.(30) recently demonstrated by light microscopy bridging bone in the center of a distal human tibial growth plate obtained from a 12-y-old and 11-mo-old girl, which might be an early sign of this shelling process.
A limitation of this study is the relatively small number of growth plates that were analyzed and the fact that some were derived from pathologic conditions. To some extent, this is compensated by the fact that we were fortunate to obtain a tissue sample from a human growth plate just in the rapid process of undergoing epiphyseal fusion, which allowed us to investigate possible underlying mechanisms. In addition, the underlying mechanism of epiphyseal maturation and fusion will be the same for all growth plates regardless of the underlying disease of each patient because eventually longitudinal growth stopped in all patients by the end of puberty. When performing EM, the gold standard in cell death research, we found no clear signs of classical apoptosis in any of the human growth plates studied including the fusing one. It should be mentioned that fixation was not performed in the optimal way for EM. However, membranes were not disrupted in the way one would expect if tissue damage had occurred secondary to fixation problems. Furthermore, all tissues were processed in the same way, and there were clear differences in chromatin pattern and collagen fibers, which were nicely preserved.
In summary, a unique piece of fusing human growth plate tissue clearly demonstrate that classical apoptosis is not likely to be involved in the process of human growth plate fusion. We found signs suggestive for hypoxia and necrosis, but the exact mechanism through which chondrocytes disappear during epiphyseal fusion in humans still needs to be defined.
Abbreviations
- TEM:
-
transmission electron microscopy
- TRACP:
-
tartrate-resistant acid phosphatase
References
Hunziker EB 1994 Mechanism of longitudinal bone growth and its regulation by growth plate chondrocytes. Microsc Res Tech 28: 505–519
Kronenberg HM 2003 Developmental regulation of the growth plate. Nature 423: 332–336
Cohen JJ 1993 Apoptosis. Immunol Today 14: 126–130
Zimmermann KC, Green DR 2001 How cells die: apoptosis pathways. J Allergy Clin Immunol 108: S99–S103
Kroemer G, Martin SJ 2005 Caspase-independent cell death. Nat Med 11: 725–730
Adamczyk MJ, Weiner DS, Nugent A, McBurney D, Horton WE Jr 2005 Increased chondrocyte apoptosis in growth plates from children with slipped capital femoral epiphysis. J Pediatr Orthop 25: 440–444
Chrysis D, Nilsson O, Ritzen EM, Savendahl L 2002 Apoptosis is developmentally regulated in rat growth plate. Endocrine 18: 271–278
Smink JJ, Gresnigt MG, Hamers N, Koedam JA, Berger R, Buul-Offers SC 2003 Short-term glucocorticoid treatment of prepubertal mice decreases growth and IGF-I expression in the growth plate. J Endocrinol 177: 381–388
Wang Y, Toury R, Hauchecorne M, Balmain N 1997 Expression of Bcl-2 protein in the epiphyseal plate cartilage and trabecular bone of growing rats. Histochem Cell Biol 108: 45–55
Ahmed YA, Tatarczuch L, Pagel CN, Davies HM, Mirams M, Mackie EJ 2007 Physiological death of hypertrophic chondrocytes. Osteoarthritis Cartilage 15: 575–586
Roach HI, Erenpreisa J 1996 The phenotypic switch from chondrocytes to bone-forming cells involves asymmetric cell division and apoptosis. Connect Tissue Res 35: 85–91
Roach HI, Clarke NM 1999 “Cell paralysis” as an intermediate stage in the programmed cell death of epiphyseal chondrocytes during development. J Bone Miner Res 14: 1367–1378
Roach HI, Clarke NM 2000 Physiological cell death of chondrocytes in vivo is not confined to apoptosis. New observations on the mammalian growth plate. J Bone Joint Surg Br 82: 601–613
Roach HI, Aigner T, Kouri JB 2004 Chondroptosis: a variant of apoptotic cell death in chondrocytes?. Apoptosis 9: 265–277
Settembre C, Arteaga-Solis E, McKee MD, de Pablo R, Al Awqati Q, Ballabio A, Karsenty G 2008 Proteoglycan desulfation determines the efficiency of chondrocyte autophagy and the extent of FGF signaling during endochondral ossification. Genes Dev 22: 2645–2650
Shapiro IM, Adams CS, Freeman T, Srinivas V 2005 Fate of the hypertrophic chondrocyte: microenvironmental perspectives on apoptosis and survival in the epiphyseal growth plate. Birth Defects Res C Embryo Today 75: 330–339
Wang S, Qiu Y, Zhu Z, Ma Z, Xia C, Zhu F 2007 Histomorphological study of the spinal growth plates from the convex side and the concave side in adolescent idiopathic scoliosis. J Orthop Surg 2: 19
Zhu F, Qiu Y, Yeung HY, Lee KM, Cheng JC 2006 Histomorphometric study of the spinal growth plates in idiopathic scoliosis and congenital scoliosis. Pediatr Int 48: 591–598
Nilsson O, Chrysis D, Pajulo O, Boman A, Holst M, Rubinstein J, Martin RE, Savendahl L 2003 Localization of estrogen receptors-alpha and -beta and androgen receptor in the human growth plate at different pubertal stages. J Endocrinol 177: 319–326
Chagin AS, Chrysis D, Takigawa M, Ritzen EM, Savendahl L 2006 Locally produced estrogen promotes fetal rat metatarsal bone growth; an effect mediated through increased chondrocyte proliferation and decreased apoptosis. J Endocrinol 188: 193–203
Chagin AS, Karimian E, Zaman F, Takigawa M, Chrysis D, Savendahl L 2007 Tamoxifen induces permanent growth arrest through selective induction of apoptosis in growth plate chondrocytes in cultured rat metatarsal bones. Bone 40: 1415–1424
Martensson K, Chrysis D, Savendahl L 2004 Interleukin-1beta and TNF-alpha act in synergy to inhibit longitudinal growth in fetal rat metatarsal bones. J Bone Miner Res 19: 1805–1812
van der Pluijm G, Most W, Van der Wee-Pals L, de Groot H, Papapoulos S, Lowik C 1991 Two distinct effects of recombinant human tumor necrosis factor-alpha on osteoclast development and subsequent resorption of mineralized matrix. Endocrinology 129: 1596–1604
Ramos F, Fuertes-Nunez M, Suarez-Vilela D, Fernandez-Lopez A 2002 What does apoptosis have to do with clinical features in myelodysplastic syndrome?. Haematologica 87: 381–391
Adams CS, Shapiro IM 2002 The fate of the terminally differentiated chondrocyte: evidence for microenvironmental regulation of chondrocyte apoptosis. Crit Rev Oral Biol Med 13: 465–473
Erenpreisa J, Roach HI 1998 Aberrant death in dark chondrocytes of the avian growth plate. Cell Death Differ 5: 60–66
Cetin E, Girsch W, Brand G, Thurnher D, Cetin EM, Trieb K 2004 Distinct expression of APO-1/Fas and caspase-8 in the human growth plate. Calcif Tissue Int 74: 181–186
Rohwer F, Azam F 2000 Detection of DNA damage in prokaryotes by terminal deoxyribonucleotide transferase-mediated dUTP nick end labeling. Appl Environ Microbiol 66: 1001–1006
Robertson JD, Orrenius S, Zhivotovsky B 2000 Review: nuclear events in apoptosis. J Struct Biol 129: 346–358
White JR, Wilsman NJ, Leiferman EM, Noonan KJ 2008 Histomorphometric analysis of an adolescent distal tibial physis prior to growth plate closure. J Child Orthop 2: 315–319
Acknowledgements
We thank the orthopaedic surgeons in the Leiden University Medical Center and at the Karolinska University Hospital in Stockholm for providing the growth plate samples.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by ZonMw (project 920-03-358) the Netherlands, the Swedish Research Council, and a visiting scholarship award from the European Society for Paediatric Endocrinology.
Rights and permissions
About this article
Cite this article
Emons, J., Chagin, A., Hultenby, K. et al. Epiphyseal Fusion in the Human Growth Plate Does not Involve Classical Apoptosis. Pediatr Res 66, 654–659 (2009). https://doi.org/10.1203/PDR.0b013e3181beaa8c
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181beaa8c
This article is cited by
-
The Origin and Fate of Chondrocytes: Cell Plasticity in Physiological Setting
Current Osteoporosis Reports (2023)
-
Postnatal skeletal growth is driven by the epiphyseal stem cell niche: potential implications to pediatrics
Pediatric Research (2020)
-
Necroptosis: Biochemical, Physiological and Pathological Aspects
Pathology & Oncology Research (2011)